The Quick and Dirty on Hyperacusis
Noise is unwanted sound, like your neighbour playing bad 80s music late at night. For our hard-of-hearing patients, sound quickly becomes “noise” when it interferes with their ability to hear speech. For clients with hyperacusis, however, offending noises include everyday sounds that are typically well-tolerated. These sounds are unwanted because they are perceived as unacceptably loud or because the sounds elicit discomfort or pain, annoyance, distress, and even fear.
Baguley and Andersson define hyperacusis as “the experience of inordinate loudness of sound that most people tolerate well, associated with a component of distress.”1 (for a discussion of current directions in terminology, see Aazh H, McFerran D, Salvi R, Prasher D, Jastreboff M, Jastreboff P. Insights from the first international conference on hyperacusis: Causes, evaluation, diagnosis and treatment. Noise Health [serial online] 2014 [cited 2015 Feb 8];16:123-6. Available from: http://www.noiseandhealth.org/text.asp?2014/16/69/123/132100).
According to this definition, hyperacusis includes (1) an auditory component, specifically increased auditory gain that contributes to alterations in the perception or acceptability of moderately loud sounds, and (2) a psychological component described as an aversive, emotional reaction to sound accompanied by pronounced stress arousal.
Increased central auditory gain is believed to arise from neuroplastic changes resulting in disinhibition or over-excitation of auditory neurons in the auditory pathways. The psychological component of hyperacusis is attributed to engagement of non-auditory areas of the brain responsible for arousal, fear and attention.
Hyperacusis is distinct from recruitment which is increased loudness growth due to changes in cochlear function.
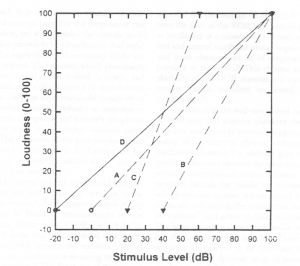
Figure 1. Idealized schematic contrasts the (A) normal loudness growth function with abnormal loudness growth functions typical of (B) a cochlear recruitment deficit (C), hyperacusis and (D), and super-sensitivity.2
Figure 1 shows a hypothetical loudness growth function for normal hearing (line A), cochlear loss with recruitment (line B) and hyperacusis (line C).2 Hyperacusis is a central phenomenon, subject to variations in stress arousal, and one that can be reversed; whereas recruitment is a peripheral phenomenon that does not vary with arousal state or treatment.
Prevalence estimates of hyperacusis in the general population vary from 2–3%. In tinnitus clinic patients, however, the prevalence is between 40–79%.1 Hyperacusis may develop prior to, concurrent with, or after tinnitus onset. Approximately half of individuals with hyperacusis have hearing loss.
Patients with hyperacusis are typically bothered by moderately intense, high-frequency and/or percussive sounds such as dishes clattering or reversal beeps on trucks. Sometimes the culprit is continuous sound such as computer fans, refrigerator compressors in grocery stores or running water. If tinnitus is present, patients with hyperacusis report tinnitus that worsens for minutes to days following exposure to doses of sound that would be considered safe as per occupational guidelines. Individuals with decreased sound tolerance may also report increased awareness of sounds and an exaggerated startle response to unanticipated sounds.
In addition to sound–induced discomfort, many affected individuals go out of their way to avoid sounds or situations that might provoke hyperacusis or tinnitus. They may report using hearing protection to feel safe and avoid exposure. At work they may wear both ear plugs and ear muffs, a practice that ironically limits their ability to hear important warning signals and compromises safety. Most researchers agree that such patients ultimately overuse hearing protection.
Hyperacusis can be a significant contributor to rejection of amplification. We often see that the frequencies that are least well tolerated overlay the frequencies at which hearing thresholds are poorest. Hyperacusis will result in a lower MCL, and hearing aids set accordingly will go into compression more frequently. Amplification set to target gain may be uncomfortable, increase existing tinnitus, and contribute to physical tension.
I often find that patients with hyperacusis report a long-standing dislike of sound or a history of auditory vigilance. Examples of this are patients who report a history of trauma, abuse, of growing up in house where children were expected to be very quiet (usually when one parent needed to sleep during the day), or those who report the need to monitor sound in their jobs (e.g, law enforcement officers).
So how do we help our patients with hyperacusis? There is still very little evidence to guide best practice. Here are some tips on clinical management and rationale for practice based on our current understanding of hyperacusis and clinical experience:
- Counsel patients about safe levels of sound. They appreciate knowing that even if sounds are uncomfortable, the sounds that bother them are not necessarily doing any permanent damage to their ears or auditory system. If others around them are not obviously physically uncomfortable or holding their ears, then the patient probably does not need to worry about the sound causing damage to his or her ears.
- Explain the mechanism of hyperacusis. I often tell patients that their ears are overly sensitive because the brain’s volume control is stuck on “high,” making incoming sound uncomfortably loud. Our job is to loosen the volume control and bring it back down to a normal setting, or to recalibrate central auditory gain.
- Encourage patients to slowly wean themselves off of hearing protection not required for hearing loss prevention. A study by Formby et al. found that subjects using ear plugs throughout the day developed decreased sound tolerance, suggesting that inappropriate use of hearing protection may trigger or exacerbate hyperacusis.3
- Encourage your patients to gradually increase exposure to sound in safe and fairly predictable environments. Hyperacusic patients need to feel that they are not trapped in a situation that they find intolerable as this will increase stress arousal and enhance their negative response to sound. For some this may mean increasing sound exposure at home before venturing outside. For others it may mean returning to difficult situations with an escape plan or ear plugs that can be worn “just in case.”
- Depending on the severity of hyperacusis, some hearing-impaired patients will need to delay or limit use of amplification until their sound tolerance has improved. Amplification will need to be gradually increased over several months before reaching target gain. It is important that your client understands that their instruments will not provide the full benefit for hearing loss until sound tolerance has improved.
- Severe cases of hyperacusis may require use of sound generators to reduce the contrast between offending sounds and background sound. Clients usually enjoy the “buffering” effect of using sound generators. Furthermore, use of low-level sound generators prior to or in conjunction with introduction of amplification may allow hearing aid users with hyperacusis to better tolerate amplified sounds,4,1, and possibly facilitate recalibration of central auditory gain. Fortunately, many manufacturers now provide sound generator options with their instruments.
- Marshall Chasin has developed a clever desensitization exercise using a piano. "A three-finger approach to hyperacusis".
- Good quality electronic ear muffs such as the Peltor Tactical Pro (class A) or Bilsom Impact provide (class B) hearing protection for sounds above 82 dBA. At lower sound levels, they provide mild amplification. These are appropriate for hyperacusis and tinnitus patients exposed to intermittent noise at work or at home and will help them to avoid overuse of hearing protection.
- Keep in mind that hyperacusis has a psychological component. Psychological intervention may be warranted to address the emotional component of hyperacusis as well as any comorbid anxiety or depression that can contribute to sound intolerance. Cognitive behavioural therapy (CBT) can help clients learn to identify and change negative automatic thinking about sound, although finding a CBT-trained knowledgeable about hearing disorders can be a challenge.
- I frequently refer clients who complain of sound-induced ear pain/discomfort and transient aural fullness to a physiotherapist certified in temporomandibular disorders and cervical treatment, especially where there is history of head or neck injury. Prior medical assessment of otalgia and aural fullness is necessary to rule out any serious medical problems that could contribute to these symptoms.
I view recovery from hyperacusis much like recovery from a concussion. The pace and degree of recovery varies from person to person. Recovery may happen over weeks or months. It may improve with “auditory rest” or may require specific intervention. Hyperacusis may resolve completely or there may be lingering sensitivities that require modifications to lifestyle or work. As audiologists, we can help our clients to understand their reaction to sound and, with the right tools, help them to increase sound tolerance and enjoy the world of sound again (with the exception of neighbours’ questionable choice of music).
References
- Baguley D and Andersson G. Hyperacusis: mechanisms, diagnosis, and therapies. Plural Publishing: San Diego; 2007.
- Tyler RS. The use of science to find successful tinnitus treatments. In: Proceedings of the Sixth International Tinnitus Seminar (3-9). London: The Tinnitus-Hyperacusis Center; 1999.
- Formby C, Sherlock LP, and Gold SL. Adaptive plasticity of loudness induced by chronic attenuation and enhancement of the acoustic background. J Acoust Soc Am 2003;114:55–58.
- Formby C, Hawley M, and Sherlock LP et al. Intervention for restricted dynamic range and reduced sound tolerance: Clinical trial using a Tinnitus Retraining Therapy protocol for hyperacusis. Proceedings of Meetings on Acoustics, 19, 050083; 2013. DOI:http://dx.doi.org/10.1121/1.4799870.

