What Is a Hearing Care Outcome? Rethinking Measurement Through Trust, Agency, and Identity
1. Introduction: What Counts as an Outcome?
In audiology, we often treat outcomes as endpoints. We test, we fit, we measure, and we move on. Outcomes are usually presented as stable, objective snapshots of change: an improved QuickSIN score, a ticked-off COSI goal, a positive IOI-HA response. But what if we’ve misunderstood the very nature of what an outcome is? What if outcomes reflect not only measurable change, but also the lived integration of that change into a person’s identity and daily life?
This article revisits how we define and evaluate success in hearing care. While traditional audiological metrics are helpful, they are incomplete. A richer model must acknowledge the dynamic, lived, and relational nature of hearing rehabilitation. It must account for how people engage with care, how they adapt their lives, and how they come to see hearing help as part of who they are. In short, we need to expand our understanding of outcomes from "what works" to "what fits, endures, and empowers."
2. Current Practice: How We Measure Hearing Care Outcomes
The field of audiology is replete with outcome measures. Objective tests such as speech-in-noise assessments (e.g., QuickSIN, HINT, DIN) capture performance in controlled listening conditions (Killion et al., 2004; Nilsson et al., 1994). Subjective tools such as the APHAB (Cox & Alexander, 1995), SSQ (Gatehouse & Noble, 2004), HHIE (Ventry & Weinstein, 1982), and IOI-HA (Cox et al., 2000) offer insight into self-perceived difficulty, satisfaction, and benefit. More individualized instruments like the COSI (Dillon et al., 1997) and Goal Attainment Scaling (Turner-Stokes, 2009) attempt to bridge the gap between clinical goals and lived priorities.
These tools have contributed significantly to evidence-based care. But they are limited by their assumptions. They assume that outcomes are:
- Static (i.e., measured at fixed points)
- Individual (rather than relational or contextual)
- Quantifiable (often reducing complexity to a numerical score)
Moreover, we frequently debate the relative merits of clinician-driven vs. patient-reported outcomes. While important, this debate overlooks a deeper issue: are we measuring the right things at all?
3. What Outcomes Miss: The Human Foundations
In many cases, people disengage from hearing care not because of poor technology or audiological failure, but because something more fundamental is missing. We propose three under-measured outcomes that underpin the success of all others:
- Trust: The degree to which a person feels safe, respected, and understood within the hearing care process (Hall et al., 2001).
- Agency: The sense of control, choice, and ownership a person has over their decisions and actions (Bandura, 2001).
- Identity Coherence: The alignment between the hearing care journey and the person's self-concept, values, and life roles (Oris et al., 2016).
These are not "soft" outcomes. They are scaffolds for every other outcome. Without trust, the person won't disclose their struggles honestly. Without agency, they won't follow through. Without identity coherence, they may reject care even if it is effective.
These constructs are not abstract ideals; they are measurable, actionable, and increasingly supported by validated tools. Trust in healthcare providers has been operationalized through psychometrically sound instruments such as the Trust in Physician Scale (Anderson & Dedrick, 1990), which captures interpersonal trust within the patient-provider relationship, and the Wake Forest Trust Scales (Hall et al., 2002), which broaden this lens to include institutional trust in the healthcare system as a whole. Agency, a critical factor in health behavior and outcomes, can be indexed using the Patient Activation Measure (PAM) (Hibbard et al., 2004), which assesses an individual’s knowledge, skill, and confidence in managing their health across four empirically defined levels of activation. Identity coherence, though a newer concept in hearing healthcare, is gaining traction through emerging tools rooted in chronic illness identity frameworks, such as the Illness Identity Questionnaire developed by Oris et al. (2016), which articulates how individuals integrate (or resist integrating) a health condition into their self-concept. These frameworks provide not only theoretical grounding but also practical pathways for clinical assessment and intervention. In short, we are not constrained by a lack of imagination—we are simply in the early stages of applying these constructs meaningfully within audiological care.
4. The Problem of Static Outcomes: Beechey & Naylor (2025)
One of the most profound critiques of current outcome thinking comes from Beechey and Naylor (2025), who argue that most clinical outcomes assume people are passive responders to context. In reality, people are active shapers of their environments. They move through life adjusting, avoiding, reconfiguring, and reinterpreting their contexts to maintain meaning and function.
For example, a person who stops going to noisy restaurants due to hearing loss has not simply failed to improve—they've adapted their environment. A measurement model that cannot accommodate this kind of change risks mislabeling adaptive behavior as clinical failure.
Beechey and Naylor call for outcome models that are dynamic and modulatable—ones that reflect a person's evolving relationship to their environment, not just their function within a static one. In hearing care, this means recognizing not only what people can do in controlled conditions, but how they reshape their lives to preserve connection, dignity, and coherence.
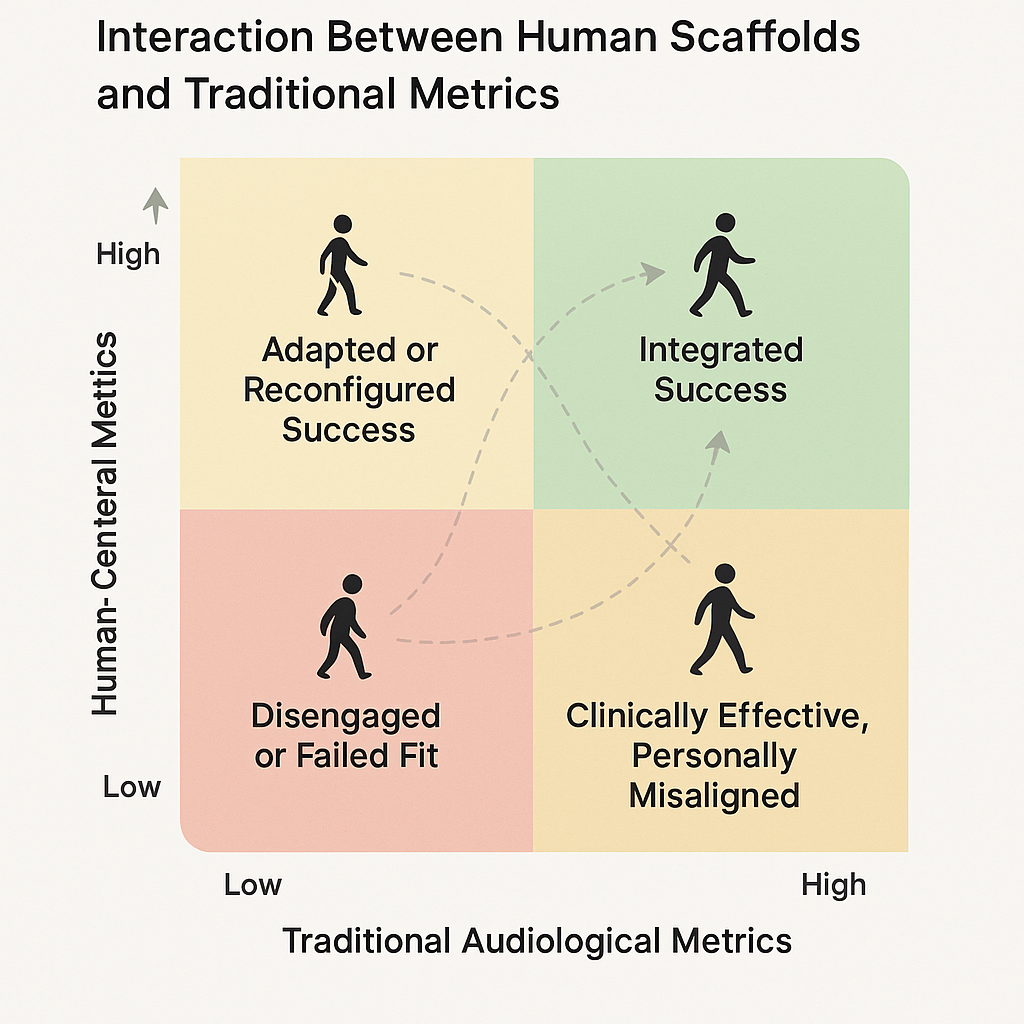
This quadrant model illustrates how clinical outcomes in hearing care emerge from the interplay between measurable audiological performance (horizontal axis) and foundational human constructs—trust, agency, and identity coherence (vertical axis). Each quadrant represents a distinct outcome profile, from disengagement to integrated success, highlighting that high clinical scores alone do not guarantee meaningful or sustainable change. Movement across quadrants reflects potential patient trajectories, emphasizing the need for both technical and relational alignment in care.
5. Behavior as the Endgame: COM-B and Real-World Change
The COM-B model (Michie et al., 2011) offers a framework for understanding behavior as a function of:
- Capability (knowledge, skills)
- Opportunity (environmental and social support)
- Motivation (internal drive, meaning)
Trust, agency, and identity coherence map elegantly onto these:
- Trust enhances opportunity by creating relational safety.
- Agency supports capability by instilling confidence and control.
- Identity coherence fuels motivation by making hearing care meaningful.
Together, these scaffolds do more than enable action—they sustain it. COM-B reminds us that outcomes should not just be measures of change, but reflections of durable behavior embedded in real life.
6. A New Integrated Model of Hearing Outcomes
We propose a four-layer model for outcome thinking:
- Audiological Metrics (e.g., speech-in-noise, COSI goals, IOI-HA ratings)
- Human-Centered Scaffolds (trust, agency, identity coherence)
- Behavioral Integration (use, communication changes, relational impacts)
- Contextual Modifiability (a person’s ability to reshape their environment)
This model reframes outcomes as dynamic, layered, and person-driven. Traditional tools remain vital, but they must be interpreted within the context of these deeper, more flexible dimensions.
Clinicians might begin by asking new questions: What parts of your life have changed because of your hearing? Where have you adjusted things? What still feels misaligned? These answers won’t fit on a Likert scale, but they will shape how we tailor support.
7. Conclusion: Redefining Success in Hearing Care
If we want to improve outcomes in hearing care, we must first redefine what an outcome is. It is not simply a test score or a satisfaction rating. It is the lived experience of continuity, autonomy, and connection in the presence of hearing difficulty.
By integrating trust, agency, identity coherence, and contextual modifiability into our framework, we move from a model of intervention delivery to one of person-centered transformation.
But redefining outcomes also means rethinking our practices. If coherence—not just acceptance—is the goal, then everything from intake to follow-up must be reshaped to reflect that. We may need to ask different questions, listen for different cues, and become comfortable with a less linear notion of progress. Outcome measures would not just track change—they would trace how a person reconfigures their world to stay connected, whole, and self-consistent.
And yes, someone will ask: isn’t this just acceptance by another name?
Here’s why it’s not.
Acceptance is a suitcase. You pack your hearing loss into something manageable. You carry it with you. It’s present, but external—something to work around.
Coherence is a skin graft. It fuses. It heals. It becomes part of the structure of who you are. You don’t carry it anymore. You become someone new because of it—seamlessly, and sometimes invisibly.
This is the difference between accommodating hearing loss and integrating it by using a device and becoming a different kind of listener.
Of course, identity coherence is not equally available to all. It's shaped by culture, community, trauma, and access to care. People who face structural barriers may not have the same opportunities to reconfigure their environment or feel safe integrating differences into their identity. Any future-facing outcome model must hold space for these inequities while still naming what good looks like.
And let’s not forget the clinician. Coherence is not just a patient outcome—it’s a professional imperative. Clinicians need supportive environments to practice with integrity, empathy, and presence. Otherwise, we risk asking them to deliver coherence while experiencing fragmentation themselves.
The future of hearing care will not be defined by better devices alone. It will be defined by whether we’ve built systems, relationships, and tools that help people hear—and stay whole.
References
- Anderson, L. A., & Dedrick, R. F. (1990). Development of the Trust in Physician Scale: A measure to assess interpersonal trust in patient–physician relationships. Psychological Reports, 67(3), 1091–1100.
- Bandura, A. (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology, 52, 1–26.
- Beechey, T., & Naylor, G. (2025). Dynamic outcomes in hearing healthcare: Toward a model of contextual modifiability. International Journal of Audiology, 64(2), 115-123. https://pubmed.ncbi.nlm.nih.gov/40091404/
- Charon, R. (2006). Narrative medicine: Honoring the stories of illness. Oxford University Press.
- Cox, R. M., & Alexander, G. C. (1995). The abbreviated profile of hearing aid benefit. Ear and Hearing, 16(2), 176–186.
- Cox, R. M., Alexander, G. C., & Beyer, C. M. (2000). Norms for the international outcome inventory for hearing aids. Journal of the American Academy of Audiology, 11(8), 419–426.
- Dillon, H., James, A., & Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology, 8(1), 27–43.
- Gatehouse, S., & Noble, W. (2004). The Speech, Spatial and Qualities of Hearing Scale (SSQ). International Journal of Audiology, 43(2), 85–99.
- Hall, M. A., Dugan, E., Zheng, B., & Mishra, A. K. (2001). Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? The Milbank Quarterly, 79(4), 613–639.
- Hibbard, J. H., Stockard, J., Mahoney, E. R., & Tusler, M. (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39(4p1), 1005–1026.
- Killion, M. C., Niquette, P. A., Gudmundsen, G. I., Revit, L. J., & Banerjee, S. (2004). Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. The Journal of the Acoustical Society of America, 116(4), 2395–2405.
- Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 42.
- Nilsson, M., Soli, S. D., & Sullivan, J. A. (1994). Development of the Hearing In Noise Test for the measurement of speech reception thresholds in quiet and in noise. The Journal of the Acoustical Society of America, 95(2), 1085–1099.
- Oris, L., Schrauwen, L., Rassart, J., Goubert, L., & Moons, P. (2016). Illness identity in adults with a chronic illness. Journal of Clinical Psychology in Medical Settings, 23(3), 265–276.
- Turner-Stokes, L. (2009). Goal attainment scaling (GAS) in rehabilitation: A practical guide. Clinical Rehabilitation, 23(4), 362–370.
- Ventry, I. M., & Weinstein, B. E. (1982). The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing, 3(3), 128–134.

