Hearing Health is Associated to all Health
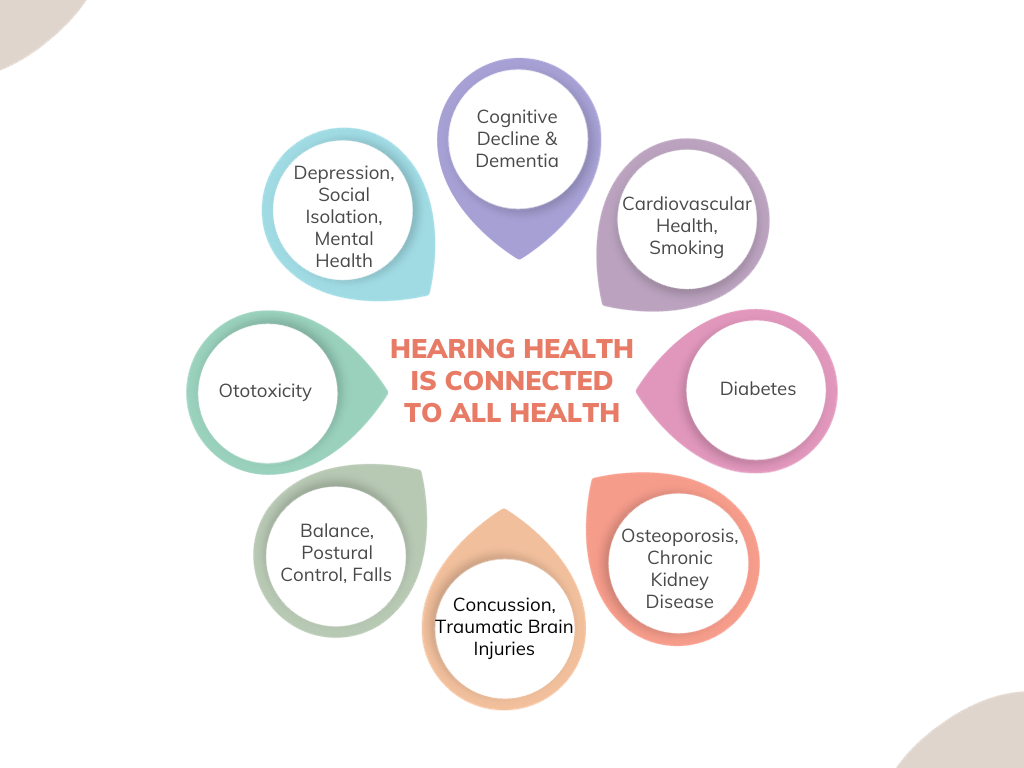
It is becoming increasingly recognized that untreated hearing loss is associated with increased risks of cognitive decline and dementia (Griffiths et al, 2020; Maidment et al., 2023; Pichora-Fuller, 2023); indeed, hearing loss is reported to account for 8% of all cases of dementia (Huang et al., 2023). Many possible mechanisms link hearing loss to dementia (Griffiths et al, 2020; Pichora-Fuller, 2023). Most interesting is the suggestion that early-onset hearing loss may affect changes in neuronal mechanisms and brain structures before the onset of dementia, thereby causing an increased risk of dementia (Griffiths et al, 2020). In addition, the increased cognitive load required for processing impoverished auditory input in those with hearing loss may affect neuronal and synaptic changes during dementia (Griffiths et al, 2020). This may limit cognitive and memory resources, causing decreased cognitive stimulation (Livingston et al., 2020) and cortical processing changes in the medial temporal lobe (Griffiths et al, 2020). At the same time, hearing loss is also associated with balance difficulty, poorer postural control, and increased risk of falls (Lin & Ferrucci, 2012). There also exists a relationship between hearing loss and cardiovascular health, including hypertension, diabetes, smoking, chronic kidney disease, high fever, osteoporosis, concussion, etc (Maidment et al., 2023). Inflammation and oxidative stress caused by cardiovascular events can directly damage cochlear proteins and impair molecular transport in cochlear cells (Maidment et al., 2023). Recent evidence has suggested that a minimum of 2.5 to 5 hours per week of moderate physical activity is recommended to achieve optimal health benefits and reduce metabolic risk factors of cardiovascular events (WHO, 2020). Improved cardiovascular health may have the added benefit of slowing down the progression of hearing loss, though this hasn’t been evident in the literature yet. However, physical activity has been shown to decline faster in older adults with reported hearing loss than those with no (Goodwin et al., 2023). This may be explained by the increased auditory, mental, and emotional fatigue and the cognitive load and attentional and mental resources required to process degraded and impoverished speech in those with hearing loss.
Hearing Care should be Integrated and Coordinate within the Larger Healthcare System
Given that hearing health is connected to all health and hearing loss is associated with a range of negative health consequences, it makes sense then that a holistic and interdisciplinary patient-centered approach should be managed integratively across health disciplines rather in silo. Unfortunately, in the world of audiology, there are several barriers to incorporating hearing health as an integral part of the patient care battery. Most important of these barriers, in my opinion, is likely a general lack or limitation in the awareness of the relationship between hearing loss and other health conditions. Thus, many healthcare professionals may forget or be unaware of the consequences of hearing impairment on health and quality of life. They may neglect to refer to audiology as part of a routine health assessment. In private practice audiology, financial barriers may also limit some of these referrals or access to audiological care for our patients. Audiology services are fee-for-service, and associated devices can be costly. While some provincial funding programs and extended health benefits offer funding for some, it is typically not enough; far from it. In addition, some people don’t have access to insurance or health benefits, which only further limits access to hearing health. Perhaps this serves as a part of an explanation for the continuing low penetration rates of hearing healthcare that we see in the industry. Regulatory and legal constraints in some provinces may also make interdisciplinary communication difficult, further adding to these barriers.
What can we do?
As audiologists in private practice, we have many gaps to bridge. Demanding that our patient’s care be holistic and integrative in the healthcare system’s context, we should strive to do and take the time to insist on. Our field is small and small in numbers, but we are growing, so our voices can be really loud. Working to raise awareness of the consequences of hearing impairments on general health should be the first priority. Advocating for our patients within their circle of care is equally important. At the same time, it is essential to widen our professional networks beyond our patient’s primary healthcare teams to include other health care practitioners that may also be involved in their care, directly or indirectly. For example, it would be particularly important for us to collaborate and communicate with our patients’ Otolaryngologists when we’ve recommended a referral to them to re-test and provide intervention in conjunction with outcomes. However, we often recommend the referral, and we never hear back about whether an appointment was given, let alone what the recommended intervention was. This needs to change, so that we can be kept in the loop. Similarly, working collaboratively with practitioners who work with patients who may be suffering from dementia or cognitive decline is also important to ensure their hearing acuity is considered during cognitive assessments. It is equally important for them to consider the potential future deleterious impact of hearing loss on further cognitive decline. There currently exists a gap in holistic and integrative interdisciplinary hearing health care. Evaluating a patient’s general health to offer more targeted support can help reduce and mitigate the burden of other diseases that come with hearing loss.
References
- Goodwin, M. V., Hogervorst, E., Hardy, R., Stephan, B. C., & Maidment, D. W. (2023). How are hearing loss and physical activity related? Analysis from the English longitudinal study of ageing. Preventive Medicine, 173, 107609.
- Griffiths, T. D., Lad, M., Kumar, S., Holmes, E., McMurray, B., Maguire, E. A., ... & Sedley, W. (2020). How can hearing loss cause dementia?. Neuron, 108(3), 401-412.
- Huang, A. R., Jiang, K., Lin, F. R., Deal, J. A., & Reed, N. S. (2023). Hearing loss and dementia prevalence in older adults in the US. Jama, 329(2), 171-173.
- Lin, F. R., & Ferrucci, L. (2012). Hearing loss and falls among older adults in the United States. Archives of internal medicine, 172(4), 369-371.
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., ... & Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413-446.
- Maidment, D. W., Wallhagen, M. I., Dowd, K., Mick, P., Piker, E., Spankovich, C., & Urry, E. (2023). New horizons in holistic, person-centred health promotion for hearing healthcare. Age and Ageing, 52(2), afad020.
- Pichora-Fuller, K. (2023). Is Hearing Loss in Older Adults Predictive of Later Development of Dementia and Does Hearing Care Modify Dementia Risk? Canadian Audiologist, 10(1).
- World Health Organisation. WHO Guidelines on Physical Activity and Sedentary Behaviour. Geneva: World Health Organisation, 2020.

