Striking the Right Balance – Superior Canal Dehiscence Surgery: Did it Work?
Post-operative Audiovestibular Findings with Incomplete Plugging Surgery
Janine Verge, AuD, AuD(C) and Michael Vekasi, MClSc, RAud, Aud(C) will be coordinating the “Striking the Right Balance,” feature which will cover the latest information on “all things vestibular.”
In this edition of "Striking the Right Balance," Yvette Reid, audiologist at St. Paul's Hospital in Vancouver, BC, reviews three patient cases to look at the outcome of canal plugging surgery in the treatment of superior semicircular canal dehiscence. For this article, Yvette collaborated with Dr. Brian Westerberg, and Dr. Jane Lea, otolaryngologists with specialized training in otology & neurotology.
If you are a health care professional and would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by emailing JanineAllison.Verge@nshealth.ca to let us know that you want to be included. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
Superior semicircular canal dehiscence (SCD) is an absence of bone overlying the superior semicircular canal. SCD is typically characterized by aural fullness, sound-induced vertigo (Tullio phenomenon), pressure-induced vertigo, autophony and/or conductive hyperacusis.1 It is most often diagnosed with audiovestibular testing and imaging, typically a high-resolution temporal bone computed tomography (CT).2,3 An audiogram may show a pseudo-conductive hearing loss with supranormal bone conduction thresholds and an air-bone gap, normal tympanograms and present acoustic reflexes. Vestibular evoked myogenic potentials (VEMPs) will evoke an abnormally high-amplitude response and/or subthreshold response. SCD can be treated surgically by plugging the superior canal, which obliterates the function of that canal. Post-operatively, dizziness and balance dysfunction is expected temporarily. However persistent dizziness may suggest an incompletely filled canal.
The objective of this article is to review the audiovestibular assessment results obtained in three patients who had residual symptoms related to an incompletely plugged superior canal.
Patient 1
A 44-year-old woman presented with dizziness provoked by loud music and hearing her baby crying, as well as when sneezing and straining. She reported a sensation of constant motion, and of tipping to the left. She had a number of audiovestibular assessments from 2006 to 2011 at different hospitals. Her audiograms were negative for an air-bone gap but cervical VEMPs in 2009 and 2011 demonstrated a subthreshold response in the right ear. A temporal bone CT scan noted a near-dehiscence bilaterally. Oculomotor, caloric, positional, and positioning testing were all normal.
She underwent right transmastoid superior semicircular canal plugging surgery in 2012. Post-operatively she was still symptomatic. Repeat oculomotor and caloric testing were again normal. Video head impulse testing (vHIT) testing for the right anterior/superior (Note superior semicircular canal = anterior semicircular canal) canal was normal without the low gain and overt and/or covert saccades that would be expected for a plugged (i.e. nonfunctional) canal. The cVEMP threshold was abnormally low bilaterally. However, Dix-Hallpike testing to the right evoked an unexpected transient right torsional (i.e., counterclockwise) downbeat nystagmus, during which the patient reported vertigo. This result would normally suggest anterior/superior canal benign paroxysmal positional vertigo (BPPV), which seemed very unlikely. The more plausible explanation was that the canal plug was behaving like otoconia in the superior canal.
Magnetic resonance imaging (MRI) was performed as it provides better distinction than a CT scan between fluid and non-fluid material (i.e., between the canal’s perilymph and the plug), and was therefore used to evaluate the extent of the canal plugging. In this case the MRI confirmed that the right superior canal was incompletely filled and the patient underwent revision surgery, after which her symptoms improved considerably.
Patient 2
A 55-year-old woman presented with complaints of hearing loss and pressure in the left ear, dizziness in response to loud sound and “bouncing eyes” when jogging. She also noted that she could hear her heartbeat, eye and spine movements, and her voice seemed abnormally loud. She trialled a hearing aid in the left ear and found that it exacerbated her dizziness. An audiovestibular assessment in 2014 found a large air-bone gap in the left ear and subthreshold cVEMP responses bilaterally but particularly in the left ear. Oculomotor, caloric, positional and positioning tests were normal. A temporal bone CT scan noted bilateral superior canal dehiscence. She underwent left and right transmastoid superior canal plugging in May 2014 and in March 2015 respectively. Initially she reported feeling better, however a few months after the second surgery she reported a resurgence of her sound-induced dizziness, and a fullness in her left ear.
She returned for a vestibular assessment in January 2016. The vHIT was abnormal in both superior canals, as expected after plugging surgery. cVEMPs and oVEMPs were normal, which again was consistent with adequately plugged superior canals. However, Dix-Hallpike to both sides evoked persistent downbeating nystagmus, suggesting the canal plugs were presenting as anterior canal BPPV (cupulolithiasis variant). As in Patient 1, an MRI confirmed the persistent dehiscence on the left.
Patient 3
A 50-year-old man presented with complaints of conductive hypercusis and dizziness with loud sound. He reported that when he sang in his choir his vision would “twist” and that he could hear his heartbeat and his own voice abnormally loudly. An audiovestibular assessment in 2014 found an air-bone gap in the left ear with present acoustic reflexes, a subthreshold cVEMP response on the left and an asymmetrical oVEMP (50% asymmetry ratio). Oculomotor, caloric, positional and positioning tests were normal. During vHIT testing eye movement was delayed relative to head movement and the audiologist could see the eye movement stalling briefly partway through the eye movement. A temporal bone CT scan noted left superior canal dehiscence. He underwent left transmastoid superior canal plugging in September 2014. Post-operatively he continued to experience both sound-induced dizziness and autophony.
Audiovestibular testing was repeated in February 2015. The left cVEMP threshold was in the normal range and the superior canal vHIT was abnormal as expected post plugging surgery. Dix-Hallpike testing was normal; no downbeating nystagmus was seen. However, the air-bone gap was still present in the left ear. Surprisingly, the oVEMP response was absent on the left. An MRI indicated that the superior canal was inadequately plugged.
Results Summary
Table 1 summarizes the results for all three patients. The results that were unexpected for successful plugging surgery are in bold. Note that in Patient 2, Dix-Hallpike testing was the only vestibular test suggestive of incomplete plugging. In Patient 3, Dix-Hallpike testing was normal; however, the oVEMP was unexpectedly absent and the post-op MRI scan indicated that the anterior limb of the superior canal was completely plugged, suggesting the plug had been pushed toward the ampulated end of the superior canal potentially damaging the neuroepithelium of the superior canal. The absence of downbeating nystagmus in this patient may be attributed to destruction or injury to the ampulated end of the superior canal.
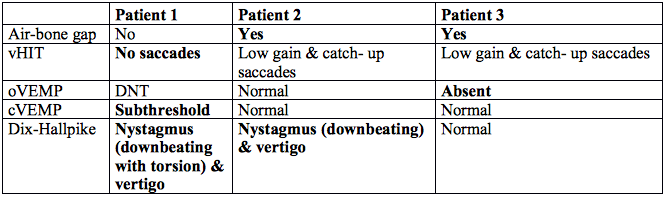
Table 1. Post-operative Results for SCD Plugging. Unexpected Results Are in Bold
Discussion
Patients with residual symptoms after plugging surgery for superior canal dehiscence and downbeat nystagmus in Dix-Hallpike testing may require an MRI scan to assess for a persistent dehiscence. Although downbeat nystagmus (with or without torsion) in Dix-Hallpike testing can indicate central nervous system (CNS) disease,4 absence prior to surgery as well as a lack of CNS features makes this unlikely. It is more probable that the downbeat nystagmus in the first two patients is secondary to incomplete plugging of the canal, whereby the surgically placed canal plugs behave like otoconia and result is symptoms and signs similar to anterior/superior canal BPPV.
Further study is warranted to determine if Dix-Hallpike testing is sensitive enough to use as a screening tool for an incompletely filled dehiscent canal. However, the results outlined suggest that an audiogram and cVEMP (the conventional assessments for superior canal dehiscence) are insufficient to evaluate the success of plugging surgery, and that the patient should undergo a more complete audiovestibular assessment, including Dix-Hallpike and vHIT testing.
References
- Minor L, Solomon D, Zinreich J, and Zee D. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg 1998;124(3):249–58.
- Carey JP, Minor LB, Nager GT. Dehiscence or thinning of bone overlying the superior semicircular canal in a temporal bone survey. Arch Otolaryngol Head Neck Surg 2000;126(2):137–47.
- Rosengren SM, Aw ST, Halmagyi GM, et al. Ocular vestibular evoked myogenic potentials in superior canal dehiscence. 2008;79(5):559–68. Epub 2007 Aug 31.
- Bertholon P, Bronstein AM, Davies RA, et al. Positional down beating nystagmus in 50 patients: Cerebellar disorders and possible anterior semicircular canalithiasis. J Neurol Neurosurg Psychiatr 2002;72(3):366–72.

