From Tinnitus to Musical Hallucinations: Navigating Complex Auditory Symptoms

Introduction
Auditory hallucinations, also known as paracusia, occur when the brain perceives sounds without any external source.1– 4 This condition is complex and often misunderstood, carrying significant implications for an individual’s well-being. The experiences associated with these hallucinations can vary widely, ranging from simple sounds—such as clicks or bells—to more elaborate perceptions like voices or music. The emergence of these phantom sounds is driven by intricate brain mechanisms, ultimately influencing individuals' responses.
While these hallucinations are frequently linked to psychotic disorders or substance use, they can also manifest in various contexts, including hearing loss, sensory deprivation, and neurological conditions.3– 6 For instance, patients with vestibular migraines may experience fleeting whispers or musical fragments as their symptoms progress. Similarly, older adults with a long-standing history of hearing loss, without any signs of mental health issues, may hear a familiar tune or melody from their past as if it is coming from their surroundings.
Moreover, it is important to differentiate auditory hallucinations from musical tinnitus—a term that often misrepresents the underlying mechanisms and the nature of the experience. Audiologists, often the first professionals to evaluate patients reporting these complex symptoms, must have a comprehensive understanding of auditory hallucinations, particularly musical ones, for accurate diagnosis and effective management.
Mapping Auditory Hallucinations: Classification Systems and Common Causes
The current literature on auditory hallucinations relevant to audiologists is limited, and no universally accepted classification system exists. In research, auditory hallucinations are generally classified based on the nature and content of the perceived sounds, and divided into two main categories: simple and complex forms.2– 4 Simple Auditory Hallucinations involve perceiving basic, non-verbal, and unstructured sounds such as clicks, bells, whistling or hissing, which can resemble tinnitus and may be challenging to differentiate from it.5,6 The distinction between these symptoms typically relies on identifying the underlying etiology or associated conditions. Complex Auditory Hallucinations involve perceiving intricate sounds such as music and voices. As for simple auditory hallucinations, they can be perceived either unilaterally or bilaterally, and may seem to originate either from inside the head or from the external environment. Let’s first look at auditory hallucinations involving the perception of music.5
Musical Hallucinations (MH), also called Musical Ear Syndrome, are characterized by the perception of melodies and songs without any external source.2,3,5,8–10 Unlike simple auditory hallucinations, MH often presents as well-defined and detailed musical experiences that are often familiar to the individual.3,7 These hallucinations can include many sounds, including beloved tunes from childhood like nursery rhymes, folk songs, church hymns, and even commercial jingles. Many patients also report hearing instrumental harmonies, rhythmic patterns, and distorted sounds similar to an out-of-tune radio station. Their duration and intensity can vary, with some individuals experiencing brief episodes, while others report chronic, persistent symptoms that are typically perceived as intrusive and distressing.5,11
MH needs to be distinguished from earworms and musical imagery. Earworms are catchy fragments of songs that involuntarily repeat in the mind but eventually fade, while musical imagery involves the intentional and conscious recall of music. Both phenomena are common and considered part of normal human experience in the general population.10– 13 Moseley et al., conducted a survey to differentiate these auditory experiences. Their findings indicated that MH are less frequent than earworms and characterized by minimal lyrical content. Additionally, musicians may underreport their MH due to their training and familiarity with musical imagery, making it difficult for them to differentiate between voluntary imagery and involuntary hallucinations.
The most common cause of MH is significant and progressive hearing loss and sensory deprivation, particularly in older adults. However, it has also been documented in younger individuals with conditions such as otosclerosis, where symptoms subsided following successful surgical intervention and improvement in hearing.8,14,15 A similar phenomenon occurs in the visual domain, known by vision care professionals as Charles Bonnet syndrome, which involves simple to complex visual hallucinations in older adults with substantial vision loss.19 MH can be classified into two main categories:
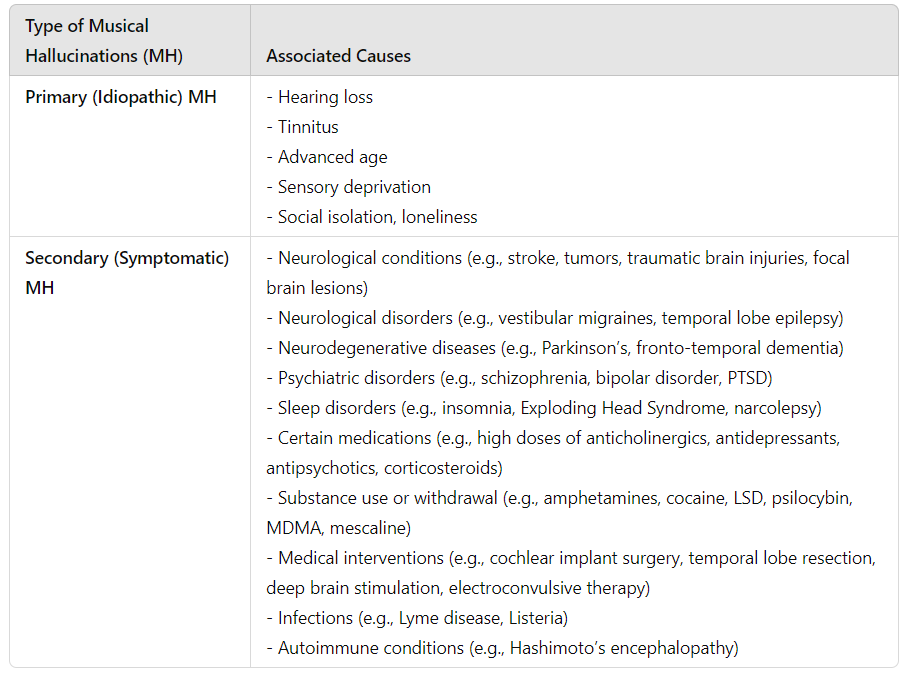
- Primary (Idiopathic) MH: These occur without a specific underlying cause and may be associated with risk factors such as hearing loss, tinnitus, sensory deprivation, advanced age, and social isolation/loneliness.4,5,7,8,15,16
- Secondary (Symptomatic) MH: These hallucinations are often linked to identifiable conditions such as traumatic brain injury, stroke, neurological disorders (e.g., vestibular migraines, temporal lobe epilepsy), neurodegenerative conditions, infections, and autoimmune conditions.2,3,7,18 Although less common, these hallucinations can also be associated with psychiatric disorders (e.g., schizophrenia, bipolar disorder), sleep disorders, medications affecting the central nervous system, and substance use or withdrawal.7,13 Additionally, they may occur due to medical interventions, including cochlear implant surgery and deep brain stimulation.5,6,17,20 For a comprehensive overview of these associated causes, please refer to Figure 2.
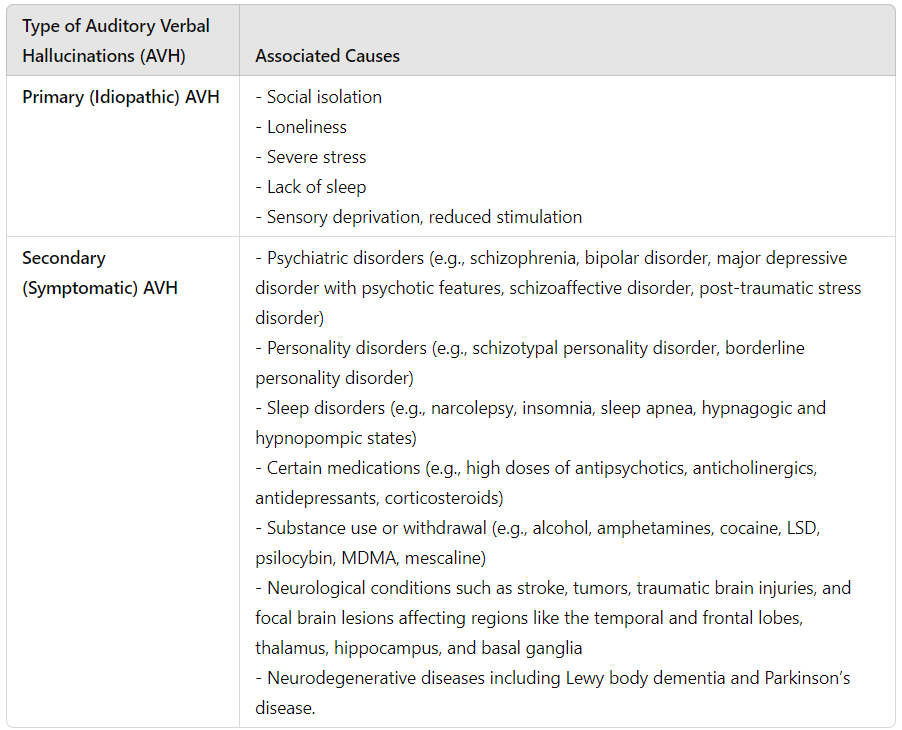
Auditory Verbal Hallucinations (AVH) are characterized by the perception of spoken words, speech, voices, or conversations without any external source1,2,21, 22, 23, 24. AVH can be both familiar and unfamiliar, with some individuals hearing recognizable voices, such as those of friends or family, while others encounter entirely new voices. The nature and content of these hallucinations can vary widely, ranging from brief fragments of speech to more elaborate interactions, including voices that converse with, comment on, or command the individual. Like MH, AVH can vary significantly in severity, but are debilitating for most affected individuals.21,23
These hallucinations are most commonly linked to psychiatric disorders, including schizophrenia, bipolar disorder, mood disorders, personality disorders, post-traumatic stress disorder, and sleep disorders.1,23,25,26 They can also occur in substance-related conditions, both during use and withdrawal, particularly with hallucinogens (e.g., LSD, psilocybin) and stimulants (e.g., amphetamines, cocaine). Although less frequent, AVH are also reported in neurodegenerative diseases such as advanced-stage Lewy body dementia and Parkinson’s disease-related delirium, where they are often regarded as cornerstone symptoms of the condition.16,27,28 For a comprehensive list of associated causes, refer to Figure 3.
Auditory hallucinations can be understood as existing on a continuum, ranging from everyday perceptual experiences (e.g., earworms, musical imagery) to conditions like tinnitus and more complex clinical issues like MH and AVH.10,24 This perspective also highlights that, although tinnitus and MH are commonly linked to hearing loss and AVH to psychiatric conditions, all three can occur in the same patient or in succession. This overlap indicates that these symptoms may exist along a spectrum rather than as distinct categories.29,32 Although classifying auditory hallucinations as either psychiatric or non-psychiatric may oversimplify the issue, this distinction can still help clinicians make appropriate referrals.
Epidemiological Insights: Understanding the Prevalence of Auditory Hallucinations
Auditory hallucinations, including MH and AVH, are more common than often recognized. Epidemiological studies suggest that 10-15% of the general population may experience occasional auditory hallucinations.5,30,33 Among these, AVH are significantly more prevalent than MH, especially in psychiatric conditions, with 75% of individuals with schizophrenia and 40% of those with PTSD.25,31 It is hypothesized that MH are less reported and documented than AVH due to factors such as limited awareness, unclear definitions, and a predominant focus on AVH in clinical and research settings.33
A comprehensive observational study by Linszen et al., found that MH and AVH are prevalent among older adults with hearing loss, particularly those with severe deficits. The study revealed that 16.2% of individuals with hearing loss experienced auditory hallucinations in the past four weeks, increasing to 24% in those with severe hearing loss, compared to 5.8% in those without hearing loss. Additionally, 80.6% of those with auditory hallucinations also experienced tinnitus, compared to 70.3% in those without hallucinations. Finally, auditory hallucinations, including both MH and AVH, are reported more frequently by females, with an overall female-to-male ratio of approximately 2:1. The reasons for this gender difference remain unclear.4,5
Comparative Clinical Presentations of MH and Tinnitus
Musical hallucinations (MH) and tinnitus often co-occur and can both be triggered by risk factors such as advanced age, hearing loss, and sensory deprivation. Due to their high prevalence among individuals with MH, some researchers posit a link between tinnitus and the development of these hallucinations. However, both conditions differ significantly in their cognitive and emotional impacts and their implications for diagnosis and treatment. Tinnitus is generally experienced as a persistent, simple, and often unfamiliar internal sound, while MH are characterized by complex, often familiar music or songs perceived as coming from the environment. While 15–20% of individuals with tinnitus report bothersome symptoms that can affect their quality of life, most individuals with MH face distress, fear, and embarrassment, as these hallucinations often challenge their sense of reality.3,13,34–36 Due to concerns about stigma, many individuals with MH may feel reluctant to disclose their experiences. As Oliver Sacks insightfully describes in Musicophilia: Tales of Music and the Brain37:
“People with musical hallucinations will often search for an external source—a radio, a neighbor’s television, or a band in the street—and only when they fail to find any such external source do they realize that the source must be within themselves. They might describe it as a tape recorder, a jukebox, or an iPod in the brain—something autonomous with its own will, not felt to be a controllable, integral part of the self. The existence of such phenomena in one’s head can evoke bewilderment and, not infrequently, fear. There is often concern that one might be going mad, or that the phantom music could signal a serious underlying condition such as a tumor, stroke, or dementia. Such fears often inhibit people from acknowledging their hallucinations; this reluctance may partly explain why MH have long been considered rare, though it is now understood that this is not the case.”
Neural Mechanisms behind MH: A Complex Symphony of Brain Activity
The exact neural mechanisms underlying MH in older adults with long-standing hearing loss and no psychiatric abnormalities remain poorly understood. However, it is widely recognized that hearing loss and sensory deprivation are significant risk factors, particularly in that population.8,38,39 Prolonged hearing loss initiates a cascade of neurophysiological changes that impact both auditory processing and cognitive function.40,41 As the brain is exposed to repeated and diminished auditory input, it undergoes maladaptive changes—such as the reorganization of neural pathways and alterations in cortical thickness—that can result in the perception of phantom sounds, including music.42,43 In the absence of external sounds, the brain compensates by increasing activity not only in auditory processing areas, such as the superior temporal cortex, but also in regions linked to memory, attention, and emotional regulation, including the hippocampus, amygdala, and prefrontal cortex.11 This overcompensation engages stored musical memories to fill the gap, leading to the generation of “phantom” music.
Although an extensive body of research has examined auditory verbal hallucinations (AVH) associated with psychiatric conditions, there has been comparatively less focus on the neural mechanisms underlying MH in individuals with hearing loss, particularly through neuroimaging techniques.9,11,44–48 Studies employing Positron Emission Tomography (PET) and functional Magnetic Resonance Imaging (fMRI) have provided key insights into the brains of those experiencing MH, confirming the specific regions activated during these events. As illustrated in Figure 4, findings indicate increased metabolic activity and enhanced connectivity in areas such as the prefrontal, medial, and superior temporal cortex, which are critical for memory and auditory processing.46 Research further reveals an overlap between the brain regions involved in music perception and those activated during MH, suggesting that shared neural pathways may underlie both experiences. In contrast, AVH engage distinct circuits related to speech and language processing, including Broca’s area, Heschl’s gyrus, and Wernicke’s area.30,49,50 Studies indicate that, in musically untrained individuals, the brain’s right hemisphere is typically more active during musical processing, in contrast to musicians, who tend to show greater engagement in the left hemisphere.48,51,52 This shift suggests that musicians may process music similarly to language, utilizing analytical and syntactical aspects, as both music and speech share cognitive and neural resources.53–55

In addition to hearing loss and sensory deprivation, structural brain lesions can contribute to MH by disrupting normal auditory processing 5,7,51,56. Lesions resulting from stroke or traumatic brain injury can cause localized damage in critical brain regions, such as the auditory cortex, hippocampus, and amygdala. This damage affects the brain’s ability to process and interpret auditory information accurately, potentially leading to the generation of phantom music.
In neurodegenerative diseases like Parkinson’s disease, MH can occur, although they are less common than visual or AVH and may present alongside symptoms such as delirium.27,28 Parkinson’s disease is characterized by abnormal protein deposits known as Lewy bodies in brain regions related to motor control and cognition, leading to progressive motor dysfunction and cognitive decline, which can impact areas involved in auditory perception and memory. Delirium, an acute and reversible state of severe mental confusion, can occur in individuals with Parkinson’s due to various factors, including medication side effects, infections, or metabolic imbalances. This state can exacerbate sensory processing issues, contributing to the experience of MH.
Finally, neurological disorders such as vestibular migraines and temporal lobe epilepsy (TLE) are also associated with MH.57,58 Vestibular migraines involve complex brain function changes that lead to headaches, aura, and sensory disturbances, including transient MH caused by cortical spreading depression, which disrupts normal sensory processing. TLE, characterized by recurrent seizures and auras, often results in MH due to abnormal bouts of electrical activity affecting auditory processing in the temporal lobes.
Guidelines for Effective Assessment and Management of MH
Detailed Case History. Proper diagnosis of MH is based on a comprehensive history-taking.18,37,56,59 This should involve questions about the nature of the hallucinations, including whether they involve voices, melodies, songs, or non-verbal sounds and their origin—whether organic or related to psychiatric conditions. It is also important to inquire about associated symptoms and their progression. Are there early warning signs like an “aura” or postdrome symptoms such as headaches or fatigue as seen in vestibular migraines or TLE? Family history is also critical, especially regarding hearing loss, mental health conditions or dementia. Recent physical health, medications, or emotional status changes should also be explored. Gathering this information will help determine if a referral to a specialist, such as a neurologist, ENT, or psychiatrist, is needed for more precise diagnosis and treatment.
Audiological Evaluation. Given that long-term hearing loss is a major factor in MH, a comprehensive hearing evaluation is essential to determine the extent and impact of the loss. If hearing loss is identified, fitting and recommending hearing aids is a critical first step in managing MH.8,18,56,59–61
Hearing Aid Verification. For patients already using hearing aids, verifying the hearing aid output through real-ear measurements is essential, as sensory deprivation is a known risk and aggravating factor for MH. In many cases, patients with recent onset of MH may have hearing aids set below prescriptive gain targets, such as NAL-NL2. Ensuring optimal amplification can help mitigate the impact of MH. Additionally, patients may not be using their hearing aids as consistently as advised. Therefore, counselling on proper usage is critical to enhancing both hearing outcomes and symptom management.
Informational Counselling. Informational counselling plays a vital role in managing MH. Educating patients to help them understand and normalize their symptoms can effectively reduce stress and anxiety, and provide reassurance.33 This approach also promotes the development of more effective coping strategies.62,63 Given the likely bi-directional relationship between MH-related distress and mental well-being, poor mental health can intensify how patients perceive the severity of MH. Increased stress and feelings of annoyance, shame, and frustration may worsen concerns and distress about the symptoms and treatments. Helping patients understand this two-way relationship could lead to more effective management of their mental health and MH.62–64 Regular follow-up appointments are important for monitoring progress and adjusting the management plan as needed. If anxiety or depression persists, referring patients to a cognitive behavioral therapy specialist could be beneficial. Additionally, consulting with primary care physicians to explore medical treatments for managing stress and anxiety can further support patient care.
Sound Therapy. If MH persists despite appropriate hearing aid adjustments, sound therapy, similar to tinnitus management techniques, should be considered. This approach may involve sound enrichment strategies at home or sound therapy programs integrated into hearing aids. In a 2010 study by Yutaka and colleagues, AVH in two patients were significantly reduced within a month of sound therapy combined with medication, with no recurrence observed for 31 and 17 months, respectively.65
By addressing the various facets of MH, audiologists can offer more comprehensive care and ensure that patients receive the appropriate treatment and support for their conditions.
References
- American Psychiatric Association. (2014). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. https://doi.org/10.1176/appi.books.9780890425596
- Blom JD, Sommer IE. Auditory hallucinations: nomenclature and classification. Cogn Behav Neurol. 2010 Mar;23(1):55-62. doi: 10.1097/WNN.0b013e3181b2791e. PMID: 20299866.
- Berrios GE. Musical hallucinations. A historical and clinical study. Br J Psychiatry. 1990 Feb;156:188-94. doi: 10.1192/bjp.156.2.188. PMID: 2180526.
- Evers S, Ellger T. The clinical spectrum of musical hallucinations. J Neurol Sci. 2004 Dec 15;227(1):55-65. doi: 10.1016/j.jns.2004.08.004. PMID: 15546592.
- Lian X, Song W, Si TM, Lian NZ. Classification of musical hallucinations and the characters along with neural-molecular mechanisms of musical hallucinations associated with psychiatric disorders. World J Psychiatry 2024; 14(9): 1386-1396 DOI: 10.5498/wjp.v14.i9.1386.
- Costa OPF, Dalcim ML, Smaira SI, Lovadini GB. Musical hallucination or musical obsession? A differential diagnosis between two cases. Dement Neuropsychol. 2024 Jun 24;18:e20230073. doi: 10.1590/1980-5764-DN-2023-0073. PMID: 38933080; PMCID: PMC11206231.
- Golden EC, Josephs KA. Minds on replay: musical hallucinations and their relationship to neurological disease. Brain. 2015 Dec;138(Pt 12):3793-802. doi: 10.1093/brain/awv286. Epub 2015 Oct 7. PMID: 26446167.
- Duchêne J, Ribadeau Dumas A, Bonnard D, et al. Musical ear syndrome: prevalence and characteristics in cochlear implant bearers. Eur Ann Otorhinolaryngol Head Neck Dis 2021;138(3):153-7. doi: 10.1016/j.anorl.2020.11.005. Epub 2020 Nov 27. PMID: 33257264.
- Aldhafeeri FM. Musical Ear Syndrome in a Patient with Unilateral Hearing Loss: A Case Report. Am J Case Rep. 2022 Sep 20;23:e936537. doi: 10.12659/AJCR.936537. PMID: 36123807; PMCID: PMC9511037.
- Moseley P, Alderson-Day B, Kumar S, Fernyhough C. Musical hallucinations, musical imagery, and earworms: A new phenomenological survey. Conscious Cogn. 2018 Oct;65:83-94. doi: 10.1016/j.concog.2018.07.009. Epub 2018 Aug 1. PMID: 30077016; PMCID: PMC6204882.
- Griffiths TD. Musical hallucinosis in acquired deafness. Phenomenology and brain substrate. Brain. 2000 Oct;123 ( Pt 10):2065-76. doi: 10.1093/brain/123.10.2065. PMID: 11004124.
- Killingly C, Lacherez P. The song that never ends: The effect of repeated exposure on the development of an earworm. Q J Exp Psychol (Hove). 2023 Nov;76(11):2535-2545. doi: 10.1177/17470218231152368. Epub 2023 Feb 4. PMID: 36622014; PMCID: PMC10585939.
- Clark, T., Williamon, A., & Aksentijevic, A. (2012). Musical imagery and imagination: The function, measurement, and application of imagery skills for performance. In The Oxford handbook of music psychology (pp. 329-348). Oxford University Press. https://doi.org/10.1093/acprof:oso/9780199568086.003.0022
- Marneros A, Beyenburg S, Berghaus A. Unilateral hallucinations and other psychotic symptoms due to otosclerosis. Psychopathology. 1997 Mar-Apr;30(2):89-92. doi: 10.1159/000285034. PMID: 9168564.
- Auffarth IS, Kropp S. Musical hallucination in a patient after cochlear implantation. J Neuropsychiatry Clin Neurosci. 2009 Spring;21(2):230-1. doi: 10.1176/jnp.2009.21.2.230. PMID: 19622701.
- El Haj M, Jardri R, Larøi F, Antoine P. Hallucinations, loneliness, and social isolation in Alzheimer’s disease. Cogn Neuropsychiatry. 2016;21(1):1-13. doi: 10.1080/13546805.2015.1121139. Epub 2016 Jan 6. PMID: 26740416.
- Low WK, Tham CA, D’Souza VD, Teng SW. Musical ear syndrome in adult cochlear implant patients. J Laryngol Otol. 2013 Sep;127(9):854-8. doi: 10.1017/S0022215113001758. Epub 2013 Aug 13. PMID: 23941807.
- Cope TE, Baguley DM. Is musical hallucination an otological phenomenon? a review of the literature. Clin Otolaryngol. 2009 Oct;34(5):423-30. doi: 10.1111/j.1749-4486.2009.02013.x. PMID: 19793274.
- Van Ranst A, Keereman V, Hemelsoet D, De Herdt V. Sensory deafferentation syndromes: a case of Charles Bonnet and musical ear syndrome. Acta Neurol Belg. 2017 Sep;117(3):769-770. doi: 10.1007/s13760-016-0728-9. Epub 2017 Jan 16. PMID: 28093697.
- Schmitgen A, Saal J, Sankaran N, Desai M, Joseph I, Starr P, Chang EF, Shirvalkar P. Musical Hallucinations in Chronic Pain: The Anterior Cingulate Cortex Regulates Internally Generated Percepts. Front Neurol. 2021 May 4;12:669172. doi: 10.3389/fneur.2021.669172. PMID: 34017308; PMCID: PMC8129573.
- Parnas J, Yttri JE, Urfer-Parnas A. Phenomenology of auditory verbal hallucination in schizophrenia: An erroneous perception or something else? Schizophr Res. 2024 Mar;265:83-88. doi: 10.1016/j.schres.2023.03.045. Epub 2023 Apr 5. PMID: 37024418.
- de Leede-Smith S, Barkus E. A comprehensive review of auditory verbal hallucinations: lifetime prevalence, correlates and mechanisms in healthy and clinical individuals. Front Hum Neurosci. 2013 Jul 16;7:367. doi: 10.3389/fnhum.2013.00367. PMID: 23882203; PMCID: PMC3712258.
- Chiang YH, Beckstead JW, Lo SC, Yang CY. Association of auditory hallucination and anxiety symptoms with depressive symptoms in patients with schizophrenia: A three-month follow-up. Arch Psychiatr Nurs. 2018 Aug;32(4):585-590. doi: 10.1016/j.apnu.2018.03.014. Epub 2018 Mar 13. PMID: 30029752.
- Stanghellini G, Langer AI, Ambrosini A, Cangas AJ. Quality of hallucinatory experiences: differences between a clinical and a non-clinical sample. World Psychiatry. 2012 Jun;11(2):110-3. doi: 10.1016/j.wpsyc.2012.05.007. PMID: 22654943; PMCID: PMC3363387.
- McCarthy-Jones S, Longden E. Auditory verbal hallucinations in schizophrenia and post-traumatic stress disorder: common phenomenology, common cause, common interventions? Front Psychol. 2015 Jul 28;6:1071. doi: 10.3389/fpsyg.2015.01071. PMID: 26283997; PMCID: PMC4517448.
- Wallis S, Denno P, et al. The phenomenology of auditory verbal hallucinations in emotionally unstable personality disorders and post-traumatic stress disorder. Irish Journal of Psychological Medicine. 2022;39(2):196-206.doi:10.1017/ipm.2020.77
- Pineault, Dany (2023). Managing older adults with cognitive health worries. Audiologist Today, April 2023 - Volume 10 - Issue 3. https://canadianaudiologist.ca/13192-2/?output=pdf
- Eversfield CL, Orton LD. Auditory and visual hallucination prevalence in Parkinson’s disease and dementia with Lewy bodies: a systematic review and meta-analysis. Psychol Med. 2019 Oct;49(14):2342-2353. doi: 10.1017/S0033291718003161. Epub 2018 Nov 26. PMID: 30474581; PMCID: PMC6763539.
- McCarthy-Jones S, Trauer T, Mackinnon A, Sims E, Thomas N, Copolov DL. A new phenomenological survey of auditory hallucinations: evidence for subtypes and implications for theory and practice. Schizophr Bull. 2014 Jan;40(1):231-5. doi: 10.1093/schbul/sbs156. Epub 2012 Dec 23. PMID: 23267192; PMCID: PMC3885292.
- Maijer, K., Begemann, M. J. H., Palmen, S., Leucht, S., and Sommer, I. E. C. (2018). Auditory hallucinations across the lifespan: a systematic review and meta-analysis. Psychol. Med. 48, 879–888. doi: 10.1017/s0033291717002367
- Choong C, Hunter MD, Woodruff PW. Auditory hallucinations in those populations that do not suffer from schizophrenia. Curr Psychiatry Rep. 2007 Jun;9(3):206-12. doi: 10.1007/s11920-007-0020-z. PMID: 17521516
- Linszen MMJ, van Zanten GA, Teunisse RJ, Brouwer RM, Scheltens P, Sommer IE. Auditory hallucinations in adults with hearing impairment: a large prevalence study. Psychol Med. 2019 Jan;49(1):132-139. doi: 10.1017/S0033291718000594. Epub 2018 Mar 20. PMID: 29554989.
- Cole MG, Dowson L, Dendukuri N, Belzile E. The prevalence and phenomenology of auditory hallucinations among elderly subjects attending an audiology clinic. Int J Geriatr Psychiatry. 2002 May;17(5):444-52. doi: 10.1002/gps.618. PMID: 11994933.
- Dobie, R.A. (2004) Overview: suffering from tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. Lewiston, New York: BC Decker Inc., 1–7.
- Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, Archer SM, Blakley BW, Carter JM, Granieri EC, Henry JA, Hollingsworth D, Khan FA, Mitchell S, Monfared A, Newman CW, Omole FS, Phillips CD, Robinson SK, Taw MB, Tyler RS, Waguespack R, Whamond EJ. Clinical practice guideline: tinnitus executive summary. Otolaryngol Head Neck Surg. 2014 Oct;151(4):533-41. doi: 10.1177/0194599814547475. PMID: 25274374.
- Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990 Aug;8(4):221-54. doi: 10.1016/0168-0102(90)90031-9. PMID: 2175858.
- Sacks, O. (2007). Musicophilia: Tales of music and the brain (pp. 230-250). Alfred A. Knopf. Chapter 11: Musical hallucinations.
- Tracy DK, Shergill SS. Mechanisms underlying auditory hallucinations-understanding perception without stimulus. Brain Sci. 2013 Apr 26;3(2):642-69. doi: 10.3390/brainsci3020642. PMID: 24961419; PMCID: PMC4061847.
- Marschall TM, Brederoo SG, Ćurčić-Blake B, et al. Deafferentation as a cause of hallucinations. Current opinion in psychiatry 2020;33(3):206-11.
- Uchida Y, Sugiura S, Nishita Y, Saji N, Sone M, Ueda H. Age-related hearing loss and cognitive decline - The potential mechanisms linking the two. Auris Nasus Larynx. 2019 Feb;46(1):1-9. doi: 10.1016/j.anl.2018.08.010.
- Powell DS, Oh ES, Reed NS, Lin FR, Deal JA. Hearing Loss and Cognition: What We Know and Where We Need to Go. Front Aging Neurosci. 2022 Feb 28;13:769405. doi: 10.3389/fnagi.2021.769405.
- Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013 Nov 9;382(9904):1600-7. doi: 10.1016/S0140-6736(13)60142-7.
- Henry JA, Roberts LE, Caspary DM, Theodoroff SM, Salvi RJ. Underlying mechanisms of tinnitus: review and clinical implications. J Am Acad Audiol. 2014 Jan;25(1):5-22; quiz 126. doi: 10.3766/jaaa.25.1.2. PMID: 24622858; PMCID: PMC5063499.
- Bernardini F, Attademo L, Blackmon K, Devinsky O. Musical hallucinations: a brief review of functional neuroimaging findings. CNS Spectr. 2017 Oct;22(5):397-403. doi: 10.1017/S1092852916000870. Epub 2016 Dec 19. PMID: 27989258.
- Vitorovic D, Biller J. Musical hallucinations and forgotten tunes - case report and brief literature review. Front Neurol. 2013 Aug 8;4:109. doi: 10.3389/fneur.2013.00109. PMID: 23964264; PMCID: PMC3737457.
- Cavaliere C, Longarzo M, Orsini M, Aiello M, Grossi D. Fronto-Temporal Circuits in Musical Hallucinations: A PET-MR Case Study. Front Hum Neurosci. 2018 Sep 27;12:385. doi: 10.3389/fnhum.2018.00385. PMID: 30319380; PMCID: PMC6170624.
- Kaur A, Basavanagowda DM, Rathod B, Mishra N, Fuad S, Nosher S, Alrashid ZA, Mohan D, Heindl SE. Structural and Functional Alterations of the Temporal lobe in Schizophrenia: A Literature Review. Cureus. 2020 Oct 26;12(10):e11177. doi: 10.7759/cureus.11177. PMID: 33262914; PMCID: PMC7689947.
- Kasai K, Asada T, Yumoto M, Takeya J, Matsuda H. Evidence for functional abnormality in the right auditory cortex during musical hallucinations. Lancet. 1999 Nov 13;354(9191):1703-4. doi: 10.1016/S0140-6736(99)05213-7. PMID: 10568580.
- van Swam, C., Federspiel, A., Hubl, D., Wiest, R., Boesch, C., Vermathen, P., et al. (2012). Possible dysregulation of cortical plasticity in auditory verbal hallucinations-A cortical thickness study in schizophrenia. J. Psychiatr Res. 46, 1015–1023. doi: 10.1016/j.jpsychires.2012.03.016.
- Xu, J., Wang, J., Fan, L., Li, H., Zhang, W., Hu, Q., et al. (2015). Tractography-based parcellation of the human middle temporal gyrus. Sci. Rep. 5:18883. doi: 10.1038/srep18883.
- Roberts DL, Tatini U, Zimmerman RS, Bortz JJ, Sirven JI. Musical hallucinations associated with seizures originating from an intracranial aneurysm. Mayo Clin Proc. 2001 Apr;76(4):423-6. doi: 10.4065/76.4.423. PMID: 11322359.
- Cerrato P, Imperiale D, Giraudo M, Baima C, Grasso M, Lopiano L, Bergamasco B. Complex musical hallucinosis in a professional musician with a left subcortical haemorrhage. J Neurol Neurosurg Psychiatry. 2001 Aug;71(2):280-1. doi: 10.1136/jnnp.71.2.280. PMID: 11488278; PMCID: PMC1737492.
- Patel AD. Why would Musical Training Benefit the Neural Encoding of Speech? The OPERA Hypothesis. Front Psychol. 2011 Jun 29;2:142. doi: 10.3389/fpsyg.2011.00142. PMID: 21747773; PMCID: PMC3128244.
- Peretz I, Vuvan D, Lagrois MÉ, Armony JL. Neural overlap in processing music and speech. Philos Trans R Soc Lond B Biol Sci. 2015 Mar 19;370(1664):20140090. doi: 10.1098/rstb.2014.0090. PMID: 25646513; PMCID: PMC4321131.
- Koelsch S, Gunter TC, v Cramon DY, Zysset S, Lohmann G, Friederici AD. Bach speaks: a cortical “language-network” serves the processing of music. Neuroimage. 2002 Oct;17(2):956-66. PMID: 12377169.
- Gordon AG. Do musical hallucinations always arise from the inner ear? Med Hypotheses. 1997 Aug;49(2):111-22. doi: 10.1016/s0306-9877(97)90216-4. PMID: 9278923.
- Lo YL, Hameed S, Rumpel H, Chan LL. Auditory hallucinations and migraine of possible brainstem origin. J Headache Pain. 2011 Oct;12(5):573-5. doi: 10.1007/s10194-011-0355-z. Epub 2011 Jun 4. PMID: 21643695; PMCID: PMC3173622.
- Furia A, Licchetta L, Muccioli L, Ferri L, Mostacci B, Mazzoni S, Menghi V, Minardi R, Tinuper P, Bisulli F. Epilepsy With Auditory Features: From Etiology to Treatment. Front Neurol. 2022 Jan 27;12:807939. doi: 10.3389/fneur.2021.807939. PMID: 35153984; PMCID: PMC8829259.
- Coebergh JA, Lauw RF, Bots R, Sommer IE, Blom JD. Musical hallucinations: review of treatment effects. Front Psychol. 2015 Jun 16;6:814. doi: 10.3389/fpsyg.2015.00814. PMID: 26136708; PMCID: PMC4468361.
- Sanchez TG, Rocha SC, Knobel KA, Kii MA, Santos RM, Pereira CB. Musical hallucination associated with hearing loss. Arq Neuropsiquiatr. 2011;69(2B):395-400. doi: 10.1590/s0004-282x2011000300024. PMID: 21625772.
- Doluweera Y, Suraweera C. Those Who Hear Music: Three Cases on Musical Hallucinations. Case Rep Psychiatry. 2018 Jun 27;2018:9361382. doi: 10.1155/2018/9361382. Erratum in: Case Rep Psychiatry. 2021 Jan 30;2021:7603280. doi: 10.1155/2021/7603280. PMID: 30050719; PMCID: PMC6040295.
- Pineault, Dany (2024). The bidirectional association between tinnitus & mental well-being: clinical implications for audiologists. Audiologist Today, April 2024 - Volume 11 - Issue 2. https://canadianaudiologist.ca/13192-2/?output=pdf
- Hashim MJ. Patient-Centered Communication: Basic Skills. Am Fam Physician. 2017 Jan 1;95(1):29-34. PMID: 28075109.
- Herr RM, Bosch JA, Theorell T, Loerbroks A. Bidirectional associations between psychological distress and hearing problems: an 18-year longitudinal analysis of the British Household Panel Survey. Int J Audiol. 2018 Nov;57(11):816-824. doi: 10.1080/14992027.2018.1490034. Epub 2018 Jul 27. PMID: 30052099.
- Kaneko Y, Oda Y, Goto F. Two cases of intractable auditory hallucination successfully treated with sound therapy. Int Tinnitus J. 2010;16(1):29-31. PMID: 21609910.

