Hearing Aid Use for Patients with Posttraumatic Stress Disorder
Posttraumatic stress disorder (PTSD) is a constellation of clinical signs and symptoms that affect individuals who survive traumatic events during which their physical integrity is threatened, they are held captive, or lives are lost.1 Perpetrators of violence and trauma may also develop PTSD.2 The defining behaviors of PTSD according to the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-V; 2013) are summarized in Table 1, and include re-experiencing the event through spontaneous memories, dreams or flashbacks of the trauma; avoidance of environments or circumstances that recall the event; negative thoughts or mood including blame of self or others; and heightened stress arousal (i.e., the “fight or flight” response) that presents as hypervigilance, disturbed sleep, and aggression.3 Shay recommends that PTSD be considered a psychological injury in order to capture more clearly the destruction of a victim’s character, the prolonged and durable effects of trauma that can “wreck the personality.”4
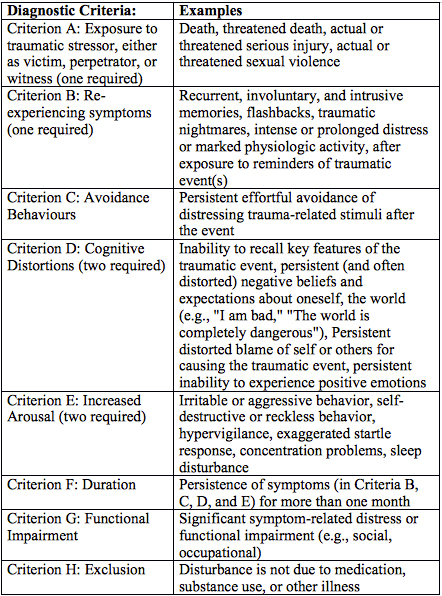
Table 1. Diagnostic Markers for PTSD (DSM V; American Psychiatric Association)
Individuals of all ages, from all socio-economic backgrounds who experience traumatic events, prolonged abuse or captivity are at-risk for developing PTSD. Additionally, trauma endured before the age of 10 increases the likelihood of a patient developing PTSD later in life.5 Patients are more likely than the general public to battle substance abuse and chronic health problems.1,6 With respect to auditory effects, exaggerated startle responses, hyperacusis, and tinnitus are more common and rated as more severe among patients with PTSD than those without, even when patients without PTSD suffer from depression or other psychological disorders.7,8
Exposure to damaging sound pressure levels often is associated with traumatic events in military and veteran populations. Similar noise levels may affect many civilians who develop PTSD as a result of motor vehicle accident, or as a result of an event that produces closed-head injury or mild traumatic brain injury (mTBI). Resulting auditory and vestibular dysfunction is often similar to that of a combat veteran. Therefore, although this paper will review results primarily from veteran’s affairs clinical activity, the results can inform work in more diverse clinical settings.
Patients with PTSD may experience sensory distortions, and their hypervigilance fosters insecurity because they may believe that their senses are not reliable.6 Against such a backdrop, it is reasonable to expect that improved awareness and audibility of the acoustical environment through hearing aids or other assistive devices would be therapeutic and beneficial to individuals with PTSD.
Justification for hearing aid use, as with any patient, should be focused on quality of life issues and improvement of auditory performance. Patients with PTSD often remind us that such issues revolve as much around the sense of security in their environment as communication. A few specific symptoms from the DSM-V suggest that patients should benefit from improved audibility for environmental events. For example, the stressor’s (Criterion A, see Table 1) enduring influence may manifest as marked physiologic reactivity, such as increased heart rate, panic, or powerful sympathetic nervous system symptoms, after exposure to trauma-related stimuli. Other symptoms relate to re-experiencing the trauma when the environment resembles, or recapitulates the environment experienced during the trauma. For example, an individual who startles, or physically lashes out in response to an innocuous stimulus, such as silverware dropped in a restaurant, has in some way mislabeled the sound as a potential threat. Such mislabeling or misinterpretation of environmental events is an important symptom of PTSD. Patients receiving services in a tinnitus clinic who suffer from PTSD are more likely to report sound tolerance problems than patients without PTSD. In more than half the cases, the patients with PTSD rate the sound tolerance issues as more severe than their tinnitus.7 Although hearing aids may increase the startle response in some patients, improved audibility provided by a fitting approach that carefully selects and controls output and is tailored specifically to the patient’s limitations should contribute to a sense of control in challenging social situations. Although a patient’s exaggerated startle response may endure, sound tolerance issues may be reduced over time.9
Because PTSD often develops after exposure to violent acts, blasts, head trauma, and other powerful stressors, patients often experience tinnitus in addition to hearing loss. The effects of tinnitus and PTSD may be mutually reinforcing as patients with tinnitus rate PTSD as more severe than those without tinnitus,10 and patients with PTSD rate their tinnitus as more severe than those without PTSD.7 Therefore, when hearing loss is present, several factors may contribute to the benefits of amplification. First, audibility of speech sounds should be improved, thereby facilitating communication and reducing listening strain. Second, the improved audibility of ambient sounds may foster complete or partial tinnitus suppression, and ultimately influence in a positive way the auditory pathway changes responsible for tinnitus maintenance. Finally, hearing aids can foster the patient’s sense of security as sounds in the environment could be detected more easily and accurately than when the patient is unaided.
Searchfield offers guidelines for programming hearing aids to maximize their utility for patients with tinnitus; these settings often benefit patients whose tinnitus is complicated by the presence of PTSD.11 Searchfield’s approach pursues tinnitus amelioration through improved audibility in a variety of listening situations while prioritizing outputs that cannot exceed the patient’s tolerance limits. Controlling output is especially important for patients with PTSD in order to minimize sound tolerance issues. The programming establishes a “tinnitus setting” that includes omnidirectional microphone, no noise suppression, expansion options disengaged, and wide dynamic range compression with a low (20–40 dB SLP) kneepoint that provides access to environmental sounds without producing excessive loudness. Target gain values associated with higher levels of low-frequency gain, such as DSL[i/o] should be employed. A second program would provide essentially the opposite characteristics: target gain set to NAL-NL1 or NL2 to maximize audibility of the speech spectrum, directional microphone, noise suppression engaged, and expansion or soft squelch engaged. Searchfield recommends an open fit device whenever possible to avoid occlusion that might increase tinnitus awareness.
The efficacy of hearing aids for patients with the most severe tinnitus is encouraging. Table 2 shows rates of patient reports from our Veteran’s Affairs clinic indicating benefit from hearing aid use. Note that patients with tinnitus and PTSD report that hearing aids benefit tinnitus more frequently than do patients with tinnitus and other psychological disorders. Patient reports suggest that the ability to monitor the environment in some cases trumps improvements in audibility that facilitate communication. Perhaps more reliable monitoring decreases the patient’s stress arousal, and as a result, reduces the negative effects of tinnitus. Therefore, the optimal fitting approach for such patients may need to prioritize loudness tolerance and the need to enhance the patient’s ability to monitor their environment consistently rather than improved speech understanding.
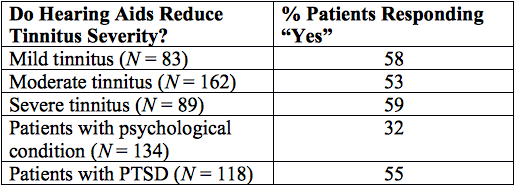
Table 2. Reduction of Tinnitus Severity Associated with Hearing Aid Use By Patient Report. PTSD = posttraumatic stress disorder
Although fitting hearing aids to patients with loudness tolerance issues is a challenge, audiologists have much to offer patients whose lives are influenced by the enduring and disorienting effects of trauma. A hearing aid’s potential benefits for patients affected by PTSD appear to outweigh the risks given that output can be controlled effectively, and tailored specifically for the patient’s limitations. While there is great value in restoring audibility to facilitate communication, it may be that some patients benefit more from the ability to monitor their environment more consistently and accurately. Awareness and consideration of the special needs of patients with PTSD – the increased need to monitor the acoustical environment, manage exaggerated startle response to sound, decreased sound tolerance, and tinnitus – will enhance the role of the audiologist in their care.
REFERENCES
- Herman JL. Trauma and recovery. New York, NY: Basic Books; 1997.
- Lifton RJ. The Nazi doctors. New York, NY: Basic Books; 1986.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing; 2013.
- Shay J. Achilles in Vietnam: The undoing of character. New York, NY: Scribner; 1994.
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults; J Consult Clin Psychol 2000;68(5):748–66.
- Schnurr PP and Jankowski MK. Physical health and posttraumatic stress disorder: Review and synthesis. Semin Clin Neuropsychiatr 1999;4:295–304.
- Fagelson MA. The association between tinnitus and posttraumatic stress disorder. J Am Acad Audiol 2007:16;107–17.
- Smith SL, Fagelson M. Development of the self-efficacy for tinnitus management questionnaire. J Am Acad Audiol 2011;22(7):424–40.
- Formby C and Gold SL. Modification of loudness discomfort level: evidence for adaptive chronic auditory gain and its clinical relevance. Semin Hear 2002;23(1):21–34
- Hinton DE, Chhean D, Pich V, Hofmann SG and Barlow DH. Tinnitus among Cambodian refugees: Relationship to PTSD severity. J Traumatic Stress, 2006;19:541–546.
- Searchfield G. Hearing aids and tinnitus. In: Tyler R, ed. Tinnitus treatments: Clinical protocols. New York, NY: Thieme; 2006.


