When Positional Vertigo is Not “Benign”
From: When Positional Vertigo is Not “Benign” | The Hearing Review
Used with permission. Hearing Review

Benign paroxysmal positional vertigo (BPPV) is the No. 1 cause of vertigo. Except when it’s actually not the cause. Vertebral artery compromise can mimic BPPV and should always be considered in cases of “atypical” BPPV.
By Richard E. Gans, PhD
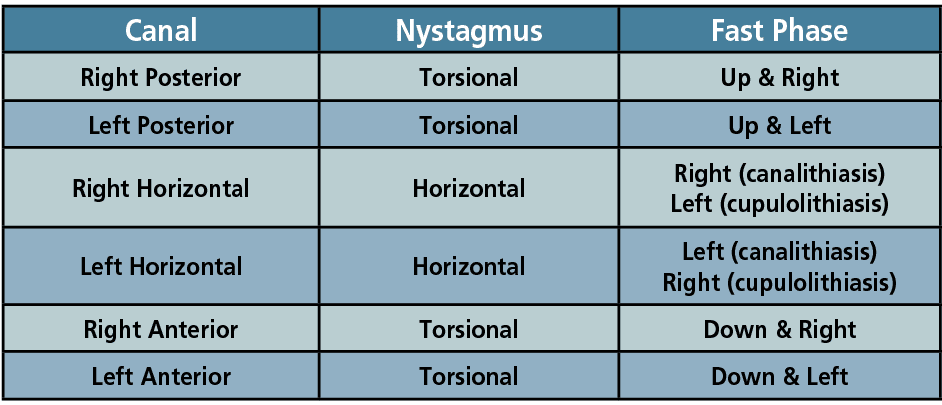
Practitioners specializing in dizziness and balance disorders have become very familiar with patients complaining of positional vertigo, and the vast majority of the time it is related to a posterior canal BPPV.1 This applies to attending staff within walk-in clinics and hospital emergency departments (ED) as well. In fact, BPPV is so prevalent it is estimated that 50% of all individuals will experience at least one occurrence by age 70.2 This all-too-common condition has unfortunately caused practitioners at times to become jaded, to the point that when there is a non-classic case it may erroneously be labeled as an “atypical” BPPV. Roberts and Gans (2008)3 have published specific nystagmus patterns for involvement of each of the semi-circular canals affected, as shown in Table 1.
Further exacerbating this situation during a bedside positioning protocol, most commonly a classic Hallpike, is the hyperextension and rotation of the neck to the side being tested. This mechanical position places stress on the cervical spine so that if there is any cervical stenosis, spur, osteoarthritis, or congenital malformation, it potentially may cause compromise or even dissection of the vertebral artery (VA). Numerous investigators4,5 have published extensively on the benefit of using a modified Hallpike (mHallpike) or hybrid method, which may include the use of side-laying or other modifications to reduce such risks due to extreme hyperextension with rotation of the neck. This author has recommended the vertebral artery screening test (VAST) be included in all evaluations and pre-treatment for BPPV as well as in numerous publications and textbook chapters for over 30 years.
What is Vertebral Artery (VA) Compromise?
The VA consists of major arteries in the neck. Its anatomy arises from the subclavian artery at C 5 and C 6 and moves superiorly up through C2. The arteries comprising the VA are very thin and are tortuous at the superior portion. It enters the cranium through the foramen magnum where it joins together with the contralateral VA to form the basilar artery. An anatomical representation is shown in Figure 1, including a left VA dissection and subsequent repair. These arteries carry oxygen-rich blood to the brainstem and cerebellum. Any mechanical compression or tear in the walls can cause neurologic symptoms. Conditions can range from a compromise of blood flow to a complete dissection of the artery.

Why is a Vertebral Artery Screening Test Recommended?
The VAST is a simple bedside exam that may be performed with the patient seated or supine. Its purpose is to test the vertebral artery blood flow. It is not 100% sensitive but has been recommended by numerous investigators and white papers to be included in any vestibular evaluation. The symptoms of VA compromise are always of a neurologic nature and are clearly distinguishable from those seen with cervicogenic dizziness and BPPV.
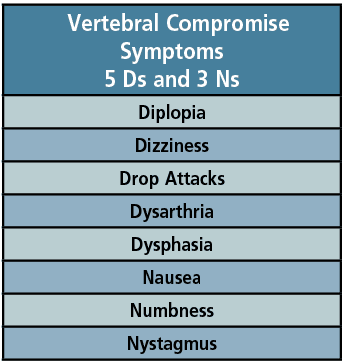
The VAST protocol has been well-described in detail.6 While seated, the patient rotates their head and then hyperextends their neck. This rotation first, prior to hyperextension, is to ensure that if there is any spur it would not dissect the VA. This position should be held for about 20-30 seconds. The patient will only rotate and hyperextend within their acceptable range of motion. In patients who have undergone a cervical spine fusion, the VAST should likely be withheld. The patient is questioned for the appearance of any of the symptoms (5 Ds and 3 Ns) outlined in Table 2. The patient should reply out loud so any dysarthria can be noted. The patient then moves back down into a neutral position. Symptoms could also occur when they return to the neutral position. The procedure is then repeated in the opposite direction. If it is determined the patient is positive for VA compromise, it is imperative when testing for posterior-canal-type BPPV (PC-BPPV) that traditional Hallpike placements be avoided, and alternative modifications such as side-laying be used.
Case Study
The following case study reflects a fairly common patient journey for those with undiagnosed VA compromise. These patients have typically not been evaluated, quickly released with a diagnosis of “atypical” BPPV, and then receive multiple canalith repositioning treatments. Not only do the treatments not eliminate the symptoms, but they in fact exacerbate them and could lead to stroke. VA dissection is the number one cause of stroke in young males.6
History
A normal, otherwise healthy 26-year-old male with unremarkable history of otologic or neurologic conditions experienced an acute onset of vertigo while playing golf. He was transported to ED of nearby hospital. CT scan without contrast was unremarkable and he was discharged from ED with a prescription for meclizine.
He was referred to the physical therapy (PT) department with a provisional diagnosis of benign paroxysmal positional vertigo (BPPV). He was treated multiple times on multiple visits with modified Epley maneuvers for “atypical” PC-BPPV. These did provoke a subjective report of dizziness and nausea with left Hallpike (neck extension and head rotation to the left), but no observable nystagmus. He was given Brandt-Daroff exercises to do at home on a daily basis. Patient reported increasingly severe symptoms while doing these exercises but without any improvement. On occasion the symptoms were so intense he needed several hours to recover.
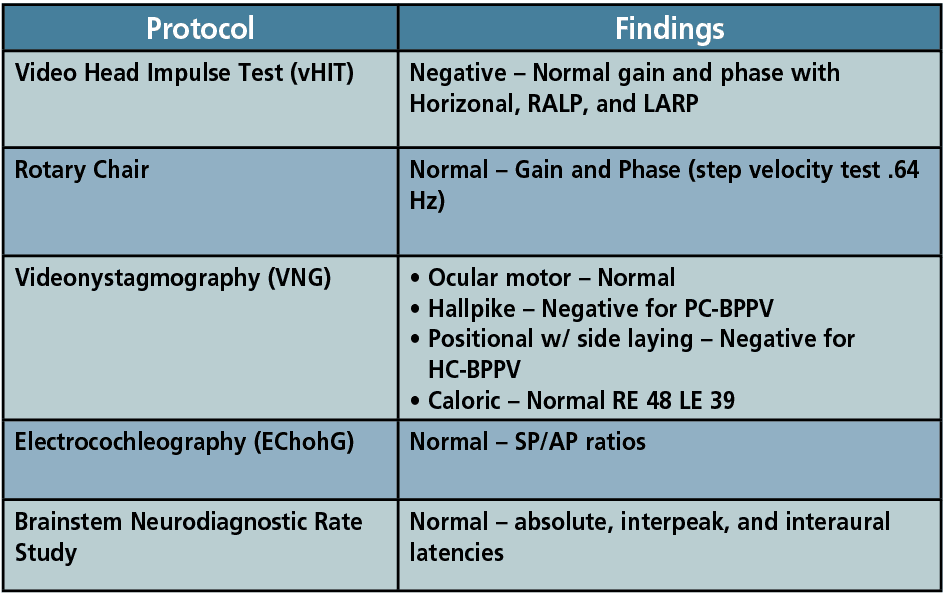
After four weeks of numerous recurrences and unsuccessful repositioning treatments to resolve the symptoms, the patient was subsequently referred to an ENT. Prior to this, no vestibular assessment had been recommended or performed. The sole assessment had been the CT scan at the hospital ED. The initial ENT exam was unremarkable with negative Hallpike (no nystagmus, no fatigue) but symptomatic for dizziness, nausea, and blurred vision with Hallpike to the left. Patient was then scheduled for comprehensive neurodiagnostic vestibular testing.
Clinical Findings and Recommendations
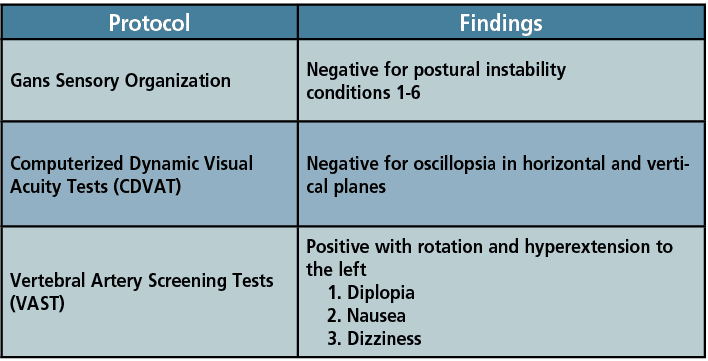
As can be seen in Table 3 and Table 4, the sole abnormality noted was the positive VAST with rotation and hyperextension to the left. All other tests were negative or unremarkable for a BPPV of either ear or any canal. Likewise, there were no indications of peripheral or central vestibular involvement or other neurological indicators. Also, no indicators for a chronic uncompensated vestibulopathy. The positive VAST finding indicated the need for neurological consultation with radiographic studies of the cervical spine and VA pathway.
There are a variety of symptoms which may occur with the VAST, as shown in Table 2. Patients need only exhibit one of the systems and usually do not present with most or all of the indicators. The side of the involvement may also not necessarily be the side of the head rotation. If it occurs unilateral to the rotation, the VA may be crimped. But if it occurs on the contralateral side, the VA may be stretched. So, one may think about what can happen to water flowing through a garden hose if it is either crimped or stretched. The symptoms will always be of a neurological origin as it causes compromise to the posterior circulation of the brain. If there is nystagmus, since it is of a central origin, it will not follow the principles of a unilateral peripheral vestibular condition.
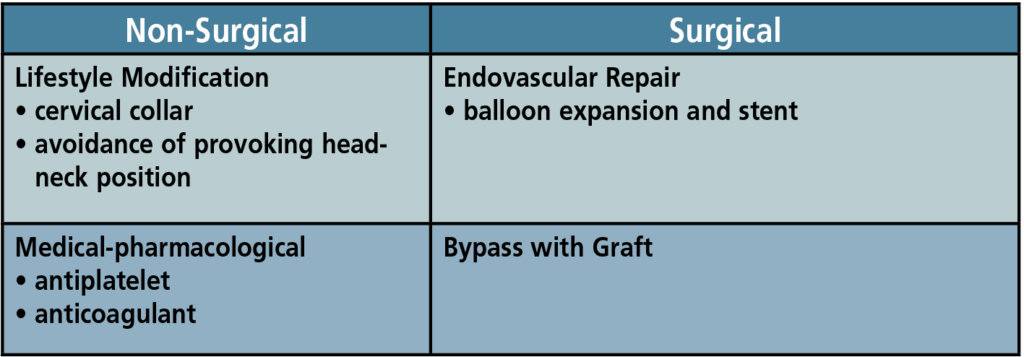
There are multiple treatment options for VA compromise, as shown in Table 5. These will be based on the radiographic studies, genesis of the condition, age, and medical status of the patient. The determination of which strategy to apply is complex and requires serious considerations based on the patient’s age, good health, and interest in an active lifestyle. In our case study, the patient and his physicians opted to have a stent placed within the left VA with ongoing medical and neurological follow-up and angiographic studies.
Summary
Despite the prevalence of BPPV in the general population, not all forms of positional vertigo can be attributed to BPPV. Practitioners are encouraged to be familiar with the gold standard of nystagmus patterns and symptoms seen in BPPV for all canals and should be conservative in their application of a diagnosis of “atypical” BPPV. This is critically important when patients have not undergone at least a VAST, had a full evaluation, present with central findings, or are unresponsive to multiple and diverse canalith repositioning. In keeping with the basic tenet of medicine attributed to Hippocrates, “First, do no harm.”
Richard E. Gans, PhD, is the founder and CEO of the American Institute of Balance (AIB). He is a research scientist member of the American Academy of Neurology, a scientific fellow member of the American Academy of Otolaryngology Head and Neck Surgery, and a past president of the American Academy of Audiology.
References
- Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1-S47. doi:10.1177/0194599816689667
- Figtree WVC, Menant JC, Chau AT, Hübner PP, Lord SR, Migliaccio AA. Prevalence of Vestibular Disorders in Independent People Over 50 That Experience Dizziness. Front Neurol.2021;12:658053. Published 2021 May 20. doi:10.3389/fneur.2021.658053 PMID: 34093406; PMCID: PMC8176523.
- Roberts R, Gans R. Background, technique, interpretation and usefulness of positional/positioning testing. In G. Jacobson & N. Shepard (Eds). Balance Function Assessment and Management. San Diego, CA: Plural Publishing; 2008.
- Roberts RA, Gans RE, Montaudo RL. Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2006;17(8):598-604. doi:10.3766/jaaa.17.8.6.
- Dispenza F, Kulamarva G, De Stefano A. Comparison of repositioning maneuvers for benign paroxysmal positional vertigo of posterior semicircular canal: advantages of hybrid maneuver. Am J Otolaryngol. 2012;33(5):528-532. doi:10.1016/j.amjoto.2011.12.002
- APTA. Cervical Arterial Dysfunction (CAD) Assessment (Vertebrobasilar Insufficiency (VBI) Test, Vertebral Artery Test (VAT), Neck Extension-Rotation Test). Available at: https://www.apta.org/patient-care/evidence-based-practice-resources/test-measures/cervical-arterial-dysfunction-cad-assessment-vertebrobasilar-insufficiency-vbi-test-vertebral-artery-test-vat-neck-extension-rotation-test

