Other People’s Ideas
Calvin Staples, MSc, will be selecting some of the more interesting blogs from HearingHealthMatters.org which now has almost a half a million hits each month. This blog is the most well read and best respected in the hearing health care industry and Calvin will make a regular selection of some of the best entries for his column, Other People’s Ideas.
Tinnitus: is a common encounter that continues to require more research and education to facilitate audiologists role in supporting sufferers. The complexity of the tinnitus condition, coupled with no formally agreed upon treatment options challenges the clinician. The following articles from Hearing Health & Technology Matters provides some updates on possible treatment opportunities for tinnitus sufferers.
Signia Primax Hearing Aids Now Offering Notch Therapy Feature for Tinnitus
Originally posted on February 21, 2017
Earlier this month, Signia (formerly Siemens) announced their latest hearing aid innovation: Notch Therapy. According to the company, they are the first in the hearing aid industry to use the novel approach to combat tonal tinnitus, the most common form of tinnitus.
Tonal tinnitus, defined by the American Tinnitus Association, is the “perception of near-continuous sound (or overlapping sounds) with well-defined frequencies”. In many cases, individuals experiencing tonal tinnitus can perceive fluctuating changes in volume over time.
Hearing Aids and Tinnitus Management
Patients undergoing tinnitus treatment are often prescribed hearing aids and also undergo some type of noise or sound therapy to help reduce the intensity of their symptoms. However, unlike traditional sound therapy acoustic stimuli or noise, Notch Therapy is inaudible. This new, proprietary feature enables hearing care professionals to program hearing aids with a filtered “notch” centered at the pitch of the tinnitus.
According to a recent study (Strausse, et al, 2015), published in Clinical Otolaryngology, subjects with Notch Therapy activated in their hearing aids, compared with those that used hearing aids alone, showed a significant improvement within three weeks and maintained the benefit past six months.
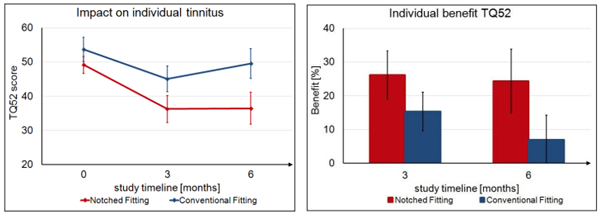
Left: Average reduction of Tinnitus Questionnaire 52 (TQ52) scores for individuals with Conventional Fitting and Notch Fitting. A reduction of the TQ52 score corresponds to an improvement in tinnitus perception and relief. Right: Percent of benefit based on TQ52 scores at 3 and 6 months.
How Does Tinnitus Notch Therapy Work?
During the course of the hearing aid fitting, the hearing professional identifies the pitch of the tinnitus sound, then activates a “notch” that matches pitch within the hearing aids.
For example, if the patient’s tinnitus is centered around 1,000 Hz, the hearing aids can be set to provide amplification for the patient according to their hearing loss across the frequency range, with the exception of at 1,000 Hz. This therapy technique utilizes cortical lateral inhibition, a neural mechanism that reduces the activity in the over-stimulated region of the brain responsible for many types of tinnitus, and has been shown in multiple clinical studies to be highly effective.
According to the company, this “this strategically placed spectral notch works to suppress tinnitus at its neurological source without restricting good hearing and speech comprehension” and thereby allows the brain to learn to disregard the tinnitus sound over time.
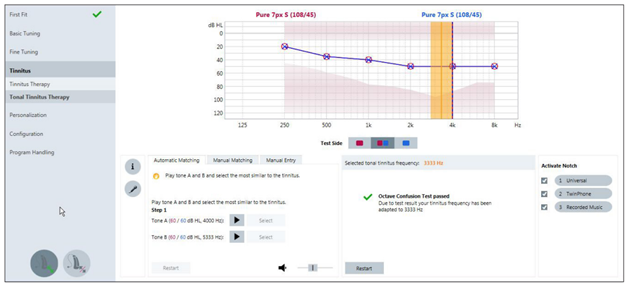
Tonal Tinnitus Therapy screen in Signia Connexx fitting software, showing a Manually Entered pitch match as 3333 Hz, with the Frequency Check completed and the notch activated in all three listening programs.
Tinnitus Management: Options
The new Notch Therapy approach to tinnitus is available in Signia primax hearing aids, which is offered in addition to the more traditional sound therapy options that are also available for activation within the fitting software.
According to the company, the hearing aids can be used to provide relief to tinnitus patients, with or without hearing loss.
All About Tinnitus for Consumers and Patients
Article originally posted December 28, 2016
Today’s topic is a vexious problem that gets far less attention by hearing health professionals than you would think. Tinnitus is a big issue for patients, but not one that is treatable by pills, surgery, or other traditional treatments. However, there are treatments that are effective for some people.
What It Is
Tinnitus (pronounced “tin EYE tus”) is a frequent, unpleasant companion to hearing loss. Moreover, it is an invisible, unpleasant companion because it is heard in almost every case only by the person who has it, not by others. Many people describe their tinnitus as sounding like bells or crickets.
For some, tinnitus is occasional, low level and largely ignored. For others, it is worrisome or frightening – they wonder if they have mental problems or if they have a brain tumor. Fortunately, tinnitus is not a sign of mental problems and only a tiny fraction of a percent of people with tinnitus and/or hearing loss have so-called “eighth nerve tumors.”
There is one small but important group of people who are tinnitus sufferers – their tinnitus is constant, extremely distracting, loud- to-blaring. For those people, tinnitus is a disabling condition.
The Clinical Picture
“Tinnitus is one of the most common clinical syndromes in the US, affecting 12% of men and almost 14% of women who are 65 and older. It only rarely afflicts the young, with one significant exception: those serving in the armed forces. Tinnitus affects nearly ½ the soldiers exposed to blasts in Iraq and Afghanistan” (Gropman, 2009).
Important neurophysiologic research is being conducted on tinnitus. Researchers are using rats to test theories of tinnitus and find drugs that suppress tinnitus. They have yet to identify a successful suppression treatment, but they have definitively proven that tinnitus is caused by biological changes in the brain, not by psychological processes. In other words, it’s not just something people imagine – although it certainly affects those who have it psychologically.
The idea that brain changes underlie tinnitus is a game-changer for audiologists and their patients. We used to think that tinnitus resulted from damage to the inner ear. That’s still the case, especially for tinnitus caused by high aspirin dosage. But now we know that it’s not that simple. There is a “central” origin (or probably multiple centers) in the brain which regulates a person’s perception of tinnitus. This is in line with new thinking on hearing loss and hearing aids: the initial insult that causes hearing loss occurs in the inner ear, but the changes in auditory perception that occur because of that insult are in the auditory centers of the brain. That is why hearing aids are now considered to be a first line of defense against losing auditory perceptual capability, and possibly auditory cognitive deficits as well.
Help for Tinnitus Sufferers
What is available to help people who suffer from tinnitus? There are no FDA approved drug therapies for tinnitus treatment, but antidepressants and anti-anxiety medications are prescribed for some people to ease their suffering, much as they are for people who suffer from chronic pain. Those drugs do not suppress tinnitus, they just make it more bearable.
On the other end of the treatment spectrum, Tinnitus Retraining Therapy relies on sound therapy and patient-centered psychological counseling to remove negative connotations of tinnitus. TRT takes 12 to 18 months, which makes patient compliance a serious concern. In general, success rates with drugs or counseling based treatments are hard to pin down but none are stellar.
The most successful treatment for tinnitus is some form of amplification, either with hearing aids alone or those fitted with tinnitus “masker” circuitry which pumps tailored noise into the wearer’s ear to cover or compete with the sound of the tinnitus. In one report, hearing aids “often have a beneficial effect on the underlying tinnitus. Relief from tinnitus may persist for hours after the hearing aid has been removed” (Castillo & Roland, 2007). In another study, about two thirds of 1440 patients fitted with hearing aids on one or both ears reported improvement in their tinnitus (Trotter & Donaldson, 2009). In a survey of hearing health care providers, 88% reported that they recommended hearing aids as the treatment of choice for tinnitus (in the presence of hearing loss). Those providers reported a success rate of 60%: 22% of their patients experienced major benefit and 38% found their tinnitus reduced to some extent.
What Tinnitus is Not and What to Do About It
Tinnitus is a symptom and not a disease. That makes it confusing to patients and primary care physicians when it comes to deciding how to handle it, especially in cases of mild hearing difficulty.
The first step in EVERY case is a comprehensive diagnostic audiology evaluation to rule out or identify presence of an auditory nerve tumor, middle ear disorders, and even impacted wax. Audiometric testing takes about an hour, can be covered under Medicare, and points patient and physician to the appropriate management strategy.
Additionally, audiologists can administer the Tinnitus Handicap Inventory, a self-report measure, to assess the impact of tinnitus on a patient’s daily life. If audiometric test results show deficits in speech audibility and intelligibility, hearing aids may be in order to correct speech processing deficits as well as potentially mitigate tinnitus effects reported by patients.
References
Castillo MP & Roland PS. Disorders of the auditory system. In Roeser R, Valente M & Hosford-Dunn H (eds), Audiology: Diagnosis (2007, 2nd Ed). New York: Thieme.
Groopman J (2009). That buzzing sound: The mystery of tinnitus. The New Yorker, Feb 9 & 16, 42-49.
Henry JA et al (2009). Tinnitus Retraining Therapy: Clinical Guidelines. San Diego: Plural Publishing.
Kaltenbach JA (2009). Insights on the origins of tinnitus: An overview of recent research. Hearing Journal 62(2), 26-31.
Kochkin S & Tyler R (2008). Tinnitus treatment and the effectiveness of hearing aids: Hearing care professional perceptions. Hearing Review, Dec, 14-17.
Korres S, et al. Tinnitus Retraining Therapy (TRT): outcomes after one-year treatment. Int’l Tinnitus Journal, 2010; 16(1): 55-9.
Newman CJ et al. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143-148.
Sereda M et al. Consensus on Hearing Aid Candidature and Fitting for Mild Hearing Loss, With and Without Tinnitus: Delphi Review. Ear Hear. 2015 Jul; 36(4): 417–429.
Trotter M & Donaldson I (2008). Hearing aids and tinnitus therapy: a 25-year experience. J Laryngol & Otol 122(10):1052-6.
New User-Friendly Tinnitus Programs Have Potential To Meet Demand
Originally posted on December 26, 2016
Tinnitus is a condition affecting upwards of 15% of the population and many bothered by the condition may be under served. That according a recent JAMA Otolaryngology article, which concluded there is a significant opportunity for hearing care professionals to get more actively involved in the long-term care and management of patients experiencing bothersome tinnitus.
Other organizations appear to be heeding this call to action. At the recently concluded annual International Hearing Society meeting in Chicago, members were encouraged to enroll in their upcoming Tinnitus Care Provider Workshop. Under the direction of leading tinnitus researcher, University of Iowa professor of audiology, Richard Tyler, the two-day workshop will focus on counseling strategies that can be used as part of a tinnitus management practice.
Ida Institute Launches Tinnitus Management Tools
In addition to the new IHS certification program, the Ida Institute of Denmark, has developed three new tinnitus management tools. Two tools, the Tinnitus Thermometer and the Tinnitus Communication Guide, are designed to help clinicians build their counseling skills and apply a holistic approach to care of patients with tinnitus. The third tool, referred to as the Tinnitus First Aid Kit is an information hub, developed in partnership with the British Tinnitus Association. This tool is designed to empower patients to access the resources they need to understand, manage, and cope with tinnitus.
The Ida Institute tinnitus management tools can be assessed here.
“Managing tinnitus is often difficult for both patients and hearing care professionals. There are a number of reasons for uncertainty in tinnitus management. These include the fact that the tinnitus has different causes and patient experiences vary, so a treatment that works for one patient may not work for another. Additionally, many clinicians do not specialize in tinnitus and may feel that they don’t have adequate counseling skills to support the patient. Part of tinnitus management also involves thinking about how messages are related to the patient. Because there is no cure for tinnitus, patients might focus on the negative and develop a feeling of hopelessness that impacts their ability to consider treatment options. It is the responsibility of the professional to help the patient leave the appointment with a more positive mindset – “I can do something to make this better,” or, “I will feel better in the future,” rather than, “There is no cure.” Together with collaborators from our seminar, we have developed three resources to help hearing care professionals find an effective way to give patients the hope and support they need to manage tinnitus.”
–Lise Lotte Bundesen, Managing Director, Ida Institute
Effective Treatment Options
In addition to the new program offerings from IHS and the Ida Institute, a published ahead of print article at Ear and Hearing seems to indicate that more generic forms of counseling, when combined with ear level hearing aids or so-called combination devices offer effective treatment approaches for patients with bothersome tinnitus.
In a randomized controlled trial involving two well-established methods: Tinnitus Masking (the late Jack Vernon’s program) and Tinnitus Retraining Therapy (Pawel Jastreboff’s program), these two established methods were compared to a more general form of educational counseling paired with ear level devices.
Following 12 months of intervention, the three approaches – Tinnitus Masking, Tinnitus Retraining Therapy and the more generic approach – all garnered significant improvements in tinnitus handicap.
In another randomized controlled trial from Linkoping University in Sweden – this study involving individuals with hearing loss and tinnitus, one group of participants was enrolled in the “standard practice procedures” group(patients fitted with hearing aids and counseled in a conventional manner). This group was compared to a group fitted in a similar manner, but exposed to Motivational Interviewing (MI). Both groups were provided four follow-up appointments. Although both groups derived significant benefit from their hearing aids at the end of three months, the MI group had greater reductions in tinnitus handicap.
Both studies suggest a combination of relatively general educational counseling and an ear level device provide sufficient tinnitus relief for many patients. Thus, clinicians can readily master the skills needed to provide a valuable cost-effective service for individuals bothered by tinnitus.
By offering these options, the Ida Institute and IHS are making a valuable service more accessible to professionals and their patients.
Tinnitus Primer for Consumers: And All This Time You Thought It Was In Your Ears!
Originally posted on February 14, 2017
In recent years, research from animal models and now human modeling has suggested a brain locus for tinnitus, rather than the ear-level origin assumed previously.
Research into tinnitus has become much more sophisticated of late, and is changing the common understanding of the disorder and providing the first testable model of human tinnitus that could provide some new avenues for therapy. (AAAS Eureka Alert)
Tinnitus, a Common but Confusing Condition
Tinnitus is an odd affliction of the auditory system, not unlike the “phantom pain” that afflicts many who have lost a limb. People with tinnitus perceive sounds that they variously describe as ringing, buzzing, humming, cicada-like, etc. But, their perception doesn’t match reality: the sounds they hear are phantom sounds heard only by them. The phantom sounds, like phantom pain, are a side effect of bodily damage. In the case of tinnitus, the ringing/buzzing is an early warning sign that the person has sustained damage to hair cells in the inner ear. Damaged inner ear hair cells eventually cause hearing loss.
Tinnitus is the most common disorder of the auditory system, affecting upward of 40 million people in the US. The diagnosis of tinnitus is based solely on the patient report, since the physician or audiologist cannot hear the tinnitus, measure it directly, or visualize inner ear hair cells. Until recently, research into tinnitus has been limited by these factors. The surge in tinnitus research is driven, in part, by new imaging techniques. But the high incidence of tinnitus complaints in returning veterans with hearing loss caused by exposure to loud explosions is also spurring researchers in other fields such as neurophysiology to look at tinnitus.
The Georgetown University LINC
Brain imaging studies in humans with tinnitus have been underway for some years at the Laboratory of Integrative Neuroscience and Cognition (LINC) at Georgetown University Medical Center (GUMC). The reason brain imaging is so important to tinnitus is because those studies are pointing to hyperactivity in the brain’s central auditory system as the primary source of tinnitus.
The researchers suggest that tinnitus works like this: it starts when hair cells are damaged, which sends a message to the brain’s central auditory pathways that there is a problem; the brain centers reorganize to respond to the damage. Here’s a paraphrase/quote from the researchers:
Receptors in the auditory parts of the brain aren’t receiving perceive sensory input from the damaged hair cells anymore, so they compensate by firing spontaneously and frequently, which produces the initial tinnitus signals. The brain fills in sensations in response to a deficit of input. Neighboring frequencies become amplified and expand into the vacated frequency range. It also happens to people with a hole in their retina. They don’t see the hole because the brain fills in what is missing.
Old Brain Structures and Network Dysfunctions
This is really interesting stuff, but here’s where it gets REALLY interesting. In normal auditory brain regions, the researchers have discovered a feedback system that cancels out the unreal sounds of tinnitus by a process known as “inhibition.” The feedback system is regulated down in the “old brain” in an area called the limbic system, which precedes awareness/consciousness.
The limbic system is central to emotional regulation and there is some suggestion that people who suffer from tinnitus are also more likely to suffer from chronic pain, depression, insomnia, and jaw clenching (Roberts et al., 2010). Georgetown LINC studies by Leaver et al (2011 & 2016) found that tinnitus-related neural hyperactivity was greatest in limbic structures, especially in the nucleus accumbent, which is involved in cognitive processing and implicated in addictive behaviors. Morever, the hyperactivity was specific to sounds which were matched in frequency to the patients’ own tinnitus.
We definitely know that tinnitus affects people’s quality of life (QOL). As one of the Georgetown LINC researchers comments: people with tinnitus may “have an independent, systemic vulnerability in one or more neurotransmitter systems in the limbic region. That could explain why drugs that modulate neurotransmitters like serotonin appear to help some people out... It appears tinnitus is the auditory symptom of an underlying syndrome, which becomes evident in patients who happen to have a hearing loss.” (J.P. Rauschecker,PhD)
Developing Tinnitus Treatments
Future research is aimed at identifying neurotransmitters that are involved in the brain’s noise cancellation system. If those can be identified, the thought is that they might be used as a therapeutic drug therapy to treat tinnitus in such a way that patients’ noise cancellation systems are restored. Quoting Dr. Rauschecker once more:
“If we can find a way to turn that feedback system back on to eliminate phantom sound, it might be possible one day to take a pill and make tinnitus go away.”
References
Imaging reveals how brain fails to tune out phantom sounds of tinnitus. Press Release from Georgetown University Medical Center.
Leaver, A. et al. (Jan 13, 2011). Dysregulation of limbic and auditory networks in tinnitus. Neuron, 69(1), pp 33-43.
Roberts, LE et al. (Nov 10 2010). Ringing Ears: The Neuroscience of Tinnitus. J Neuroscience, 30(45), pp 14972-14979.

