What’s New about Getting Older
What’s New About Getting Older?
Kathy Pichora-Fuller's column “What’s new about getting older?” delves into all aspects of ageing and hearing ranging from health policy developments to neurophysical research on the aging auditory brain.
Integrating Sensory Health to Promote Healthy Aging and Brain Health: Development of the Brain Health PRO Program
Hearing Health and Healthy Aging
Of course, hearing healthcare for older adults is beneficial for communication. Beyond improving communication, it is imperative to position hearing healthcare in the broader context of healthy aging because there are important links between hearing health and many physical, mental, and social aspects. Accordingly, the over-arching goal for audiologic rehabilitation is expanding to include promoting healthy aging (Pichora-Fuller, 2024). The World Health Organization (WHO) includes hearing in its guidance on integrated primary care for older people (ICOPE; WHO, 2017, 2024), where the following important terms are defined: “Healthy ageing: The process of developing and maintaining the functional ability that enables well-being in older age” and “Functional ability: The health-related attributes that enable people to be and to do what they have reason to value; it is made up of the intrinsic capacity of the individual, relevant environmental characteristics, and the interactions between the individual and these characteristics.” The original six intrinsic capacities of ICOPE included hearing, along with cognition, vision, mobility, mental health, and nutrition (WHO, 2017). Additional capacities (e.g., continance) were added in the recently published second edition of ICOPE (WHO, 2024).
Hearing Health and Brain Health

While there are many links between hearing health and other aspects of healthy aging, however, in the wake of the the Lancet reports outlining potentially modifiable risk factors for dementia (Livingston et al., 2017, 2020, 2024), audiologists have become especially intrigued by the links between hearing and cognition and possible implications for intervention (Pichora-Fuller, 2023). In addition to hearing loss, the number of health issues recognized as possible risk factors for dementia have increased as more evidence has become available (e.g., vision was included as a potential risk factor in Livingston et al., 2024). More nuanced interpretations of population-attributable fractions and investigations into their generalizability to different countries and sub-populations have also been explored, including studies using data from the Canadian Longitudinal Study on Aging (see Pichora-Fuller & Mick, 2024). The current Lancet list of 14 potential modifiable risk factors for dementia include: low education, hearing loss, high LDL cholesterol, depression, traumatic brain injury, physical inactivity, diabetes, smoking, hypertension, obesity, excessive alchol, social isolation, air pollution, and vision loss, with sleep as a likely future addition (Livingston et al., 2024).
Brain Health PRO
With the increasing connections between hearing and healthy aging in general, and between hearing and cognitive health in particular, there has been an emerging plethora of potentially important connections to hearing healthcare that may be productive to integrate in interventions. A recently developed Canadian example of a multi-domain integrated intervention to promote brain health and reduce risk of dementia is “Brain health PRO/Santé cerveau PRO” (Belleville et al., 2025). It was designed by a large team of Canadian researchers to be an evidence-based online educational program (in English or French). The main goals are to increase participant literacy, empowerment, and engagement in activities that support personal brain health, potentially reducing dementia risk.
The program provides information and guidance on seven potentially modifiable behavioural risk factors for dementia, including sensory health. Progress through the content is determined by the individual and their behavioural factors, but is guided by a model including personal and environmental determinants that could influence risk, cognitive health and quality of life. Note that personal and environmental determinants are important as the contextual components in the WHO International Classification of Functioning (ICF) model that is often used to guide audiologic rehabilitation (Humes et al., 2020). The personal and environmental determinants used to tailor Brain health PRO to individual needs include considerations that apply across domains, with most if not all of these considerations being relevant for hearing healthcare planning. Could/should audiologists consider these factora and determinants?
Behavioural factors:
- engagement in physical activity,
- engagement in cognitively stimulating activities,
- social and psychological health,
- nutrition,
- vascular health,
- sleep
- sensory health (vision and hearing).
Personal determinants:
- lack of knowledge about modifiable risk associated with decline;
- difficulty recognizing personal risk levels and their implications;
- limited understanding of potential to affect individual risk;
- unhealthy habits with targeted risk domains;
- lack of motivation;
- difficulty in meeting challenges, solving problems and coping effectively;
- low self-efficacy in making changes in modifiable risk factors,
- limited numeracy and health literacy
- negative attitudes toward aging and demenia.
Envionmental determinants include:
- limited access to environment conducive to exercise,
- limited financial resources,
- limited access to educational programs,
- limited access to healthy foods,
- stressful environment,
- isolation and limited access to social activities,
- limited access to health professionals,
- absence of community organizations providing support and resources,
- program not adapted to individual’s numeracy and health literacy.
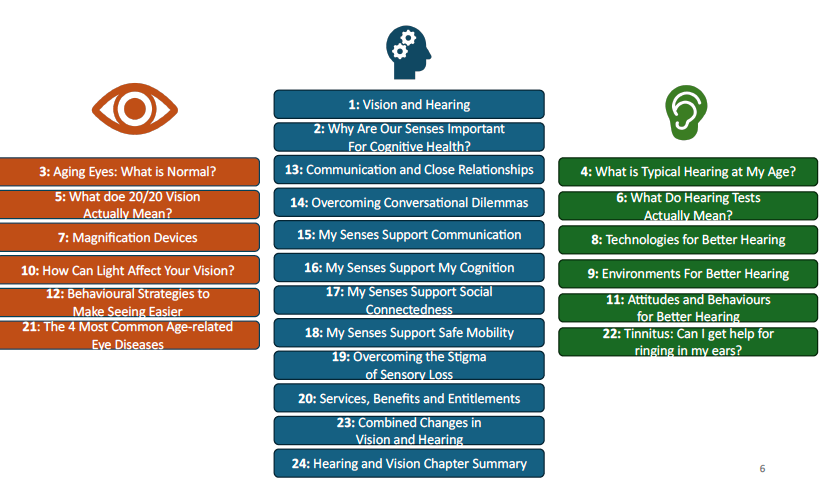
The full Brain health PRO program is designed to be completed over a 45-week period. The content for the sensory module of the program consists of 24 10-minute ‘chapters’ as outlined below (Pichora-Fuller & Wittich, 2025; CCNA webinar link (https://vimeo.com/1069995479). Some chapters focus on hearing and some on vision, but some chapters link hearing with vision and there are also links between the senses and other modules in Brain health PRO (e.g., engagement in cognitive, physical and social activities). Much of the content linking hearing health to other aspects of healthy aging could be generalized in other audiologic rehabilitation educational programs.
A pilot study was conducted to evaluate the usability and acceptance based on the administration of a shorter 15-week version of the program. The pilot study showed excellent outcomes in terms of usability and acceptance (Belleville et al., 2025). Research is now beginning to evaluate the implementation of Brain health PRO as an online educational option for older adults seen in clinical and community settings across Canada. The roll out of Brain health PRO may encourage older adults to address their hearing health as part of the larger agenda to promote healthy aging, in particular brain health. This work provides an opportunity for audiologists to form their own new connections to integrated care for older people.
References
- Belleville, S., Anderson, N. D., Bherer, L., Camicioli, R., Carrier, J., Chan, S., Cuesta, M., -Vu, Emily Dwosh, T. T., Fiocco, A. J., Ferland, G., Gilbert, B., Harris, E., Itzhak, I., Jarrett, P., Kadri, M. A., Laurin, D., Liu-Ambrose, T., McGibbon, C. A., Middleton, L., Miller, L., Nygaard, H. B., Montero-Odasso, M., Murphy, K., Phillips, N., Pichora-Fuller, M. K., Robillard, J. M., Smith, E. E., Speechley, M., Trigui, A., Wittich, W., Chertkow, H., Feldman, H. H. (2025). Brain health PRO/Santé cerveau PRO: The development of a web-based program for dementia literacy and risk factor reduction. The Journal of Prevention of Alzheimer’s Disease, 100134. https://doi.org/10.1016/j.tjpad.2025.100134.
- Humes, L. E., Pichora-Fuller, M. K., & Hickson, L. (2020). Functional consequences of impaired hearing in older adults and implications for intervention (pp. 257-280). In K. Helfer, E. Bartlett, A. Popper, & R. R. Fay (Eds), Aging and hearing: Causes and consequences, Springer Handbook of Auditory Research 72. Springer Nature Switzerland AG. https://doi.org/10.1007/978-3-030-49367-7_11
- Livingston, G., Huntley, J., Liu, K. Y., Costafreda, S. G., Selbæk, G, Alladi, S., et al. (2024). Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. The Lancet, published online July 31, 2024 https://doi.org/10.1016/S0140-6736(24)01296-0
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S. et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413-446. https://doi.org/10.1016/S0140-6736(20)30367-6
- Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames, D. et al. (2017). Dementia prevention, intervention, and care. The Lancet, 390(10113), 2673-2734. https://doi.org/10.1016/S0140-6736(17)31363-6
- Pichora-Fuller, M. K. (2023). Is hearing loss in older adults predictive of later development of dementia and does hearing care modify dementia risk? Canadian Audiologist, January, 2023. https://canadianaudiologist.ca/issue/volume-10-issue-1-2023/is-hearing-loss-in-older-adults-predictive-of-later-development-of-dementia-and-does-hearing-care-modify-dementia-risk/
- Pichora-Fuller, M. K. (2024). Inter-professional team collaborations to achieve hearing care in integrated person-centered care for older adults: A New Year’s resolution for 2024. Canadian Audiologist, January, 2024. https://canadianaudiologist.ca/issue/volume-11-issue-1-2024/column/whats-new-about-getting-older/
- Pichora-Fuller, M. K., & Mick, P. T. (2024). The risks of explaining hearing loss as a potentially modifiable risk factor for dementia: Summer 2024 update on new global and Canadian population attributable fractions (PAFs). Canadian Audiologist, 11(5), this issue.
- Pichora-Fuller, M. K., & Wittich, W. (2025). Sensory and cognitive health. Canadian Consortium on Neurodegeneration in Aging (CCNA) BrainXchange webinar series, March 26, 2025. https://vimeo.com/1069995479
- World Health Organization. (2017). Integrated care for older people (ICOPE): guidelines on community-level interventions to manage declines in intrinsic capacity. Geneva, Switzerland. https://apps.who.int/iris/handle/10665/258981
- World Health Organization. (2024). Integrated care for older people: (ICOPE): Guidance for person-centred assessment and pathways in primary care (2nd Ed.). Geneva, Switzerland. https://www.who.int/publications/i/item/9789240103726

