Screening for Vertebral Artery Compromise in Patients with Benign Paroxysmal Positional Vertigo (BPPV)
Benign Paroxysmal Positional Vertigo (BPPV) and Fall Prevention in the Aging Population
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of dizziness, affecting approximately 30% of individuals over 60, with prevalence approaching 50% after age 85 (Balatsouras et al., 2018). Left untreated, such vestibular disorders significantly increase the risk of falls, which are the leading cause of injury-related extended hospitalization stays among Canadian seniors (Public Health Agency of Canada (PHAC, 2023). In 2018, falls accounted for 48% of all injury-related deaths among older adults in Canada (PHAC, 2023). In 2004, the direct costs associated with falls among seniors in Canada were estimated at over $2 billion (PHAC, 2022). Preventing falls through simple timely vestibular assessments and interventions can alleviate the pressure on the healthcare system (PHO, 2021).
The Importance of Vertebral Artery Screening Before BPPV Testing and Repositioning Maneuvers
BPPV can be effectively assessed by the Dix Hallpike and Supine Head Roll test at the bedside and then treated with canalith repositioning maneuvers, such as the Semont, Gans, Appiani, Gufoni, Lempert, Yacovino, and Epley maneuvers, among others. However, before performing these procedures, it is crucial to screen for vertebral artery compromise to prevent serious complications, including vertebrobasilar insufficiency (VBI) or a posterior circulation stroke (such as a basilar stroke). The importance of screening arises because certain head and neck movements, such as those performed during BPPV testing and treatment, can temporarily obstruct or reduce blood flow to the vertebrobasilar arteries. For patients at risk, this can trigger dangerous symptoms like dizziness, visual disturbances, and even a stroke. Patients with BPPV have approximately a 1.4-fold risk of ischemic strokes (Zalewski, 2015). Vertebral artery screening helps identify patients at risk, ensuring that diagnostic and therapeutic maneuvers for BPPV are conducted safely, mitigating risks, and sending a medical referral for VBI or posterior circulation stroke in a timely manner.
Why Vertebral Artery Screening is Essential
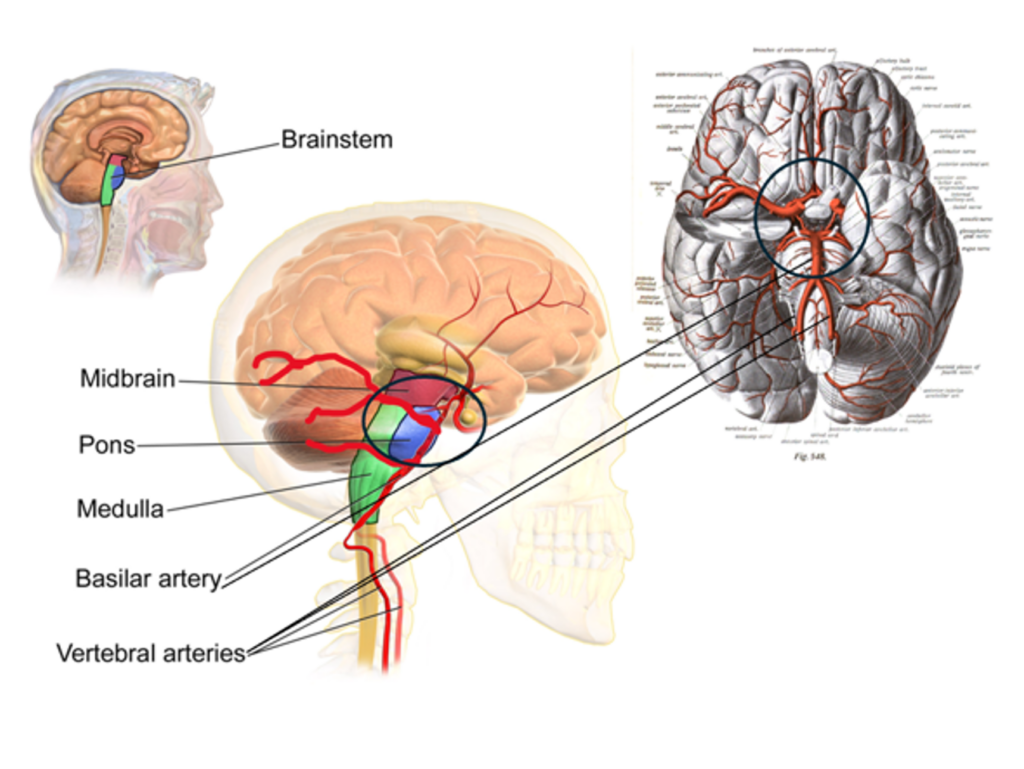
Vertebral artery screening is essential because it helps detect inadequate blood flow or ischemia through the vertebrobasilar arteries which supply crucial brain areas, including the cerebellum, medulla, midbrain, and occipital cortex. Blockage of the vertebrobasilar arteries can occur through atherosclerosis or an accumulation of emboli (deposits of cholesterol or calcium among others). Risk factors include hypertension, high blood pressure, diabetes mellitus, smoking, age, genetic factors, and high cholesterol. Ischemia of the vertebrobasilar circulation clinically presents as either a VBI or a stroke related to the cerebrum’s posterior circulation such as a basilar stroke (Pirau & Lui, 2023).
Screening for a Compromised Vertebral Artery before performing BPPV assessments helps to:
1. Differentiate Between BPPV and VBI As Causes of Dizziness.
BPPV results from dislodged otoconia entering the semicircular canals and typically presents with short-lasting rotary torsional with an up or down beating component or horizontal nystagmus along with vertigo (or a spinning sensation) lasting seconds to minutes, episodic postural instability, nausea, diaphoresis, and emesis typically evoked by specific movements. It is treated by canalith repositioning maneuvers, and symptoms resolve with 1-2 carefully executed maneuvers on average (The American Institute of Balance, 2024).
In contrast, VBI involves transitory ischemia of the vertebrobasilar circulation leading to dizziness, vertigo, headaches, double vision, slurred speech, difficulty swallowing, numbness/tingling, drop attacks, ataxia, imbalance, emesis, weakness in one or both sides of the body. Symptoms are transient and often triggered by head movements (e.g., looking up, turning head). They improve with rest or when the head returns to a neutral position. More than 60% of patients diagnosed with VBI have at least one episode of dizziness during the disease (Pirau & Lui, 2023). This condition warrants imaging and further medical evaluation by a physician. Distinguishing between these conditions is vital, as their management strategies differ significantly.
2. Avoid Posterior Circulation Stroke such as a Basilar Stroke
A posterior circulation stroke (e.g., basilar artery stroke) occurs when blood flow through the basilar artery to the brain is blocked or damaged, potentially damaging the brainstem and other critical areas. Symptoms include imbalance, vertigo, slurred speech, headache, nausea, and emesis among others. Symptoms are sudden, persistent, lasting for minutes to hours, worsening with time, worsening with head movement, and don’t improve with head turns to a neural position. This type of stroke is relatively uncommon but can result in severe outcomes, including locked-in syndrome or death. In this case, a visit to the ER for medical evaluation and imagining is imminent. Treatment in an outpatient facility is contraindicated.
3. Recommendations by the Canadian Academy of Audiology and the Medical Community at Large
Screening for vertebral artery compromise before BPPV-related procedures is recommended by The Canadian Academy of Audiology, The American Academy of Neurology, The American Academy of Otolaryngology–Head and Neck Surgery, and by the medical community at large (Canadian Academy of Audiology, 2017; Bhattacharyya et al., 2017; American Institute of Balance, 2024; Kiel & Hossain, 2017). This article will discuss the Vertebral Artery Screening test (VAST) and Head Impulse, Nystagmus, and Test of Skew (HINTS) used widely by the medical community.
How to Perform the Vertebral Artery Screening Test (VAST)
The VAST procedure as outlined by The American Institute of Balance is simple and can be performed in any clinical setting:
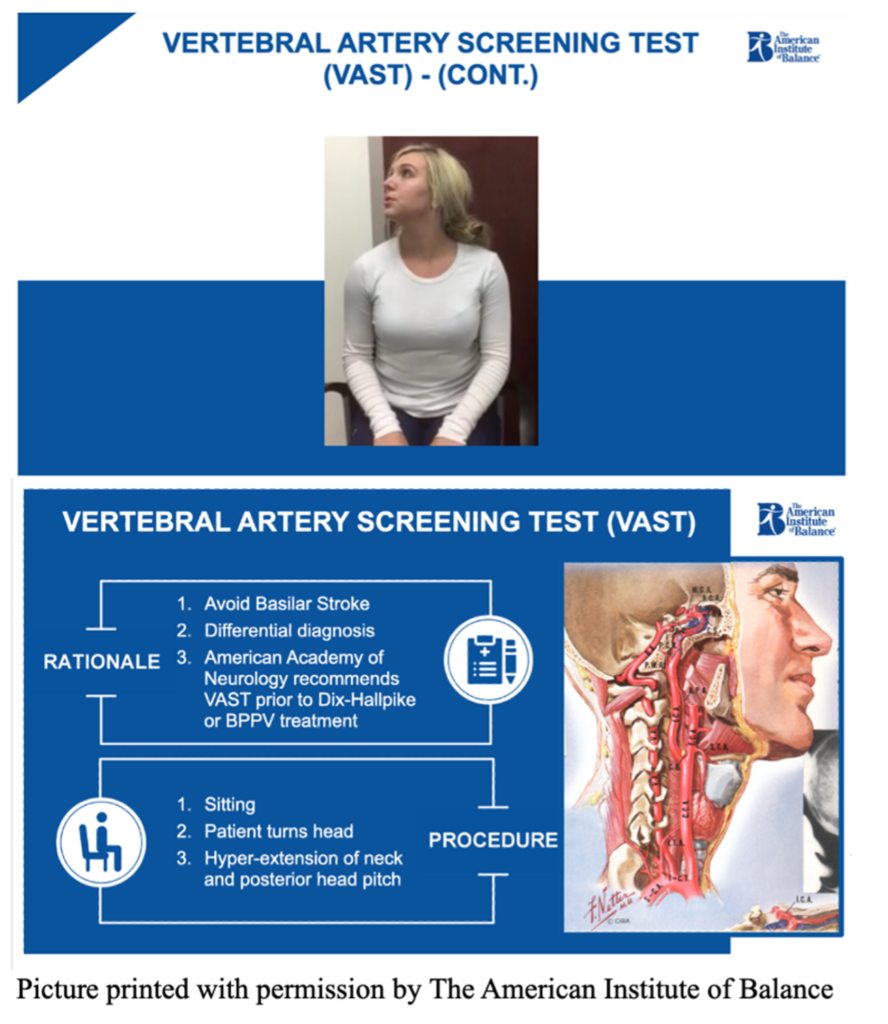
1. Position the Patient: The patient sits in a chair.
2. Head Movements:
- The patient turns their head to the right while looking up to the ceiling and holds this position for 20 - 30 seconds (while the health care provider monitors for symptoms while engaging them in general conversation)
- The patient turns their head to the left while looking up to the ceiling and holds this position for 20 – 30 seconds (while the health care provider monitors for symptoms while engaging them in general conversation)
4. Symptom Assessment
The clinician observes the patient for signs of vertebral artery compromise, particularly the 5 Ds and 3 Ns outlined below. It is important not to cue the patient with the 5 Ds and 3 Ns but rather ask open-ended questions, such as “How are you feeling in this position?”
Recognizing Vertebral Artery Compromise: The 5 Ds and 3 Ns
| THE 5 Ds | THE 3 Ns |
| Dizziness | Nystagmus – Rapid involuntary eye movements |
| Dysphagia – Difficulty swallowing | Potentially direction changing/vertical |
| Dysarthria – Difficulty speaking (slurred speech) | Numbness – facial or limb numbness |
| Diplopia – Double vision | Nausea |
| Drop Attacks – Sudden falls without syncope |
In individuals with vertebral artery compromise, the lateral rotation of the neck leads to mechanical occlusion of one or both vertebral arteries causing some or all the 5 D and 3 N symptoms for as long as they maintain the offending position (Saber Tehrani et al., 2018; Choi et al., 2005).
Interpreting VAST Results
- If the patient exhibits any of the 5 Ds or 3 Ns then the VAST is positive suggesting that either a VBI or stroke is possible, and they should be referred for further medical evaluation. Provocative tests like the Dix-Hallpike should be avoided until a physician gives clearance. Suppose a stroke is not likely and BPPV is suspected. In that case, clinicians can proceed with caution modifying the procedures to reduce stress on the cervical spine (e.g., using the side-lying test for posterior canal BPPV instead of the Dix-Hallpike test). A medical referral to a physician is still warranted for imaging and further work-up.
- If the patient exhibits no symptoms, BPPV testing and treatment can proceed as usual.
How to Perform the HINTS Screening Test
The HINTS exam is an evidence-based bedside tool widely used in the medical community for differentiating between central causes of vertigo (including VBI, basilar stroke, Wernicke’s encephalopathy, multiple sclerosis, cerebellar neoplasms etc.) and peripheral vestibular disorders like vestibular neuritis or labyrinthitis. It is has a sensitivity of 100% and specificity of 96% in identifying a stroke (Kattah et al, 2009; Newman-Toker, 2020). According to Kattah et al. (2009), the HINTS exam outperforms an MRI in detecting a stroke within the first two days of symptom presentation in patients with acute vestibular syndrome. A normal head impulse test with symptoms of vertigo, direction-changing nystagmus, or an abnormal test of skew strongly suggest a central pathology, warranting a medical referral for neuroimaging and workup. In contrast, an abnormal head impulse test with unidirectional nystagmus and no skew deviation is more indicative of a peripheral vestibular disorder. Given that vertebrobasilar strokes can mimic benign vertigo, incorporating the HINTS exam into clinical assessment enhances diagnostic accuracy and ensures timely intervention for life-threatening conditions (Kattah et al., 2009).
Conclusion
BPPV is prevalent in older adults and significantly increases the risk of falls, a major cause of mortality. Screening for vertebral artery insufficiency before BPPV assessment and treatment is essential to prevent serious complications, such as a posterior circulation stroke. The VAST helps identify at-risk patients, ensuring safe clinical procedures and timely medical referrals. Additionally, the HINTS exam is a valuable bedside evaluation for distinguishing between central and peripheral causes of vertigo, outperforming early MRI in detecting stroke. Implementing these screening protocols in clinical practice enhances patient safety, prevents misdiagnosis, and improves healthcare outcomes.
References
- The American Institute of Balance. (2024, December 4). Evaluation: Cervicogenic considerations. Presented at the Vestibular Assessment and Management Certification, Tampa, FL.
- Balatsouras, D. G., Koukoutsis, G., Ganelis, P., Korres, S., & Kaberos, A. (2018). Benign paroxysmal positional vertigo in the elderly: Current insights. Clinical Interventions in Aging, 13, 2251–2266. https://doi.org/10.2147/CIA.S151926
- Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngology–Head and Neck Surgery. 2017;156(3_suppl): S1-S47. doi:10.1177/0194599816689667
- Blausen Medical Communications. (n.d.). Brainstem anatomy [Illustration]. Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Blausen_0114_BrainstemAnatomy.png
- Canadian Academy of Audiology. (2017). Vestibular assessment & management for Canadian audiologists: A scoping review. https://canadianaudiology.ca/wp-content/uploads/2017/05/Vestibular_Scope_Review_EN.pdf
- Choi, K. D., Shin, H. Y., Kim, J. S., Kim, S. H., Kwon, O. K., Koo, J. W., et al. (2005). Rotational vertebral artery syndrome: Oculographic analysis of nystagmus. Neurology, 65(8), 1287–1290. https://doi.org/10.1212/01.wnl.0000180405.00560.51
- Kattah, J. C., Talkad, A. V., Wang, D. Z., Hsieh, Y. H., & Newman-Toker, D. E. (2009). HINTS to diagnose stroke in the acute vestibular syndrome: Three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke, 40(11), 3504–3510. https://doi.org/10.1161/strokeaha.109.551234
- Newman-Toker, D. E., Kerber, K. A., Hsieh, Y.-H., Pula, J. H., Omron, R., Saber Tehrani, A. S., Mantokoudis, G., Hanley, D. F., Zee, D. S., & Kattah, J. C. (2013). HINTS outperforms ABCD2 to screen for stroke in acute continuous vertigo and dizziness. Academic Emergency Medicine, 20(10), 986–996.
- https://doi.org/10.1111/acem.12223
- Kiel, D. M., & Hossain, M. (2017). Diagnosis and management of benign paroxysmal positional vertigo. American Family Physician, 95(3), 154-161. Retrieved from https://www.aafp.org/pubs/afp/issues/2017/0201/p154.html
- Pirau, L., & Lui, F. (2023). Vertebrobasilar insufficiency. In StatPearls (2025 Jan-). StatPearls Publishing. Retrieved March 15, 2025, from https://www.ncbi.nlm.nih.gov/books/NBK482259/
- Public Health Agency of Canada. (2022). Seniors and falls: Statistics and facts. Retrieved from https://www.canada.ca/en/public-health/services/publications/health-risks-safety/seniors-falls.html
- Public Health Agency of Canada. (2023). Surveillance report on falls among older adults in Canada. Retrieved from https://www.canada.ca/en/public-health/services/publications/healthy-living/surveillance-report-falls-older-adults-canada.html
- Public Health Agency of Canada. (2023). Seniors’ falls in Canada: Second report. Retrieved from https://www.canada.ca/en/public-health/services/publications/healthy-living/seniors-falls-canada-second-report.html
- Public Health Ontario. (2021). Falls among older adults in Ontario: A report on emergency department visits, hospitalizations, and mortality. Retrieved from https://www.publichealthontario.ca
- Saber Tehrani, A. S., Kattah, J. C., Kerber, K. A., Gold, D. R., Zee, D. S., Urrutia, V. C., & Newman-Toker, D. E. (2018). Diagnosing stroke in acute dizziness and vertigo: Pitfalls and pearls. Stroke, 49(3), 788–795.
- Sobo, S. (1909). Illustration of the blood-brain barrier [Image]. Wikimedia Commons. https://commons.m.wikimedia.org/wiki/File:Sobo_1909_3_548.png
- Zalewski, C. K. (2015). Aging of the human vestibular system. Frontiers in Aging Neuroscience, 6, 108. https://doi.org/10.3389/fnagi.2014.00108

