The Bidirectional Association between Tinnitus & Mental Well-being: Clinical Implications for Audiologists
In 2019, a health report released by Statistics Canada revealed that approximately 9.2 million adult Canadians, accounting for about 37% of the population, had experienced tinnitus in the past year.1 By analyzing data from the Canadian Health Measures Survey’s (CHMS) cycles 3 and 4, it was also found that the prevalence of tinnitus was notably higher among individuals aged 19 to 29, with a rate of 46%, compared to those aged 30 to 49 (33%) and 50 to 70 (35%).1 One possible explanation for this difference was the increased use of audio devices such as headphones or earbuds and exposure to amplified music and loud noise at events, which were more common among younger people. The CHMS data also revealed that 7% of Canadians with tinnitus reported experiencing the symptoms as bothersome, significantly affecting their mood, sleep, and concentration.1 These findings were consistent with widely accepted figures showing that approximately 15–20% of individuals with tinnitus experience troublesome symptoms.2–5
Living with bothersome tinnitus can prove to be a challenging and isolating experience, causing individuals to wrestle with frustration, irritability, fear, and a decline in their overall well-being.4,5 Over time, the persistent presence of tinnitus can chip away at one’s resilience and ability to function in daily life effectively. This article explores the intersection of bothersome tinnitus and mental health, emphasizing its implications for clinical audiologists as they provide comprehensive care to patients with tinnitus-related distress.
Tinnitus Classification
Tinnitus is the perception of sound in the ear(s) or head without an external sound source.4,5 It is generally classified as subjective or objective tinnitus. For most cases, subjective tinnitus is defined as perceiving a phantom sound, such as ringing, buzzing, hissing, or other sound from within the brain.4 While there is no universal agreement on the neural mechanisms underlying its development, the central gain theory is widely accepted as one of the leading explanations.6,7 According to this theory, damage to the ear includes compensatory homeostatic changes, resulting in an elevation in neural activity observed in different structures of the central auditory system.6,7 These structures include the dorsal cochlear nucleus, thalamus, and auditory cortex. As a result, subjective tinnitus can be triggered by a range of factors, including exposure to loud noise, aging of the auditory system, ear disorders (e.g., otosclerosis, Meniere’s disease), ear injuries and traumas (e.g., tympanic membrane perforation, ossicular chain dislocation), viral and bacterial infections, chronic health conditions (e.g., diabetes, HBP), head and neck tumors, genetic predispositions, and certain medications.3,4,8 Subjective tinnitus is almost always experienced alongside some level of hearing loss. Approximately 80–90% of patients with tinnitus are estimated to experience some degree of hearing loss.8–10 While some patients with tinnitus may show normal pure tone thresholds, they may experience damage to the synaptic junction between cochlear hair cells and auditory nerve fibers, resulting in a loss of synapses.11–13 Research evidence indicates that cochlear synaptopathy or hidden hearing loss may underlie the onset of subjective tinnitus, particularly in individuals exposed to loud noise or amplified music before symptom manifestation.11,12
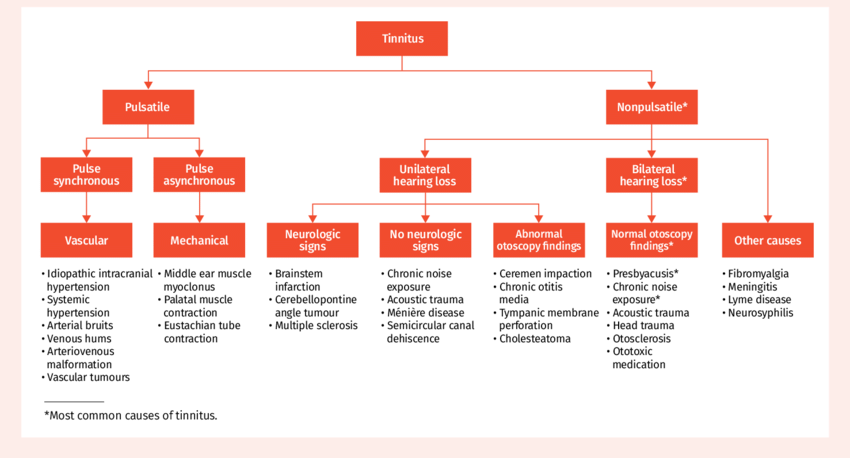
Objective tinnitus is relatively rare, comprising less than 4–5% of all cases, and is typically perceived unilaterally. It involves the perception of real sound originating from within the body. It results from anomalies or dysfunction in the vascular, muscular, skeletal, or respiratory systems.3,4,8 Pulsatile tinnitus, another term for objective tinnitus, can be classified as pulse-synchronous or pulse-asynchronous (see Figure 1).8 Pulse-synchronous tinnitus is commonly associated with vascular diseases (e.g., atherosclerosis and aneurysm), disorders involving irregular blood vessels (e.g., arteriovenous malformation, idiopathic intracranial hypertension), and tumors in the head and neck (e.g., glomus tympanicum). Descriptions of pulse-synchronous tinnitus often include terms like “heartbeat-like”, “throbbing”, “swooshing”, and “rushing”, which capture its rhythmic and pulsating nature. Pulse-asynchronous tinnitus is commonly associated with palatal and middle ear myoclonus, Eustachian tube dysfunction, and temporomandibular joint disorder. Clinicians can sometimes detect pulse-asynchronous tinnitus, frequently described as popping, fluttering, and clicking sound. Patients with pulsatile or objective tinnitus must be referred to medical specialists to ensure accurate diagnosis and appropriate treatment.
Bothersome Tinnitus
Bothersome tinnitus is a condition that significantly affects a patient’s quality of life and is associated with a range of functional, behavioral, and emotional health complications.1,3,4,10 These include difficulties in communication, difficulties understanding speech in noisy environments, reduced sound tolerance conditions (i.e., hyperacusis), an inability to relax, sleep disturbances, irritability, increased stress, anxiety, depression, strained relationship with family and friends and reduced concentration and work performance. Most patients seeking hearing and medical care for symptom relief likely struggle with bothersome tinnitus.
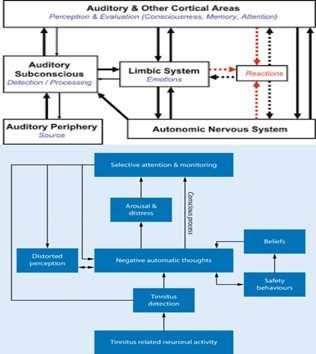
In the last 30 years, several theoretical models have been proposed to explain the emergence of negative reactions to tinnitus symptoms.11–16 Prominent examples include Dr. Pawell Jastreboff’s Neurophysiological model of tinnitus, and Dr. Lawrence Mckenna’s Cognitive-Behavioral model of tinnitus (see Figure 2). Most of these theoretical frameworks suggest that tinnitus-related annoyance and distress are primarily influenced by negative thoughts, worries, misconceptions, and misinformation about the symptoms and their treatments. Moreover, this negative experience is further intensified when relying on maladaptive coping strategies (i.e., safety-seeking behaviors) to alleviate the impact of tinnitus.
The Iceberg Model
The iceberg model is a great clinical tool enabling clinicians and patients to go beyond the surface-level symptom and probe deeper into the underlying root causes of bothersome tinnitus (Figure 3).17,18 It allows clinicians to examine various factors contributing to the severity of the symptoms, some of which may not be immediately evident or readily accessible to patients.

The iceberg model as it relates to bothersome tinnitus can be divided into two interconnected components: auditory and non-auditory (mental health). The tip or visible part of the iceberg represents the auditory component or hearing issues often associated with tinnitus. This includes the perception of ringing, buzzing, or other sounds in the ears or head, hearing difficulty, challenges in understanding speech in noisy environments, and any conditions related to reduced sound tolerance, such as hyperacusis. The submerged or invisible part of the iceberg represents the non-auditory component often associated with the experience of tinnitus. It relates to the often-hidden aspects of patients’ cognitive, behavioral, and emotional responses to tinnitus symptoms. It includes cognitive factors such as misinformation and negative thought patterns, like catastrophizing tinnitus symptoms and fixating on its causes and treatments.4,16,19 It also includes behavioral factors such as maladaptive coping strategies or safety-seeking behaviors that are used by patients to mitigate the impact of tinnitus in their life, like constantly monitoring tinnitus symptoms, overusing earplugs, and avoiding social situations to minimize exposure to loud noise.15,20 And lastly, it includes emotional and behavioral factors or frequently undiagnosed mental health conditions like anxiety, depression, and sleep disorders.4,21,22,23,24
The iceberg model clearly represents the intricate connection between patients’ thoughts, feelings, behaviors, and their influence on tinnitus symptoms. How individuals perceive their tinnitus often shapes their reactions to the symptom(s).
Mental Health
The relationship between tinnitus and mental well-being has long been recognized.19,20,21,22 Just like physical health, mental well-being can change or evolve and be influenced by a variety of factors like life events, genetic predispositions, chronic health conditions, substance use, trauma, childhood experiences, and so on.25,26,27 Mental health issues affect people of all ages, education, income levels, and cultural backgrounds.27 In Canada, it is estimated that approximately 1 in 5 individuals will experience a mental health condition at some stage in their lives.27
Clinicians need to recognize that mental health conditions can impact cognitive processes, emotional regulation, and interpersonal interactions29. Common signs of poor mental health include excessive fear and worry, persistent feelings of sadness and hopelessness, heightened irritability or mood swings, sleep disturbances, chronic fatigue, challenges with concentration, social withdrawal, increased use of substances like alcohol or drugs, and thoughts of self-harm or suicide.30 Bothersome tinnitus has been linked to various mental health disorders, including anxiety, depression, PTSD, and sleep disorders.
- Anxiety Disorders, including generalized anxiety disorders, health anxiety, social anxiety disorder, panic attacks, and obsessive-compulsive disorders, are characterized by an overwhelming sense of fear and worry, often centered around health, specific social situations, challenges at work, and future events.30,31,32 One intriguing aspect of the connection between tinnitus and anxiety is that tinnitus can worsen anxiety symptoms, while anxiety itself can alter the way tinnitus is perceived and experienced. It is estimated that approximately 30–40% of individuals with tinnitus experience an anxiety disorder.23,33,34
- Depression is characterized by persistent feelings of sadness and hopelessness, sleep disturbances, reduced energy, social isolation, and loss of interest. There is also a connection between depression and tinnitus.30,31,34 Tinnitus can also worsen depressive symptoms, while depression itself can exacerbate tinnitus-related distress. It is estimated that approximately 20–30% of individuals with tinnitus experience depression.22,34,35,36
- Post-Traumatic Stress Disorder (PTSD) is characterized by severe distress linked to traumatic experiences.30,31,37 On one hand, tinnitus can trigger distressing and traumatic memories, which can worsen symptoms of PTSD. On the other hand, PTSD symptoms can intensify the perception of tinnitus and also exacerbate tinnitus-related distress.38,39,40 Interestingly, veterans and members of the military, including soldiers and medics, face an elevated risk of developing both tinnitus and PTSD due to their increased exposure to loud noises and combat situations. While we can’t provide precise numbers for the prevalence of individuals with both conditions, research does suggest that a significant portion of military personnel experience both tinnitus and PTSD.38
- Sleep Disorders, including insomnia, sleep apnea, restless leg syndrome, and circadian rhythm disturbances, including jet-lag syndrome are characterized by disruption in sleep patterns and both quality and quantity of sleep.30,31 It is widely acknowledged that tinnitus interferes with sleep, contributing to a higher prevalence of sleep disturbances in individuals with tinnitus, ranging from 40 to 70%, in contrast to 10 to 15% in the general population.41,42
Bidirectional Relationship – A Two-Way Street
A bidirectional association exists between tinnitus-related distress and mental well-being.15,43,44 On one hand, tinnitus can affect an individual’s emotional and behavioral well-being in several ways. The constant presence of tinnitus symptoms can result in increased stress and anxiety, feelings of frustration and sadness, depressed mood, reduced concentration, and both quality and quantity of sleep.3,4,15
On the other hand, emotional and behavioral issues can influence the perception and experience of tinnitus. Individuals with anxiety disorders often experience hyper-vigilance, which heightens their sensory perception.43,44 This increased awareness extends to their surroundings and bodily sensations, including heartbeat, breathing rate, pain, aches, and tinnitus. Depression can also affect the way tinnitus is experienced. Individuals with depression often have fewer coping resources available to manage negative or difficult emotions triggered by the experience.
Unfortunately, a common tendency among patients is to attribute their cognitive, emotional, and behavioral challenges exclusively to their tinnitus, sometimes neglecting the role of their mental well-being as a contributing factor. There’s a prevalent belief that if their tinnitus were to disappear, these issues would go away. However, establishing which condition emerges first, the ‘chicken and egg’ scenario - is not always feasible. Research indicates that both conditions mutually influence each other more often than not.43,44
Guidelines for Comprehensive Assessment
Effectively addressing tinnitus symptoms and associated conditions requires a thorough assessment, extending the evaluation process across three key areas or axes.10 These axes include:
- Axis 1 - Hearing Assessment. A comprehensive understanding of tinnitus symptom(s) relies on a thorough hearing assessment. This involves a detailed case history and in-depth evaluation of the patient’s auditory system. Its aim is to identify the presence of hearing loss and associated conditions including challenges in understanding speech in noisy environments and reduced sound tolerance, such as hyperacusis.45–50
- Axis 2 - Tinnitus Evaluation. The tinnitus evaluation focuses on gathering detailed information about the nature (i.e., subjective or objective), characteristics (i.e., duration, spectral quality, perceived location), and occurrence (i.e., constant, intermittent, occasional) of the tinnitus symptoms, along with its impact on quality of life (i.e., communication difficulty, increase stress, anxiety, depression, sleep disturbances, reduced concentration, poor work performance). It involves a structured interview, completion of standardized self-assessment questionnaires (e.g., Tinnitus Handicap Inventory, Tinnitus Functional Index, Tinnitus and Hearing Survey),51,52,53 and specialized psychoacoustic assessments (e.g., pitch and loudness matching procedures).54–56 The goal is to evaluate the persistent tinnitus sensation and measure its emotional and behavioral impact on the patient.
- Axis 3 - Mental Well-being Screening. The mental well-being screening helps detect potential coexisting conditions, such as increased stress and sleep disturbances that may influence or exacerbate tinnitus symptoms. Recognizing and addressing these factors is essential for developing a comprehensive treatment plan. Figure 4 shows a brief list of clinical tools currently available for audiologists such as the Perceived Stress Scale (PSC), Hospital Anxiety and Depression Scale (HADS), Patient Health Questionnaire (PHQ-9), and Insomnia Severity Index (ISI).57–60 These tools are easy to score and should be given to patients before consultation. If a patient scores high on an anxiety or depression questionnaire, a referral to a mental health professional for assessment, diagnosis, and treatment might take priority over audiological intervention(s).61

Audiologists need to recognize that screening for emotional and behavioral issues, without an established list of referral options (e.g., psychologists, cognitive-behavioral therapists), may unintentionally increase a patient’s stress, worry, anxiety, and depression related to the concern(s). Having this network in place before introducing well-being screening in the clinic is vital to ensure more effective follow-through when additional resources or treatment options are deemed necessary.
Broaching the Topic of Mental Health
Clinicians should approach the topic of mental health with sensitivity, care, and understanding, creating a safe and welcoming environment for patients.62,63 This approach encourages individuals to openly discuss their tinnitus-related distress, facilitating a receptive conversation about the connection between mental well-being and tinnitus, and exploring stress management strategies or counseling.
Furthermore, clinicians need to be cautious about the language they use when discussing mental health. Using sensitive and less triggering terminology helps establish a supportive environment, reduces stigma, and encourages open dialog. Clinicians should focus on cognitive, behavioral, and emotional aspects of well-being, and to avoid terms like “mental illnesses,” “psychological issues,” or “psychiatric disorders.”62,63,64 It’s important to note that audiologists are not authorized to diagnose specific mental health conditions, such as depression or anxiety.
In addressing mental health during discussions about tinnitus symptom management, clinicians may consider the following counseling approaches62,65:
- Inquiring about Well-Being: Initiate the conversation by gently asking about the patient’s emotional and behavioral well-being. Start with questions like, “Have you noticed any changes in your mood, stress levels, or sleep quality since experiencing tinnitus?”
- Normalizing Reactions: Recognize that individuals with bothersome tinnitus often feel irritable, stressed, overwhelmed, and fatigued. Encourage open dialogue by asking, “Can you share any feelings, thoughts, or reactions you’ve experienced due to your tinnitus symptoms?”
- Explaining the Link: Provide information on the bidirectional association between bothersome tinnitus and mental well-being. Help patients understand that tinnitus can affect well-being and vice versa. Explain that research indicates this connection works both ways and may influence the perception and experience of tinnitus symptoms.
- Assessing Coping Strategies: Evaluate how patients are managing their tinnitus symptoms. Open the discussion with, “Given the impact of tinnitus on your stress levels, sleep, and concentration (or even work performance), have you ever explored stress management techniques like deep breathing, relaxation, mindfulness, or considered counseling? If you’re open to it, I can provide you with a list of resources and connect you with specialists who can help manage your tinnitus’s emotional and behavioral aspects.”
- Showing Empathy and Validation: Approach patients hesitant to discuss mental well-being with empathy. Acknowledge their feelings with statements like, “I understand that you might feel uncomfortable discussing this connection. Your emotions are valid, and we can revisit the topic when you’re ready.”
Conclusions
The bidirectional relationship between tinnitus and mental well-being highlights the need for comprehensive audiological care. Given the significant impact of bothersome tinnitus on patients’ quality of life, clinicians gain in exploring the intricate connections within both the auditory and non-auditory (mental health) components of the symptoms. The iceberg model is a valuable clinical tool enabling audiologists to probe into the often-hidden aspects of cognitive, behavioral, and emotional responses to tinnitus. Integrating mental well-being screening with hearing and tinnitus evaluations ensures a thorough approach. When addressing mental health with sensitivity and supportive language, clinicians can facilitate open dialogues, offering personalized treatment options and collaborating with local mental health professionals for better management of both tinnitus-related distress and associated mental health challenges when identified.
References
- Ramage-Morin PL, Banks R, Pineault D, Atrach M. Tinnitus in Canada. Health Rep. 2019 Mar 20;30(3):3-11. doi: 10.25318/82-003-x201900300001-eng.
- Dobie, R.A. (2004) Overview: suffering from tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. Lewiston, New York: BC Decker Inc., 1–7.
- Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, Archer SM, Blakley BW, Carter JM, Granieri EC, Henry JA, Hollingsworth D, Khan FA, Mitchell S, Monfared A, Newman CW, Omole FS, Phillips CD, Robinson SK, Taw MB, Tyler RS, Waguespack R, Whamond EJ. Clinical practice guideline: tinnitus executive summary. Otolaryngol Head Neck Surg. 2014 Oct;151(4):533-41. doi: 10.1177/0194599814547475. PMID: 25274374.
- Cima RFF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, Hoare DJ. A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO. 2019 Mar;67(Suppl 1):10-42. English. doi: 10.1007/s00106-019-0633-7. PMID: 30847513.
- Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990 Aug;8(4):221-54. doi: 10.1016/0168-0102(90)90031-9. PMID: 2175858.
- Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013 Nov 9;382(9904):1600-7. doi: 10.1016/S0140-6736(13)60142-7.
- Henry JA, Roberts LE, Caspary DM, Theodoroff SM, Salvi RJ. Underlying mechanisms of tinnitus: review and clinical implications. J Am Acad Audiol. 2014 Jan;25(1):5-22; quiz 126. doi: 10.3766/jaaa.25.1.2. PMID: 24622858; PMCID: PMC5063499.
- Wu V, Cooke B, Eitutis S, Simpson MTW, Beyea JA. Approach to tinnitus management. Can Fam Physician. 2018 Jul;64(7):491-495. PMID: 30002023; PMCID: PMC6042678.
- Baguley D, Fagelson M. Tinnitus : clinical and research perspectives. Bartnik G M. Managing tinnitus in adults: audiological strategies (pp. 287-308). Plural Publishing (2016).
- Pineault, Dany. (2020, September 24). Assessing and Managing COVID-19 related Tinnitus. Phonak Audiology Blog [Clinical Practice]. https://audiologyblog. phonakpro.com/assessing-and-managing-COVID-19-related-tinnitus/
- Kujawa SG, Liberman MC. Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci. 2009 Nov 11;29(45):14077-85. doi: 10.1523/JNEUROSCI.2845-09.2009.
- Vasilkov V, Caswell-Midwinter B, Zhao Y, de Gruttola V, Jung DH, Liberman MC, Maison SF. Evidence of cochlear neural degeneration in normal-hearing subjects with tinnitus. Sci Rep. 2023 Nov 30;13(1):19870. doi: 10.1038/s41598-023-46741-5. PMID: 38036538; PMCID: PMC10689483.
- Le Prell CG. Hidden versus Not-So-Hidden Hearing Loss. Publication of the Canadian Academy of Audiology (2018).
- Jastreboff PJ, Gray WC, Gold SL. Neurophysiological approach to tinnitus patients. Am J Otol. 1996 Mar;17(2):236-40. PMID: 8723954.
- McKenna L, Handscomb L, Hoare DJ, Hall DA. A scientific cognitive-behavioral model of tinnitus: novel conceptualizations of tinnitus distress. Front Neurol. 2014 Oct 6;5:196. doi: 10.3389/fneur.2014.00196. PMID: 25339938; PMCID: PMC4186305.
- Cima RFF, van Breukelen G, Vlaeyen JWS. Tinnitus-related fear: Mediating the effects of a cognitive behavioural specialised tinnitus treatment. Hear Res. 2018 Feb;358:86-97. doi: 10.1016/j.heares.2017.10.003. Epub 2017 Oct 12. PMID: 29133012.
- Goodman, M. (2002). The Iceberg Model. Innovation Associates Organizational Learning. Hopkinton, MA. Retrieved from https://files.ascd.org/staticfiles/ascd/pdf/journals/ed_lead/el200910_kohm_iceberg.pdf
- Bryan, B.; Goodman, M.; Schaveling, J. Systeemdenken (Systems thinking: discovering our organizational patterns); Academic Service: Cambridge, MA, USA, 2006. Retrieved from https://www.researchgate.net/publication/342420712_sustainability_Safety_Science_a_Systems_Thinking_Perspective_From_Events_to_Mental_Models_and_Sustainable_Safety
- Cima, R.F.F., Crombez, G. & Vlaeyen, J.W. (2011) Catastrophizing and fear of tinnitus predict quality of life in patients with chronic tinnitus. Ear Hear, 32(5), 634–641
- Budd RJ, Pugh R. Tinnitus coping style and its relationship to tinnitus severity and emotional distress. J Psychosom Res. 1996 Oct;41(4):327-35. doi: 10.1016/s0022-3999(96)00171-7. PMID: 8971662.
- Bhatt JM, Bhattacharyya N, Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope. 2017 Feb;127(2):466-469. doi: 10.1002/lary.26107. Epub 2016 Jun 15. PMID: 27301552; PMCID: PMC5812676.
- Salazar JW, Meisel K, Smith ER, Quiggle A, McCoy DB, Amans MR. Depression in patients with tinnitus: a systematic review. Otolaryngol Head Neck Surg. 2019;161(1):28-35. doi: 10.1177/0194599819835178
- Lin CE, Chen LF, Chou PH, Chung CH. Increased prevalence and risk of anxiety disorders in adults with tinnitus: A population-based study in Taiwan. Gen Hosp Psychiatry. 2018 Jan-Feb; 50:131-136. doi: 10.1016/j.genhosppsych.2017.11.006. Epub 2017 Nov 16. PMID: 29190572.
- Izuhara K, Wada K, Nakamura K, et al.. Association between tinnitus and sleep disorders in the general Japanese population. Ann Otol Rhinol Laryngol. 2013;122(11):701-706. doi: 10.1177/000348941312201107
- Centre for Addiction and Mental Health. (n.d.). Mental Illness and Addiction: Facts and Statistics. Retrieved from https://www.camh.ca/en/driving-change/the-crisis-is-real/mental-health-statistics.
- Statistics Canada. (2020). Mental Disorders in Canada. An Infographic. Retrieved from https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2023053-eng.htm
- Public Health agency of Canada. (2009). Mental Illness. Retrieved from https://www.canada.ca/en/public-health/services/chronic-diseases/mental-illness/mental-illness-links.html
- Smetanin et al. (2011). The life and economic impact of major mental illnesses in Canada: 2011-2041. Prepared for the Mental Health Commission of Canada. Toronto: RiskAnalytica. Retrieved from https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/MHCC_Report_Base_Case_FINAL_ENG_0_0.pdf
- Gross JJ, Uusberg H, Uusberg A. Mental illness and well-being: an affect regulation perspective. World Psychiatry. 2019 Jun;18(2):130-139. doi: 10.1002/wps.20618. PMID: 31059626; PMCID: PMC6502417.
- World Health Organization. (2022). Mental Disorders. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-disorders/?gclid=CjwKCAiAibeuBhAAEiwAiXBoJF00QqXejbIFoR4DpqZiBVjEG7wQAqRw8CAWeg8REWyENE3WETdhUBoCDhMQAvD_BwE
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
- Public Health Agency of Canada. (2009). Mental Health - Anxiety Disorders. It’s Your Health. Retrieved from https://www.canada.ca/en/health-canada/services/healthy-living/your-health/diseases/mental-health-anxiety-disorders.html
- Pattyn T, Van Den Eede F, Vanneste S, Cassiers L, Veltman DJ, Van De Heyning P, Sabbe BCG. Tinnitus and anxiety disorders: A review. Hear Res. 2016 Mar;333:255-265. doi: 10.1016/j.heares.2015.08.014. Epub 2015 Sep 2. PMID: 26342399.
- Pierzycki RH, Kitterick PT. Insomnia, Anxiety and Depression in Adult Cochlear Implant Users With Tinnitus. Ear Hear. 2021 Jan/Feb;42(1):235-243. doi: 10.1097/AUD.0000000000000900. PMID: 32568801.
- Public Health Agency of Canada. (2009). Mental Health - Depression. It’s Your Health. Retrieved from https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/hl-vs/alt_formats/pacrb-dgapcr/pdf/iyh-vsv/diseases-maladies/depression-eng.pdf
- Langguth B, Landgrebe M, Kleinjung T, Sand GP, Hajak G. Tinnitus and depression. World J Biol Psychiatry. 2011;12(7):489-500. doi: 10.3109/15622975.2011.575178
- Government of Canada. (2023). Post Traumatic Stress Disorders. Canadian Centre for Health and Disease. Diseases, Disorders, and Injuries. Retrieved from https://www.ccohs.ca/oshanswers/diseases/ptsd.html
- Moring JC, Resick PA, Peterson AL, Husain FT, Esquivel C, Young-McCaughan S, Granato E, Fox PT; STRONG STAR Consortium. Treatment of Posttraumatic Stress Disorder Alleviates Tinnitus-Related Distress Among Veterans: A Pilot Study. Am J Audiol. 2022 Dec 5;31(4):1293-1298. doi: 10.1044/2022_AJA-21-00241. Epub 2022 Aug 24. PMID: 36001823; PMCID: PMC9907433.
- Fagelson MA. The association between tinnitus and posttraumatic stress disorder. Am J Audiol. 2007 Dec;16(2):107-17. doi: 10.1044/1059-0889(2007/015). PMID: 18056879.
- Kreuzer PM, Landgrebe M, Vielsmeier V, Kleinjung T, De Ridder D, Langguth B. Trauma-associated tinnitus. J Head Trauma Rehabil. 2014 Sep-Oct;29(5):432-42. doi: 10.1097/HTR.0b013e31829d3129. PMID: 23982788
- American Psychiatric Association (August 2020). What are Sleep Disorders? Retrieved from https://www.psychiatry.org/patients-families/sleep-disorders/what-are-sleep-disorders#:~:text=There%20are%20several%20different%20types,both%20physical%20and%20emotional%20problems.
- Gu H, Kong W, Yin H, Zheng Y. Prevalence of sleep impairment in patients with tinnitus: a systematic review and single-arm meta-analysis. Eur Arch Otorhinolaryngol. 2022 May;279(5):2211-2221. doi: 10.1007/s00405-021-07092-x. Epub 2021 Oct 27. PMID: 34708282.
- Oosterloo BC, de Feijter M, Croll PH, Baatenburg de Jong RJ, Luik AI, Goedegebure A. Cross-sectional and Longitudinal Associations Between Tinnitus and Mental Health in a Population-Based Sample of Middle-aged and Elderly Persons. JAMA Otolaryngol Head Neck Surg. 2021 Aug 1;147(8):708-716. doi: 10.1001/jamaoto.2021.1049. PMID: 34110355; PMCID: PMC8193541.
- Herr RM, Bosch JA, Theorell T, Loerbroks A. Bidirectionalassociations between psychological distress and hearing problems: an 18-year longitudinal analysis of the British Household Panel Survey. Int J Audiol. 2018 Nov;57(11):816-824. doi: 10.1080/14992027.2018.1490034. Epub 2018 Jul 27. PMID: 30052099.
- Folmer RL, Martin WH, Shi Y. Tinnitus: questions to reveal the cause, answers to provide relief. J Fam Pract. 2004; 53(7):532–540.
- Waechter S. Association between hearing status and tinnitus distress. Acta Otolaryngol. 2021 Apr;141(4):381-385. doi: 10.1080/00016489.2021.1876919. Epub 2021 Feb 19. PMID: 33607935.
- Waechter S, Brännström KJ. Magnitude of extended high frequency hearing loss associated with auditory related tinnitus distress, when controlling for magnitude of hearing loss at standard frequenciesa). J Acoust Soc Am. 2023 Nov 1;154(5):2821-2827. doi: 10.1121/10.0022255. PMID: 37921455.
- Kam ACS. Efficacy of Amplification for Tinnitus Relief in People With Mild Hearing Loss. J Speech Lang Hear Res. 2024 Feb 12;67(2):606-617. doi: 10.1044/2023_JSLHR-23-00031. Epub 2024 Jan 25. PMID: 38271299.
- Oosterloo BC, Homans NC, Goedegebure A. Tinnitus Affects Speech in Noise Comprehension in Individuals With Hearing Loss. Otol Neurotol. 2020 Oct;41(9):e1074-e1081. doi: 10.1097/MAO.0000000000002733. PMID: 32925836.
- Aazh H, Moore BCJ. Prevalence and Characteristics of Patients with Severe Hyperacusis among Patients Seen in a Tinnitus and Hyperacusis Clinic. J Am Acad Audiol. 2018 Jul/Aug;29(7):626-633. doi: 10.3766/jaaa.17015. PMID: 29988010.
- Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol. 1998 Apr;9(2):153-60. PMID: 9564679.
- Meikle MB, Henry JA, Griest SE, Stewart BJ, Abrams HB, McArdle R, Myers PJ, Newman CW, Sandridge S, Turk DC, Folmer RL, Frederick EJ, House JW, Jacobson GP, Kinney SE, Martin WH, Nagler SM, Reich GE, Searchfield G, Sweetow R, Vernon JA. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012 Mar-Apr;33(2):153-76. doi: 10.1097/AUD.0b013e31822f67c0. Erratum in: Ear Hear. 2012 May;33(3):443. PMID: 22156949.
- Henry JA, Griest S, Zaugg TL, Thielman E, Kaelin C, Galvez G, Carlson KF. Tinnitus and hearing survey: a screening tool to differentiate bothersome tinnitus from hearing difficulties. Am J Audiol. 2015 Mar;24(1):66-77. doi: 10.1044/2014_AJA-14-0042. PMID: 25551458; PMCID: PMC4689225.
- Vernon, J. A., & Meikle, M. B. (1988(. Mesurement of tinnitus: an update. In M. Kitahara (Ed.), Tinnitus. Pathology and management (pp. 36-52). Igaku-Shoin.
- McNeill C, Távora-Vieira D, Alnafjan F, Searchfield GD, Welch D. Tinnitus pitch, masking, and the effectiveness of hearing aids for tinnitus therapy. Int J Audiol. 2012 Dec;51(12):914-9. doi: 10.3109/14992027.2012.721934. Epub 2012 Nov 5. PMID: 23126317.
- Simonetti P, Vasconcelos LG, Gândara MR, Lezirovitz K, Medeiros ÍRT, Oiticica J. Hearing aid effectiveness on patients with chronic tinnitus and associated hearing loss. Braz J Otorhinolaryngol. 2022 Nov-Dec;88 Suppl 3(Suppl 3):S164-S170. doi: 10.1016/j.bjorl.2022.03.002. Epub 2022 May 20. PMID: 35729042; PMCID: PMC9761006.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983 Dec; 24(4):385-96. PMID: 6668417.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun; 67(6):361-70. doi: 10.1111/j.1600-0447.1983.tb09716.x. PMID: 6880820.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep; 16(9):606-13. doi: 10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941; PMCID: PMC1495268.
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001 Jul; 2(4):297-307. doi: 10.1016/s1389-9457(00)00065-4. PMID: 11438246.
- Pineault, D. (2021). Impact of COVID-19 Pandemic on Mental Health and People with Hearing Problems, The Hearing Journal: March 2021 - Volume 74 - Issue 3 - p 6.
- Graham, B. (2022, November 10). How can We Normalize Talking about Mental Health. The Paper Gown. Retrieved from https://www.zocdoc.com/blog/how-can-we-normalize-talking-about-mental-health/
- Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Health Manage Forum. 2017 Mar; 30(2):111-116. doi: 10.1177/0840470416679413. Epub 2017 Feb 16. PMID: 28929889; PMCID: PMC5347358.
- Substance abuse and Mental service Administration. (n.d.). How to talk about Mental Health. U.S. Department of Health and Human services. https://www.samhsa.gov/mental-health/how-to-talk
- Pineault, Dany. (2028, September 8). Counseling Strategies for Bothersome Tinnitus. Phonak Audiology Blog [Clinical Practice]. https://audiologyblog.phonakpro.com/counseling-strategies-for-bothersome-tinnitus/


