Improving Accessibility: Expanding the Role of Audiologists in the Built Environment
The need to improve accessibility for people who are Deaf/deaf or hard of hearing in our communities is imperative. Hearing loss negatively affects interpersonal communication, psychosocial well-being, and quality of life. 1–6 Hearing loss is now the fourth leading cause of years lived with disability7 and the WHO estimates the annual cost of unaddressed hearing loss to be about US$750 billion globally.8 The aging population is also at risk of downstream conditions from hearing loss such as dementia,9 social and emotional loneliness,10 depression,11 changing family and community engagement,12 and increasing risk of falls and other physical disabilities.13
Hearing loss creates serious barriers in educational and workplace environments. The Statistics Canada Participation and Activity Limitation Survey (2006) found 39.8 % of respondents with a hearing loss reported it influenced their choice of courses or careers and 20.3% discontinued their formal education because of it. Regarding the workplace, 33.2% of employed respondents reported hearing loss limited the amount or kind of work they could perform and 32.3 % made it difficult to advance or change jobs. Of the 23.4% not participating in the labour force, 62.5% reported they were completely prevented from working, while 29.0% stated it affected their ability to look for work. Of those respondents who were retired, 39.7% reported their retirement had not been voluntary and 51.3% were completely prevented from working as a result of their hearing loss.14
Environment includes “cultural, institutional, physical, and social elements that lie outside of individuals, yet are embodied in individual actions.”15 Physical ‘built’ environments include housing, public buildings (e.g., government services, businesses, workplaces, hospitals, nursing homes, educational institutions), transportation (e.g., airports, subway), and social/cultural/recreational locations. Poor acoustics and lighting, background noise, distance to speaker, and reverberation are all too common and can cause poor speech intelligibility and increased listening effort. MarkeTrak IX reported the listening situation with the lowest satisfaction level across all groups surveyed was ‘trying to follow a conversation in the presence of noise’ (50% satisfaction for owners with hearing aids 6+ years old; 67% satisfaction for aids <5 years old). Non-owners were the least satisfied (25% satisfaction) with their ability to hear in this environment, indicating speech in noise was a universal problem. It was noted classrooms and large lecture halls were more problematic than other venues.16
In examining the role of the field of audiology in reducing these barriers, it is important to consider different models of disability. For most areas of audiology, a ‘medical model’ still persists. This model defines disability as a health problem, disease, illness or abnormality that is situated within the individual.17 Medical treatment is directed at the underlying pathology in an attempt to correct or prevent the abnormality. Critics argue that this views disability in terms of an individual deficit rather than in terms of being generated by the social consequences of the impairment.18,19
The charity model of disability sees people with disabilities as victims of their impairment. It is characterized by concepts of caretaking, protection, and segregation. Disability is seen as a deficit resulting in institutional care settings separating people from wider society.20 In 2018, Jackson argued that a consequence of institutionalization in our past is that much of our current built environment is inaccessible for people with disabilities.21
The cultural model of disability is at odds with the medical model as the Canadian Association of the Deaf report many Deaf people do not perceive themselves as ‘impaired.’ Deaf culture is seen as a healthy sociological community and a person’s status within the culture depends not upon their amount of hearing loss but upon their attitude towards the elements of the Deaf culture, involvement in the local Deaf community, and skill in sign language.22
The social model of disability counters the medical model approach by suggesting disability arises, not as a result of impairment, but from barriers within ‘an oppressive and discriminating society.’21,23 The social model shifts the onus away from an individual who requires a cure to the community itself for creating barriers that constructs the disability. A perceived strength of the social model is that it is socially and politically located in activism for social change.24,25 With regards to hearing, these barriers could affect people who have any degree of hearing loss or auditory processing difficulty. Examples of barriers include poorly designed spaces with poor acoustics, reverberation, background noise, distance, and visual obstructions. Other examples include inaccessible media (no closed captioning), lack of sign language interpreters, lack of access to assistive technologies (e.g. hearing aids, hearing loop systems, FM/IR systems, sound field systems, CART, alerting systems), discriminatory work practices, and societal prejudices.
The WHO International Classification of Functioning and Disability framework seen in figure one26 is a framework which aids in the conceptual basis for the definition, measurement and policy formulations for health and disability. It focuses on improving participation and function when doing an activity while addressing environmental and personal factors. Environmental factors make up the physical, social and attitudinal environment in which people live and conduct their lives. It characterizes disability as the result of a complex relationship between an individual’s health condition, their personal factors, and of the external factors that represent the circumstances in which the individual lives.
Figure 1. The International Classification of Functioning and Disability (ICF) framework [WHO (2001)].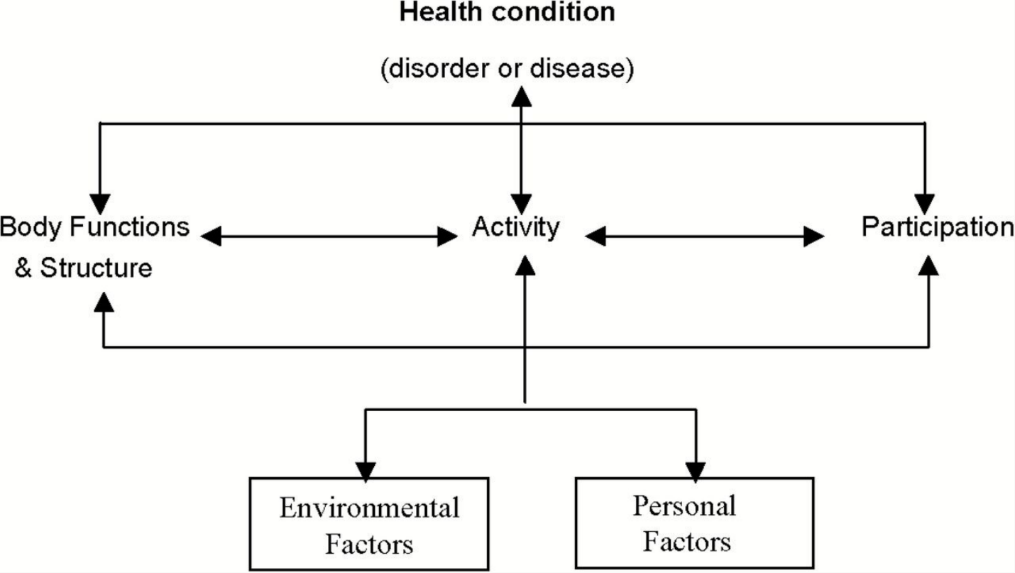
Audiology Outside of the Booth
The field of audiology can use community support services as an important metric to justify broadening its role in the environment. In 2010, a study by Schneider and colleagues looked at the impact of hearing loss on the use of community support services and reliance on non-spouse family/friends among older people. They found that hearing loss was associated with a 2-fold increased use of community services, with mild to moderate and moderate to severe loss associated with an 80% increased reliance on either formal or informal support.28
Educational audiology is a good example of how the profession facilitates successful functioning by getting out of the booth and assessing the needs of a child in their school environment. According to the WHO framework of disability, hearing loss is the health condition which can affect body functions and structures (e.g., the ear), related activities (e.g., difficulty hearing teacher), and the participation of the individual (e.g., lack of peer to peer learning). By going into the classroom and exploring each student's individual educational environment and their ability to complete specific tasks within this environment, the audiologist is able to improve access to teachers, peers and other audio components of the curriculum.
The need for support by audiologists extends beyond the pediatric population. In age-friendly communities, the policies, services, and structures related to the physical and social environment are designed to help seniors ‘age actively’ in a work place or in the community. The environment should be set up to help seniors live safely and stay involved.29 To identify and manage hearing loss, Weinstein recommends audiologists need to revisit our scope of practice and redirect our professional activities with the adoption of a lifespan approach,30 Audiologists can support age-friendly workplaces and communities by understanding universal design principles and applying them in our clinical work. The Disability Act 2005 defines universal design as “the design and composition of an environment so that it may be accessed, understood and used”:
- to the greatest possible extent,
- in the most independent and natural manner possible,
- in the widest possible range of situations,
- without the need for adaptation, modification, assistive devices, or specialized solutions, by any persons of any age or size or having any particular physical, sensory, mental health or intellectual ability or disability, and
- Means, in relation to electronic systems, any electronics-based process of creating products, services or systems so that they may be used by any person.31
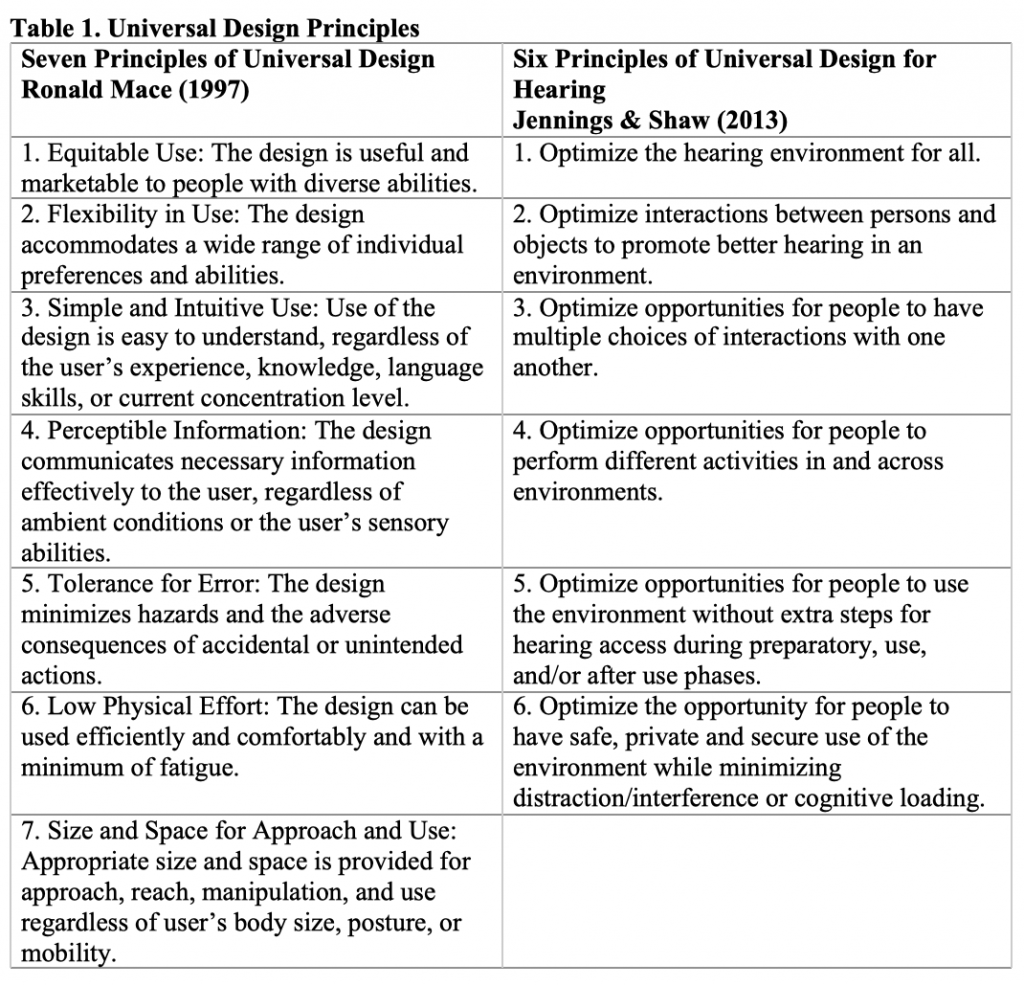
These principles incorporate a two-level design approach; a user-aware and a customizable design. A user-aware design pushes the boundaries of mainstream products, services, and environments to include as many people as possible. A customizable design minimizes the difficulties of adaptation to particular users.32 There are seven general principles of universal design outlined in table one. In 2007, Fok et al modified these principles and adapted them to create a process to examine the barriers and facilitators within the immediate environment, the community and social contexts, the degree and quality of participation, and opportunities for change for people with hearing loss.33 It assesses the communication environment from the perspective of how well the environment can meet the auditory communication needs of the users through a ‘universal hearing accessibility’ lens.34
Audiologists can work as part of a team with government, architects, product and building designers, disability support workers and people who are Deaf/deaf and hard of hearing. This helps support businesses, educational institutions, workplaces, health care settings, and community organizations apply these universal hearing design principles to environmental barriers by focusing on both user-aware and customizable designs. This support can include consultation on policies and procedures, comprehensive site assessments examining the tasks or activities required to perform within a given environment, the demands of the activities, the resources that are available, and suggestions on how to improve function and participation. Examples of solutions other than personal amplification could include assistive devices (e.g., classroom audio distribution systems, loop systems, DM systems, IR systems, alerting devices, portable or fixed counter loop systems), reducing acoustic barriers, adapting how someone performs certain tasks, counselling, and/or educational training to reduce attitudinal and societal barriers. Using the universal design for hearing principles as a framework to ensure auditory communication needs are being met is important since solutions and technologies change over time. As part of a public health approach, these principles can also play an important role in helping communities become age-friendly.
In 2015, Pichora-Fuller, et al reported the importance of adopting a healthy aging perspective that focuses on facilitating active social participation by older adults. These initiatives could “increase awareness of the importance of hearing health, better integrate hearing health care into the larger health care picture, increase uptake of amplification devices and other forms of audiologic rehabilitation, and mandate public policies and environmental accommodations such as ambient noise controls and access to written information in public spaces.”35 This is important for audiology clinics to consider when assessing the services they provide, their business model, and their return on investment. In 2015, Cavitt reported there are disruptive forces that now exist in the marketplace (e.g., Internet retailers, big-box retailers, other healthcare providers getting into the hearing aid business) that are disrupting our current model, yet we have not changed the way the model works.36 A focus on accessibility is the smart thing to do from a retail model perspective because it meets legal requirements of federal/provincial accessibility laws, improves quality of service, improves retention and loyalty, demonstrates corporate social responsibility, creates an advantage over competitors, and improves the bottom line. The Conference Board of Canada reports37:
- The number of Canadians living with a physical disability that impairs their mobility, vision, or hearing will rise from 2.9 million to 3.6 million over the next 13 years, nearly double the pace of the population as a whole.
- Real spending by this group will rise from 14 to 21% of the total consumer market.
- Improvements to workplace access would allow 550,000 Canadians with disabilities to work more, increasing GDP by $16.8 billion by 2030.
Overall, accessibility outcomes are critically affected by the way society positions and views disability. The field of audiology must move beyond the medical model and step out of the booth to better meet the needs of those they serve. One way to do this is to examine ways we can expand our role in the built environment both from a universal design perspective and in providing individual rehabilitative support. With the adoption of both Federal and Provincial accessibility legislation (Manitoba, Nova Scotia, Ontario) there is now greater support to create accessible environments in Canada.38 Creating more positions in public and private practice that extend audiology services to provide more consulting services in environments that cause barriers for people who are Deaf/deaf or hard of hearing such as workplaces, educational settings for children and adults, businesses, nursing homes and community organizations will be essential in improving accessibility.
References
- Mason A and Mason M. Psychologic impact of deafness on the child and adolescent. Prim Care 2007;34:407–26. doi: 10.1016/j.pop.2007.04.003.
- Shield B. Evaluation of the social and economic costs of hearing impairment: a report for Hear-it London: London South Bank University; 2006. Retrieved from https://www.hear-it.org/sites/default/files/multimedia/documents/Hear_It_Report_October_2006.pdf
- Kotby MN, Tawfik S, Azizm and Taha H. Public health impact of hearing impairment and disability. Folia Phoniatr Logop 2008;60:58–63. doi: 10.1159/000114646.
- Karchmer MA and Allen TE. The functional assessment of deaf and hard of hearing students. Am Ann Deaf 1999;144:68–77. doi: 10.1353/aad.2012.0468.
- Venail F, Vieu A, Artieres F, et al. Educational and employment achievements in prelingually deaf children who receive cochlear implants. Arch Otolaryngol Head Neck Surg 2010;136:366–72. doi: 10.1001/archoto.2010.31.
- Schroeder L, Petrou S, Kennedy C, et al.. The economic costs of congenital bilateral permanent childhood hearing impairment. Pediatrics 2006;117:1101–12. doi:10.1542/peds.2005-1335.
- Livingstone G, et. Al. The Lancet Commissions 2017;390(10113) P2673–2734. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)31363-6/fulltext
- World Health Organization. Global costs of unaddressed hearing loss and cost-effectiveness of interventions: a WHO report. Geneva; 2017. Licence: CC BY-NC-SA 3.0 IGO. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/254659/9789241512046-eng.pdf
- Thomson RS, Auduong P, Miller AT, and Gurgel RK. Hearing loss as a risk factor for dementia: A systematic review. Laryngoscope Investigative Otolaryngology 2017;2(2):69–79. http://doi.org/10.1002/lio2.65.
- Weinstein B, Sirow LW, and Moser S. Relating hearing aid use to social and emotional loneliness in older adults. Am J Audiol March 2016(5)54–61. doi:10.1044/2015_AJA-15-0055
- Li C-M, Zhang X, Hoffman HJ, et al. Hearing Impairment Associated With Depression in US Adults, National Health and Nutrition Examination Survey 2005–2010. JAMA Otolaryngol Head Neck Surg 2014;140(4):293–302. Retrieved from http://doi.org/10.1001/jamaoto.2014.42
- Pichora-Fuller MK, Mick P, and Reed M. Hearing, Cognition, and Healthy aging: social and public health implications of the links between age-related declines in hearing and cognition. Semin Hear 2015;36(3):122–39. Retrieved from http://doi.org/10.1055/s-0035-1555116
- Lin FR and Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med 2012;172(4):369–71. Retrieved from http://doi.org/10.1001/archinternmed.2011.728
- Statistics Canada. The 2006 Participation and Activity Limitation Survey: Disability in Canada. Statistics Canada Catalogue no. 12-89-628-X. Ottawa. Version updated Feb 2009. Ottawa; 2010. Retrieved from https://www150.statcan.gc.ca/n1/pub/89-628-x/2009012/fs-fi/fs-fi-eng.htm
- Polatajko HJ, Townsend EA, and Craik J. Canadian Model of Occupational Performance and Engagement (CMOP-E). In Enabling Occupation II: Advancing an Occupational Therapy Vision of Health, Well-being, & Justice through Occupation. EA Townsend & HJ Polatajko, Eds. Ottawa, ON: CAOT Publications ACE; 2007.
- Abrams HB and Kihm J. An Introduction to MarkeTrak IX: A New Baseline for the Hearing Aid Market. Hearing Review 2015;22(6):16. Retrieved from http://www.hearingreview.com/2015/05/introduction-marketrak-ix-new-baseline-hearing-aid-market/
- Areheart BA. When disability isn't "just right": the entrenchment of the medical model of disability and the goldilocks dilemma. Indiana Law J 2008;83(1):Article 5. Retrieved from https://www.repository.law.indiana.edu/cgi/viewcontent.cgi?article=1193&context=ilj
- Solvang P. The emergence of an us and them discourse in disability theory. Scand J Disabil Res 2000;2:3–20. Retrieved from http://dx.doi.org/10.1080/15017410009510749
- Hogsbro K. SIMREB–towards a systematic inquiry into models for rehabilitation. Scand J Disabil Res 2010;12:1–18.Retrieved from http://dx.doi.org/10.1080/15017410903338812
- Barnes C and Mercer G. Disability Volume 19 of Key Concepts. Leeds:Wiley; 2003.
- Jackson MA. Models of disability and human rights: informing the improvement of built environment accessibility for people with disability at neighborhood scale? Laws 2018;7:10.
- The Canadian Association of the Deaf-Association des Sourds du Canada. Deaf Culture vs. Medicalization. July 2015. Retrieved from http://cad.ca/issues-positions/deaf-culture-vs-medicalization/
- Oliver M. The social model of disability: thirty years on, Disability & Society 2013;28(7):1024–26, DOI: 10.1080/09687599.2013.818773
- Söder M. Tensions, perspectives and themes in disability studies, Scand J Disabil Res 2009;11(2):67–81, DOI: 10.1080/15017410902830496
- Campbell J, Oliver M. Disability Politics: Understanding Our Past, Changing Our Future. Abingdon: Routledge; 1996.
- World Health Organization. International classification of functioning, disability and health: ICF. Geneva; World Health Organization; 2001. Retrieved from http://www.who.int/iris/handle/10665/42407
- Tremblay KL. Why is hearing loss a public health concern? Hear J 2017;14–16.
- Schneider J, Gopinath B, Karpa MJ, et al. Hearing loss impacts on the use of community and informal supports, Age and Ageing 2010;39(4)1:458–64. https://doi.org/10.1093/ageing/afq051
- Government of Canada. Age-Friendly Communities; 2016. Retrieved from https://www.canada.ca/en/public-health/services/health-promotion/aging-seniors/friendly-communities.html
- Weinstein B. A life course approach to hearing care – part 1. Hear J 2018;71(1). doi: 10.1097/01.HJ.0000529844.93623.f9
- Disability Act 2005. Number 14 of 2005. Retrieved from http://www.irishstatutebook.ie/eli/2005/act/14/enacted/en/print.html
- National Disability Authority: Centre for Excellence in Universal Design. Definition and Overview; 2014. Retrieved from www.universaldesign.ie/What-is-Universal-Design/Definition-and-Overview/
- Fok D, Shaw L, Jennings MB, and Cheesman M. Universal accessibility and usability for hearing: Considerations for design. Can Acoust 2007;35:3.
- Jennings MB. Hearing Accessibility and Assistive Technology Use by Older Adults: Application of Universal Design Principles to Hearing. In Louise Hickson ed. Hearing Care for Adults 2009- The Challenge of Aging. (pp. 249-254). Proceedings of the Second International Adult Conference. Second International Adult Conference, Chicago, United States, 16-18 November 2009. Staefa, Switzerland: Phonak.
- Pichora-Fuller MK, Mick P, and Reed M. Hearing, Cognition, and healthy aging: social and public health implications of the links between age-related declines in hearing and cognition. Semin Hear 2015;36(3):122–39. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4906310/
- Cavitt K. An Audiologic Care Delivery Model for the 21st Century. Audiologyonline 2015;Feb 23. Retrieved from https://www.audiologyonline.com/articles/audiologic-care-delivery-model-for-13377
- Gibbard R, Desormeaux M, Persaud P, and Wright R. The Business Case to Build Physically Accessible Environments. Conference Board of Canada; 2018. 64 pages. Retrieved from: https://www.conferenceboard.ca/temp/ab4e1174-7848-454e-aa54-7c3ec2c3c8a4/9434_Accessible-Environs_RPT_Accessible.pdf
- Employment and Social Development Canada. Making and Accessible Canada for People with Disabilities; 2018. Retrieved from: https://www.canada.ca/en/employment-social-development/programs/accessible-people-disabilities.html

