Striking the Right Balance: Current Fall Prevention Strategies in Audiology Practice: A Review of the 2017 CAA Fall Prevention Survey Results
In this edition of “Striking the Right Balance,” Jillian Baxter, Lauren Dunphy, and Dana Song, Audiology students at the School of Human Communication Disorders at Dalhousie University along with Audiologists Michael Vekasi and Janine Verge discuss current fall prevention strategies in audiology practice and review the CAA National Vestibular Special Interest Group's fall prevention survey results.
If you are a health care professional and would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by emailing CAAvestibular@gmail.com to let us know you want to be included. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
‘Help, I’ve fallen and I can’t get up!’ This famous 1980’s catchphrase from the Lifeline Alert System commercial quickly became a humorous quote used by many teens and young adults (http://www.lifealert.com/). Despite the comical connotation associated with the advertisement, it touches on a very serious matter and the focus of this article: falling.

Falls are a public health crisis, with an estimated one third of Canada’s seniors expected to experience a fall within the next year.1 Additionally, half of Canada’s long-term care facility residents fall annually, resulting in a serious injury in one out of 10 people.1 The Public Health Agency of Canada defines a fall as “a sudden and unintentional change in position resulting in an individual landing at a lower level such as on an object, floor or the ground, with or without injury.”2 Seniors aged 65 and older are at the greatest risk of falling. More so, seniors in long-term care facilities or persons with cognitive impairment or dementia are at an even greater risk.3 Falls are the leading cause of hospitalization for children, young adults and seniors.2 Therefore, fall prevention is important for people of all ages, not specifically only for seniors. Falls are associated with detrimental physical, mental and financial consequences, which is why it is important for health professionals, including audiologists, to get involved in fall prevention.
The physical consequences of sustaining a fall can be severely debilitating and are linked with morbidity, mortality and poorer overall functioning.4 These consequences are often reflected in patient reports about falls: “My grandmother fell down and broke her hip” or “My father had a bad fall and had to be put in a nursing home.” Falls are the leading cause of hip fractures in Canadians. About 95% of hip fractures are caused by falls, with 20% of those falls resulting in death.2 Deaths from falls have increased by 65% from 2003 to 2008, and is estimated to continue to increase, providing a greater reason to get involved in fall prevention.2
Falls have serious mental health consequences. Following a fall, many patients will develop a fear of falling. This fear is not unwarranted; a history of falls is a strong predictor of future falls. Seniors who have suffered a fall are 3 times more likely to fall again within the following year.2,4 The fear of falling produces a negative feedback loop that begins with the initial fall, leading to reduced confidence in their balance and can result in reduced physical activity. This increases the chances of the patient sustaining another fall.5 Reduced activity associated with a fear of falling or physical injury has been linked to negative mental health consequences including feelings of isolation, and depression.2 In addition, fall related injuries can lead to a loss of independence. Approximately one third of seniors hospitalized for a fall will be placed in a long-term care facility. This loss of independence can result in confusion, as well as other mental health issues.2
There are also health care costs associated with falls, which includes emergency department visits, hospitalizations, and long-term care facility placements. Medical expenses, as a result of falls, cost an estimated $2 billion annually.2 Approximately 67% of Canadian seniors who experienced a fall were rushed to the emergency department due to the injuries sustained.2 On average, a hospital visit as a result from a fall is 9 days longer than a hospital visit for any other cause. In addition, the costs associated with support for those who require admittance to long-term care facility places stress on Canada’s health care system.2 Furthermore, it is anticipated that health care costs associated with falls will continue to increase due to Canada’s aging demographic. An estimated 25% of the Canadian population will be 65 or older by the year 2036.2 Fall prevention is necessary to help alleviate the physical, mental and financial costs on the individual and on the health care system.
As health care professionals, we should be proactive in assisting our current and future patients in preventing harm or injury, including falls. Falls can have a detrimental effect on our social, physical and mental wellbeing, and can be actively addressed through fall prevention awareness and clinical applications. Fall prevention can help reduce severe fall related injuries, hospitalizations, nursing home placements and also functional decline.3
Fall Prevention
What exactly do we mean when we refer to the term fall prevention? Fall prevention involves assessment of fall risk and/or previously sustained fall(s), intervention, management, and education. It is recommended that older adults who have a history of previous falls, gait and/or balance problems should receive a multifactorial fall risk assessment.1 This assessment should include examination of their feet and footwear, functional assessment, measures of perceived functional ability and fear related to falling.3 The Falls Behavioural (FaB) Scale for the Older Persons is an example of an assessment tool (5–10 minutes) that can be used to measure behaviours that can lead to increased fall risk in an individual.6 Additionally, this tool can assist the inter-professional team in developing exercises to help protect the individual from future falls or near-falls.
There are many different aspects of fall prevention intervention. This includes environmental adaptation or modification, exercise adaptation, medication reduction or withdrawal, postural hypertension, vitamin D, treating vision impairment and hearing impairments, cardiac pacing, managing foot and footwear problems, and education.1,3,4 Since balance is an integral component of our daily functioning, the intervention stage of fall prevention should involve other health professionals (i.e., physiotherapists and/or occupational therapists) to ensure thorough care for the individual.
It is crucial that we have an understanding about the numerous risk factors linked to falls in order to prevent falls and develop appropriate intervention strategies for our patients. These risk factors include the individual's current health status, behaviour, environment, and social situation.2 The current health status of the patient involves bone health, chronic illness such as diabetes, cognitive impairments such as dementia, vision and hearing, balance and gait, and muscle weakness or numbness.2,4 Health behaviours include whether the individual uses an assistive device, alcohol consumption, if they wear proper footwear, adequate diet, use of medications, and risky behaviours such as using a ladder.2,4,7 The individual's social situation is also very important. Having a strong social network of family and friends is linked to lower fall rates.2 In addition, low socioeconomic status is linked to poorer environment, diet, and creates barriers in accessing health care, which can increase the likelihood of sustaining a fall.2 Lastly, environmental risk factors are perhaps the most important to consider. About 40–60% of falls are related to environmental factors such as rugs, electrical cords, poor lighting, weather and climate, stairs and uneven surfaces.2,4
An environmental assessment can be extremely helpful to ensure safety within the home. The most common place for seniors and older adults to experience a fall is within their own home, such as in the shower or on the stairs.8 To ensure safety and comfort, it is important to identify fall risk factors that may exist within or around their home. This may include modifications such as removal of rugs or obstacles from the floor, ensuring adequate lighting inside and outside, installation handles and railings (especially in the bathroom or on stairs), adequate footwear (avoidance of slippery, unstable or flat soles), use of nonslip mats in the bathroom or kitchen, use of contrasting colour steps, use of a walker or wheelchair and the installation of a first alert system.1,4 These are just some examples of adaptations and modifications that will lead towards a safer home environment reducing the risk of falls and associated issues.
Audiologists and Fall Prevention
Fall prevention is within the scope of practice of audiologists based on numerous studies linking the patient population we see, those with hearing and vestibular impairment, with being more at risk of falls. Hearing impairment and audiology clinic visits are related to an increased fall risk and documented falls.9 Compared to individuals with no noted impairments, individuals with hearing impairments are associated with a significantly greater risk of developing chronic health problems (arthritis, depression, high blood pressure, high cholesterol and vision issues) that can contribute to an increased risk of falling.9 For example, arthritis, high blood pressure and high cholesterol may contribute to decreased physical activity, leading to muscle weakness, putting the individual at a greater risk of falling. Hearing loss and depression is suggested to lead to social isolation and cognitive decline, which is noted to be an additional risk factor for falls.5 With regards to chronic dizziness or imbalance, older seniors with these symptoms are 2 to 3 times more likely to fall compared to older people who do not experience these issues.10
There are multiple studies that provide evidence supporting the link between hearing impairment and an increased fall risk. A meta-analysis of 13 studies showed that there were a greater number of falls documented in participants with hearing loss relative to participants with normal hearing.11 Overall, this meta-analysis concluded that falls were 2.39 times more likely in participants with hearing loss than with normal hearing.11 Another study noted that 50% of the patients seen in an audiology clinic reported at least one fall one year prior to the appointment.5 More specifically, 68% of audiology patients reported a recent fall within the last 12 months compared to 28% of non-audiology patients.5 These audiology patients were also more likely to report multiple falls within the year (64.7% compared to 42.9%).5 An additional study conducted demonstrated that for every 10dB increase in PTA thresholds, a history of falls was 1.4 times more likely to be present in individuals aged 40–69 years old.12 Overall, the evidence suggests that fall risk increases with greater severity of hearing loss and hearing loss prevalence increases with age.5 The majority (83%) of the audiological clinical caseload are patients who are aged 60 years old or greater.9 This suggests that a majority of the patients an audiologist would attend to may be at a risk of falling. Therefore, it is important that we screen for fall risk and provide the appropriate intervention to help prevent future falls.
Based on our training and scope of practice, and the fact that our primary patient population is particularly at risk for falls, we as audiologists are in a prime position to take steps to prevent falls. While time in any appointment is a scarce resource, some of these steps take virtually no time at all, such as simply observing the patient’s behaviour and appearance.
- Does the patient appear generally able to take care of themselves?
- Do they keep scheduled appointments?
- Are they maintaining their hearing aids in the manner you would expect?
- Do they appear healthy?
- How does their cognition and memory seem?
- Do they shuffle their feet as they navigate around the office, or do they need to rely on someone or something for support?
Taking a quick mental note of some of these factors can help alert you to any red flags that suggest the patient may be at risk of falls
Additionally, including a few simple questions on the case history can be a very easy way to gather some information about a patient’s fall risk. Questions can be simple and direct, such as “Do you get dizzy?”, or “Have you ever fallen?”, or subtler, such as “Do you live alone?”, “Is it easy to reach your phone when you are at home?”. A quick scan of the case history form can help you decide whether you should proceed with a more detailed screening tool, or possibly make a referral to another health professional.
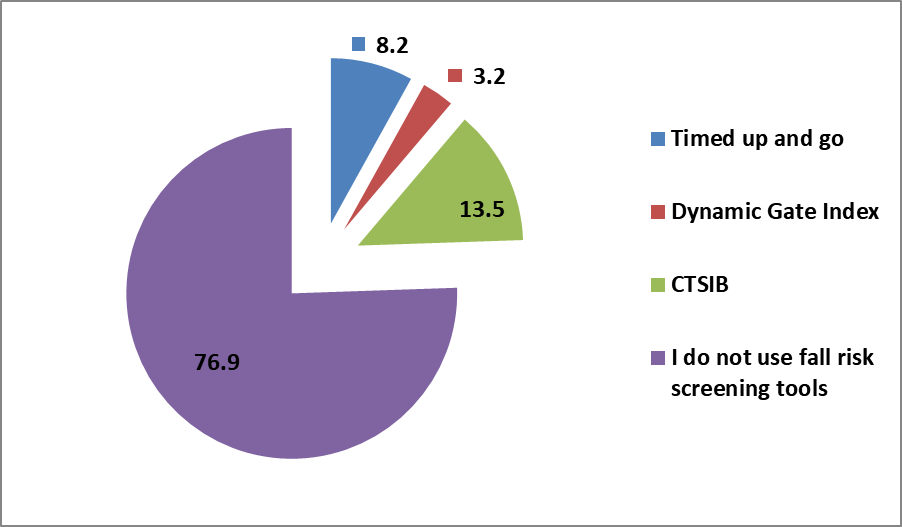
If during your observation of the patient and the case history you believe that the patient may be at risk for falls, there are several quick measures you can administer to quantify their risk of falling. There are many simple vestibular screening tools that can be done quickly, and with very little equipment and space. Some are physical assessments such as the Timed Up and Go13 or the Dynamic Gate Index.14 Others are simply questionnaires that probe further into the patient’s fall risk and/or cognitive functioning. Forms like these can even be filled out before the patient’s appointment in order to save time.15
Lastly, a good counselling session is one of the most important and valuable tool that can be used to prevent falls. When possible, family members should be included in this counselling session. As always, it is important not to scare patients, but to educate them on the seriousness of falls, and the importance that steps be taken to prevent them. Families may not be aware of emergency services such as Life Alert, or other communication strategies. For example, a small cell phone could be kept with the patient at all times, in the event that they fall and cannot reach a land line3. It can also be helpful to discuss the importance of keeping active, preventing osteoporosis, and talking to their pharmacist or family doctor if they are prescribed any medications that can increase fall risk. Handouts can be very helpful as well, so that the patient can review the information after they leave your office.
The purpose of the current study was to find out what steps Canadian audiologists are currently taking to prevent falls. A short survey was sent out to CAA members in June of 2017 which included questions about the setting in which the audiologist works, whether they inquire about falls on the case history, how much training they received in fall prevention in university, etc.
Survey Results
A total of 53 responses were received. Figure one shows the majority of respondents were from Ontario (54%) and British Columbia (28%). For educational attainment, respondents had a Master’s Degree (73.6%), an AuD (28.3%), or a PhD (3.8%). The length of time working as an audiologist varied across respondents with 30.2% being new graduates (0–5 years), 20.8% working 6–10 years, 5.7% working 11–15 years, 13.2% working 16–20 years, and 30.2% working greater than 20 years. The type of practice was evenly split with 48.1% working in public practice, 42.3 % in private practice, and 9.6% in both. Adult (88.5%) and pediatric (75%) patients were both served with a greater focus on outpatients (61.5%) than inpatients (34.6%). To complete the survey, respondents had to spend at least some of their time working clinically with the majority working clinically 75-100% of the time (79.3%).
It is important when interpreting the survey results to consider there was a high percentage of respondents who either performed vestibular assessments themselves (37.7%) or had someone else on site perform them (7.55%). There is an assumption that audiologists who work at a clinic where vestibular assessments are conducted may have more training or awareness of fall prevention.
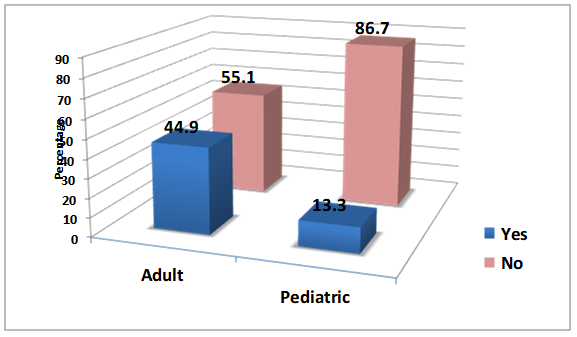
One of the best indicators of fall risk is a previous history of falls. Results from the survey show most clinics do not have a fall history question on their case history form. This was especially true in a pediatric setting. Asking about a history of falls and putting it on the report is important because it can red flag falls as a problem to referral sources and can help monitor changes in rates of falls over time. It can also be a good indicator in assessing if a patient could benefit from physiotherapy or occupational therapy services. Fall prevention is within the scope of audiology. Ignoring the problem or waiting until a patient is in a mobility crisis is not best practice. Simply including a fall history question in your case history is one simple solution you can do to improve your services.
Figure 1. Where do you currently work?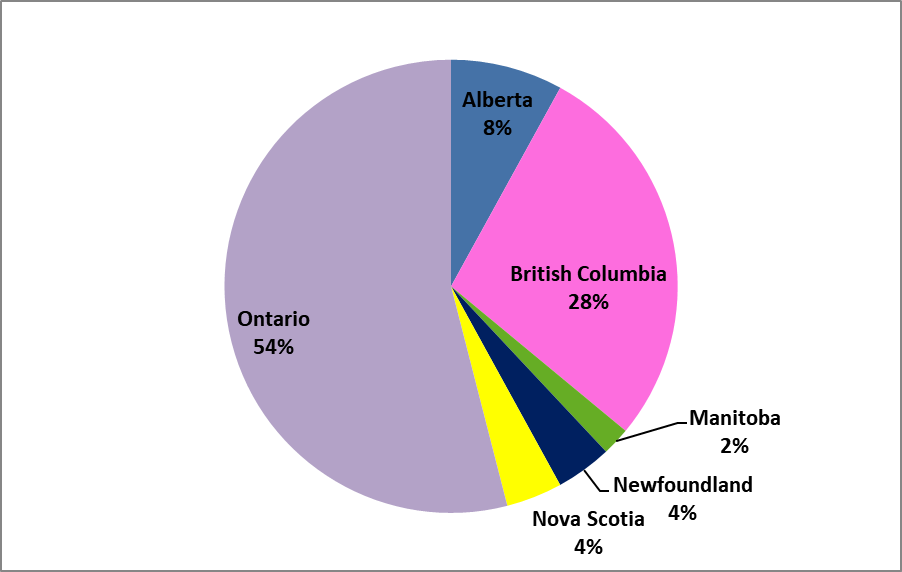
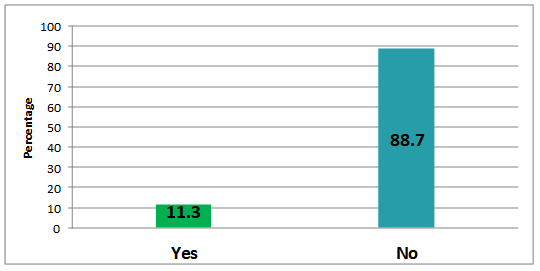
The majority of responses indicated that most clinics do not have fall prevention information in their waiting room such as brochures or posters. The advantages of having information available for patients in the waiting room is that it emphasizes its importance, encourages people to bring up their history of falls, and is an easy way to educate people about fall prevention without taking up any more clinic time. There are many websites, handouts, and free power point presentations available to help educate people about falls. November is fall prevention month – a good time to focus on this important topic. Please see the appendix for a list of resources.
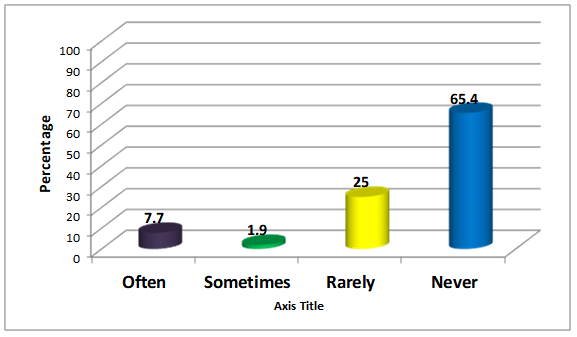
The vast majority of respondents stated they rarely or never give out handouts on fall prevention as part of their counselling sessions (90.4%). The patients that audiologists see are likely to be at high risk of falls and audiologists may be the only health professional that patient visits. The majority of falls occur in the home (6 out of 10). Giving out a home check list can be an easy and quick way to educate people who have concerns about having a fall, have a history of falls, or fail a screening test. This information can be invaluable in that it might help to prevent a fall that results in death or an early nursing home admission (please see appendix for an example).
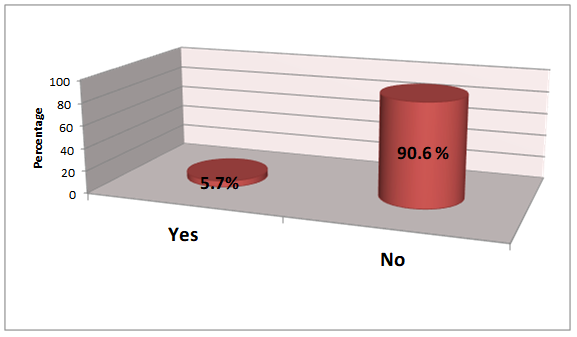
Survey results measured an overwhelming consensus (90.6%) that respondents did not feel their university training program provided enough training on falls and fall prevention which would be taught most likely within a vestibular course. This is in agreement with previous survey results from Verge and Armstrong16 assessing the current state of vestibular assessment and management in Canada. In their 2014 study, a total of 67 Canadian audiologists who count vestibular work as part of their current practice were surveyed and results showed an overwhelming majority of respondents felt that their university training was not adequate (78.6%) for vestibular assessment and management. A total of 44% of respondents received 5 or less hours of vestibular course work as a part of their formal education and those who were unsatisfied with their university training cited lack of total hours devoted to vestibular course work and lack of hands-on training. These fall prevention survey results demonstrate more training in fall prevention may be necessary in our university programs and that a potential barrier to this are reports that vestibular training as a whole may require more enhanced training.16
Responses on referral patterns suggest that the majority of audiologists rarely or never suggest a referral to occupational therapy or physiotherapy when someone has a history of falls.
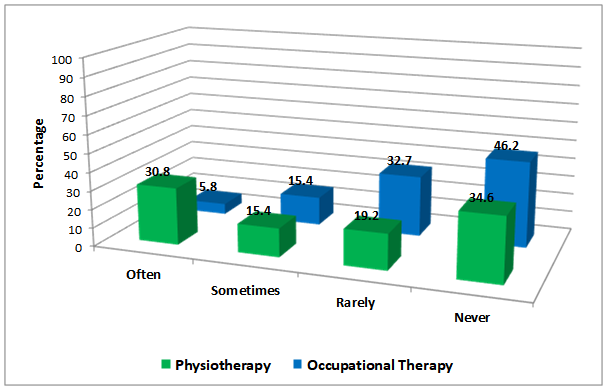
Of those that do (often or sometimes), physiotherapy (46.2%) is more commonly suggested compared to occupational therapy (21.2%). Falls are an interdisciplinary issue and understanding the roles of other professionals on your team, and when to refer, is essential. These survey results help to demonstrate a major barrier to suggesting referrals may be not asking about falls in the case history; this is an essential first step. Audiologists are encouraged to reach out to their local physiotherapists and occupational therapists and ask about referral pathways for private and public services so you are aware of how and when to suggest a referral. The extra benefit of creating this dialogue will be reciprocal referrals which will enhance services for your patients. Some clinics or hospitals offer an interdisciplinary Falls Clinic specially targeting those at risk of falls. Make sure you understand how and when to refer to these speciality clinics.
It is no wonder that the majority of respondents reported they do not use fall risk screening tools when the majority do not have a fall history question on their case history form. It is important to understand that screening tools do not have to take a lot of time in a clinical day; only a few extra minutes are required. These tools can provide a lot of information to help with management decisions like determining if a referral to other health professionals would be helpful (e.g., physiotherapy, occupational therapy, Falls Clinic) or to help gather functional information about outcome measures with rehabilitation. A barrier to using screening tools may again go back to reports of inadequate training. University programs need to be teaching the value of these tools and demonstrating how to perform them. We need to improve our services and become stronger members on interprofessional healthcare teams.
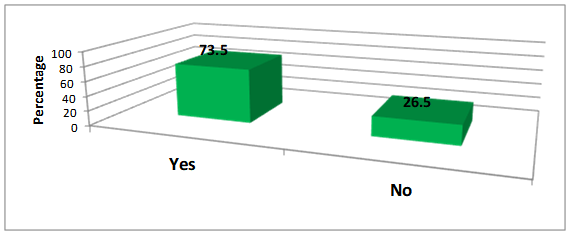
It was alarming over a quarter of respondents (26.5%) reported they felt fall prevention should not be within the scope of practice of audiologists. This is troubling for several reasons:
- Falls are a public health crisis with high financial, physical, and mental health costs.
- Falls being a cause of death for the patients you see, young and old, should be reason enough to get involved.
- Vestibular dysfunction (an area also within our scope of practice) includes hearing loss, tinnitus, unsteadiness, vertigo, and is linked to an increased risk of falls.17
- Moderate hearing impairment in older adults is associated with lower levels of physical activity (a risk factor for falls).18
- Mobility, agility, and pain conditions often occur with hearing limitations.19
- A multidisciplinary team approach to the management of dizzy and unsteady patients improves patient coping, functionality, satisfaction, and decreases overall health care utilization in vestibular patients.20
- According to the CAA Scope of Practice document, all members and associates shall:
- “Take every precaution to avoid harm to patients or clients. This includes following applicable occupational health and safety and infection prevention and control practices, and ensuring that equipment is appropriately calibrated and in proper working order.” Whether or not you believe it should be within your scope of practice only 50% of respondents reported they have a falls prevention strategy policy to reduce or prevent falls/injuries in the workplace. NB: Every workplace/clinic must ensure for the safety of those they serve (who are typically at a higher risk for falls) an environment that reduces the chance of falling in that space.As an example, the Falls Prevention Strategy Required Organizational Practice (ROP) requires clinics to implement and evaluate a falls prevention strategy. All populations at risk must be identified, the specific needs of the populations at risk must be addressed, and measures must be taken to evaluate and provide ongoing improvements to the falls prevention strategy on an ongoing basis. A safety risk assessment should be made for each patient at the beginning of service and should include21:
- A review of internal and external physical environments
- Medical conditions requiring special precautions
- Information sharing with team partners who may be involved in planning of care
- Regular updates and improvements to the safety risk assessment
- Education of patients and families on home safety issues identified in the risk assessment
- “Maintain and enhance their professional competence throughout their careers.” Whether or not your audiology university training program provided enough education on fall prevention or fall prevention was not in your scope of practice when you began, it is up to each audiologist to maintain their professional competence throughout their careers.
- “Take every precaution to avoid harm to patients or clients. This includes following applicable occupational health and safety and infection prevention and control practices, and ensuring that equipment is appropriately calibrated and in proper working order.” Whether or not you believe it should be within your scope of practice only 50% of respondents reported they have a falls prevention strategy policy to reduce or prevent falls/injuries in the workplace. NB: Every workplace/clinic must ensure for the safety of those they serve (who are typically at a higher risk for falls) an environment that reduces the chance of falling in that space.As an example, the Falls Prevention Strategy Required Organizational Practice (ROP) requires clinics to implement and evaluate a falls prevention strategy. All populations at risk must be identified, the specific needs of the populations at risk must be addressed, and measures must be taken to evaluate and provide ongoing improvements to the falls prevention strategy on an ongoing basis. A safety risk assessment should be made for each patient at the beginning of service and should include21:
Conclusion
It is our hope that the results of this survey help to highlight the need for improved fall prevention services in Canada. November is Fall Prevention Month; a good time to start thinking about your role in improving the quality of life and longevity of your patients.
The issue of preventing falls is larger than the field of audiology, and indeed larger than any one profession. The causes and consequences of falls are not just physical, but mental and emotional as well. Being such a multifaceted issue, it requires a team approach to make a difference for many patients.
As the population of Canada continues to age, falls will become an even larger public health concern. These survey results show the profession of audiology needs to better understand its role in fall prevention, our role as an inter-professional team member, and ways to better screen, educate, document, and refer those at risk of falls.
November is Fall Prevention Month
Appendix One: On-line Resources
Fall Prevention Handouts, Checklists, and Posters:
https://vestibular.org/educational-resources/infographics-presentations
http://nscommunitylinks.ca/resources/
https://go4life.nia.nih.gov/sites/default/files/FallProofingYourHome.pdf
http://www.nscommunitylinks.ca/wp-content/uploads/2015/02/Resource-8-Home-Assessment- Checklist.pdf
Fall Prevention Presentations:
https://www.youtube.com/watch?list=PLhMDDgobcByGW3sSoKnQaKZG-oQgnkUvI&v=Cb-q7gcDBHs
https://www.youtube.com/watch?v=EpAD6ochdTE
https://www.aota.org/Practice/Productive-Aging/Falls/Toolkit.aspx
Fall Prevention Tool Kits:
http://www.patientsafetyinstitute.ca/en/toolsResources/Documents/Interventions/Reducing%20Falls%20and%20Injury%20from%20Falls/Falls%20Getting%20Started%20Kit.pdf
http://www.patientsafetyinstitute.ca/en/toolsresources/Pages/default.aspx
http://rgps.on.ca/files/IntegratedProvincialFallsPreventionFrameworkToolkit_July2011.pdf
Fall Prevention Screening Tools:
http://sydney.edu.au/health-sciences/staff/docs/lindy_clemson/FaB_manual_2003.pdf
http://www.rehabmeasures.org/Lists/RehabMeasures/PrintView.aspx?ID=898
http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=903
http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=898
References
- Danhauer JL, Johnson CE, Newman CW, et al. An open letter to Dennis: We can do more to educate our patients about falls risk. Audiol Today 2011;23(5):58–69.
- Public Health Agency of Canada. Seniors’ falls in Canada: Second report. Ottawa: Author 2014. Available at: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/seniors-aines/publications/public/injury-blessure/seniors_falls-chutes_aines/assets/pdf/seniors_falls-chutes_aines-eng.pdf
- American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148–57.
- American Speech-Language-Hearing Association. Audiology information series: Preventing Falls; 2015. Available at: http://www.asha.org/uploadedFiles/AIS-Preventing-Falls.pdf
- Criter RE and Honaker JA. Audiology patient fall statistics and risk factors compared to non-audiology patients. Int J Audiol 2016; 55(10):564–70.
- Clemson L, Cumming RG, and Heard R. The falls behavioural (FaB) scale for the older person: Instruction manual; 2003. Available at: http://sydney.edu.au/health-sciences/staff/docs/lindy_clemson/FaB_manual_2003.pdf
- Shorr RI. Review: Psychotropic drugs increase the risk for falls in older persons … commentary on Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J AM GERIATR SOC 1999 Jan;47:30–9. ACP J Club 1999;131(1):24–24.
- Canadian Patient Safety Institute. Resource guide on falls prevention – for home care service providers; 2014. Available at: http://www.patientsafetyinstitute.ca/en/toolsResources/HomeCareSafety/Documents/Resources%20for%20home%20care%20providers%20-%20Resource%20guide%20on%20falls%20prevention.pdf#search=resource%20guide%20on%20falls%20prevention.
- Criter R. Falls in audiology patients [PowerPoint slides]. As presented at the World Congress of Audiology XXXIII on September 20, 2016 in Vancouver, BC.
- Ko CW, Hoffman HJ, and Sklare DA. Proceedings from 29th mid-winter meeting of the Association for Research in Otolaryngology (ARO): Chronic Imbalance or Dizziness and Falling: Results from the 1994 Disability Supplement to the National Health Interview Survey and the Second Supplement on Aging Study. Baltimore, MD; 2006.
- Jiam NT, Li C, and Agrawal Y. Hearing loss and falls: A systematic review and meta-analysis. Laryngoscope 2016;126(11):2587–96.
- Lin FR and Ferrucci L. Hearing loss and falls among older adults in the United States. Archives of Internal Medicine 2012;172(4):369–70.
- Podsiadlo D and Richardson S. The timed “up & go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39(2):142–48.
- Shumway-Cook A and Woollacott M. Motor control: Theory and practical applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
- Lindsey H. Audiologists integral piece of the puzzle in fall prevention. Hear J 2015;68(10):16–22.
- Verge JA and Armstrong M. Message from the guest editors. Canadian Audiologist 2014;1(4). Available at: http://www.canadianaudiologist.ca/message-from-the-guest-editors/
- Mira E. Improving the quality of life in patients with vestibular disorders: the role of medical treatments and physical rehabilitation. Int J Clin Pract. 2008;62(1):109–14. Epub 2007 May 30.
- Gispen FE, Chen DS, Genther DJ, and Lin FR. Association between hearing impairment and lower levels of physical activity in older adults. J Am Geriatr Soc 2014;62(8):1427–33.
- Statistics Canada. The 2006 participation and activity limitation survey: Disability in Canada (89-628-X). Ottawa: Author; 2010. Available at: http://www5.statcan.gc.ca/olc-cel/olc.action?objId=89-628-X&objType=2&lang=en&limit=1
- Naber CM, Water-Schmeder O, Bohrer PS, et al. Interdisciplinary treatment for vestibular dysfunction: The effectiveness of mindfulness, cognitive-behavioral techniques, and vestibular rehabilitation. Otolaryngol Head Neck Surg 2011;145(1), 117–24.
- Accreditation Canada, the Canadian Institute for Health Information, and the Canadian Patient Safety Institute. Preventing falls: From evidence to improvement in Canadian health care; 2014. Available at:https://accreditation.ca/sites/default/files/falls-joint-report-2014-en.pdf

