Striking the Right Balance: The Importance of Screening for Vestibular Impairment in Children
In this edition of “Striking the Right Balance,” Dr. Joshua Huppert discusses the importance of screening for vestibular disorders in the pediatric population.
If you are a health care professional and would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by emailing CAAvestibular@gmail.com to let us know you want to be included. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
Review of the Vestibular System
The peripheral vestibular system is composed of five sensory organs housed in the inner ear – three semi-circular canals and two otolith organs. The three semi-circular canals, oriented orthogonally in the dense, petrous portion of the temporal bone of the skull, detect angular (i.e., rotational) movement of the head, while the two otolith organs, the utricle and saccule, detect gravitational pull and linear movement of the head and body in space. Collectively, these five sensory organs relay information about motion, equilibrium, and spatial orientation through the superior and inferior portions of the vestibulocochlear nerve (i.e., cranial nerve VIII) to the brain.1 Although all five sensory organs are functional at birth, connections between the peripheral and central vestibular systems (required for balance) continue to develop until 12 years of age,2 at which point they are thought to peak in order to facilitate the development of emerging motor skills and postural control.3
Vestibular function is achieved and maintained through complex interactions between the vestibular, vision, and proprioception systems, all of which integrate at the level of the cerebellum. Specifically, these systems collectively mediate the function of three primary reflexes (vestibulo-ocular reflex [VOR], vestibulo-colic reflex [VCR], and the vestibulo-spinal reflex [VSR]) that allow individuals to see clearly when moving about his/her environment, identify orientation with respect to gravity, determine direction and speed of movement, and make automatic postural adjustments to maintain posture and stability in various conditions and activities.1 Therefore, it stands to reason that, should the communication and integration of any/all of these sensory systems be erroneous, some degree of impairment would ensue.
Interestingly enough, emerging audiological research and clinical practice in the areas of pediatric vestibular assessment and management has begun to expose the consequences these types of impairments may have on overall development and patient quality of life measures.
Prevalence of Vestibular Disorders in Children
Until fairly recently, very little was known about the prevalence of vestibular disorders in children. Not only do children lack the vocabulary to accurately describe hallmark presentations associated with vestibular disorders (e.g., vertigo), but many of these disorders often manifest themselves in the form of visual disturbances, headaches, clumsiness, sensory processing difficulties, delayed developmental milestones, or even learning disabilities, making the recognition and/or diagnosis of vestibular disorders challenging for both parents and professionals alike.4
Fortunately, in April of 2016, the National Institute on Deafness and Other Communication Disorders (NIDCD) funded the Child Balance Supplement (CBC) to the 2012 National Health Interview Survey (NHIS) in an effort to better determine the prevalence of, risk factors associated with, and availability of services for children with vestibular and balance impairments. The study, led by NIDCD statistician, Chuan-Ming Li, was published in the Journal of Paediatrics, and included data collected on nearly 11,000 children.5 The remarkable findings were as follows:
- The United States’ (US) nationally-weighted prevalence of vestibular disorders in children between the ages of 3 and 17 was found to be 5.3%.
- According to this data, more than 1 in 20 (nearly 3.3. million) US children may have a vestibular disorder.
- Children with hearing impairment are two times more likely to have vestibular disorders compared to children with normal hearing.
Based upon the findings presented in the NIDCD study, it would appear that vestibular disorders are actually far more common in children than we initially thought.
Screening for Vestibular Impairment in Children
According to Devin McCaslin, PhD, Director of the Vestibular/Balance Laboratory at Mayo Clinic in Rochester, MN, “One of the key indicators of a vestibular impairment is whether a child achieves their traditional milestones at appropriate times.” One example provided by Dr. McCaslin regarded how typically developing children begin to sit and crawl at approximately 5–6 months of age; however, children with underlying vestibular impairment may not begin to sit and crawl until approximately 8–18 months of age. Dr. McCaslin then goes on to say, “It can take a child with vestibular impairment 33 months to learn to walk independently versus only 12 months for an age-matched child with normal function.”3 Based upon Dr. McCaslin’s advice, delayed motor milestones may be the first sign of an underlying vestibular impairment in children. Additionally, as mentioned in the NIDCD study, children with hearing impairment are two times more likely to have vestibular disorders when compared to children with normal hearing. For this reason, screening of vestibular function should also be strongly considered in all children with hearing loss.
While at Vanderbilt University in Nashville, TN, Dr. McCaslin and his team utilized the following benchmarks (Table 1) to screen for developmental motor milestones in children. Should screening reveal the child to be at risk, comprehensive vestibular evaluation and/or medical evaluation by the child’s pediatrician and/or managing otolaryngologist may be warranted.6
Table 1. Benchmarks That Can Be Used to Screen Motor Milestone Benchmarks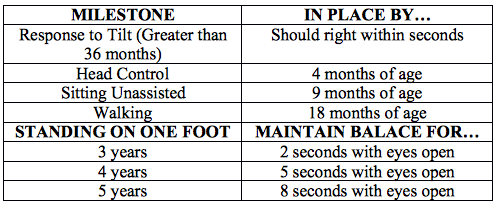
Lastly, use of self-report measures should also be considered for use in the clinic. The Pediatric Dizziness Handicap Inventory for Patient Caregivers (pDHI-PC), similar to the Dizziness Handicap Inventory (DHI),7 was designed to be administered to the caregiver(s) of children 5–12 years of age and aims to determine the impact present symptomology associated with dizziness/imbalance may have on patient quality of life. Utilization of the DHI might be considered at the discretion of the clinician for children beyond 12 years of age, as the reliability of the patient subjective report typically improves with age/maturity. Another self-report measure, created by physical therapist, Dr. Marousa Pavlou and colleagues, is the Pediatric Vestibular Symptom Questionnaire (PVSQ)8 and can be utilized for children between 6 and 17 years of age. The PVSQ aims to determine whether or not the subjective symptomology relating to dizziness/imbalance reported by the patient and/or his/her caregiver is mediating from the inner ear. The PVSQ is especially helpful in determining whether or not comprehensive vestibular evaluation is warranted and, if not, which type of specialty referral might be most appropriate based upon the presentation/report provided by the patient and his/her family. The pDHI-PC is available online through the American Speech Language and Hearing Association (ASHA) and the PVSQ is available online through The Journal of Paediatrics, as there is no copyright or license currently attached to its use, which has been confirmed by Dr. Pavlou herself.
NOTE: Should comprehensive vestibular evaluation be warranted, most of the present test battery used to assess vestibular function can be adapted for evaluation in children, as discussed explicitly in the Manual of Pediatric Balance Disorders by Drs. Robert O’Reilly, Thierry Morlet, and Sharon Cushing; however, site-specific normative data should be collected prior to evaluation to adequately account for maturational differences in development between children and adults. Additionally, prior to collecting data, each institution is strongly encouraged to consult with their research and development department and/or Institutional Review Board (IRB) to ensure proper execution of procedure as defined by their institution.
Centres Offering Services for the Assessment and Management of Vestibular Disorders in Children
Thankfully, a handful of pediatric institutions across the US and Canada have recognized and responded to the need for assessing, diagnosing, treating, managing, and rehabilitating children with vestibular disorders. Most of these centres utilize a multi-disciplinary approach that lend themselves well to comprehensively evaluating this complex sensory system from a multitude of different expert lenses including audiology, physical therapy, otolaryngology, neurology, optometry/ophthalmology, and gait specialists.
Current major medical centres with pediatric vestibular programs include, but are not limited to: Children’s Hospital Colorado (Aurora, CO), Nemours/A.I. duPont’s Hospital for Children (Wilmington, DE), Boston Children’s Hospital (Boston, MA), Hospital for Sick Children (Toronto, Ontario), Vanderbilt University (Nashville, TN), Boystown National Research Hospital (Omaha, NE), American Balance Institute (Largo, FL), Children’s of Alabama (Birmingham, AL), Rady Children’s Hospital (San Diego, CA), and Children’s Hospital of Philadelphia (Philadelphia, PA).
References
- VEDA. The Human Balance System. Portland, OR: Author; 2016. Available at: http://vestibular.org/understanding-vestibular-disorder/human-balance-system.
- Peterson ML, Christou E, Rosengren KS. Children achieve adult-like sensory integration during stance at 12-years-old. Gait Posture 2006 Jun;23(4):455–63. Epub 2005 Jul 5.
- McCaslin DL. 20Q: Pediatric vestibular disorders and the role of the audiologist. AudiologyOnline, Article 17145; 2016. Retrieved from www.audiologyonline.com.
- O'Reilly R, Cushing SL, and Morlet T. Manual of Pediatric Balance Disorders. San Diego: Plural Publishing; 2013.
- Li CM, Hoffman JJ, War BK, et al. Epidemiology of dizziness and balance problems in children in the United States: A population-based study. J Pediatr 2016;171:240–47.
- McCaslin DL, Jacobson GP, Lambert W, et al. The development of the Vanderbilt Pediatric Dizziness Handicap Inventory for Patient Caregivers (DHI-PC). Int J Pediatr Otorhinolaryngol 2015;79:1662–66.
- Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990 Apr;116(4):424–7.
- Pavlou M, Whitney S, Alkathiry AA, et al. The Pediatric Vestibular Symptom Questionnaire: A validation study. J Pediatr 2016;168:171–7.

