The Importance of Telecommunication Accessibility for People Living with Hearing Loss
Janine Verge, AuD, Aud (C) is coordinating the “Issues in Accessibility,” column which will cover topics addressing issues in accessibility for people who are Deaf/deaf and hard of hearing.
Introduction
The COVID-19 pandemic has highlighted how important accessible telecommunications are to our social connectedness, now and in the future. These devices and tools continue to evolve at exponential rates, giving rise to a multitude of telecommunication devices and features to choose from. Audiologists play an essential role in helping people communicate effectively, which includes the use of telecommunications since these can be a barrier for people living with hearing loss. Solutions are unique for each person and they should be selected based on a variety of factors including the degree of hearing loss, type of amplification used, telecommunication devices used, and the listening needs required for each device. Differences between age groups continue to exist in telecommunication usage and must be considered when helping seniors overcome communication barriers. We propose that the field of audiology should re-evaluate its role in providing support for telecommunication technologies. This article will explore why some barriers to telecommunication exist, the significance of these barriers, and finally propose ideas on how to provide more support.
Telecommunication Barriers
The Digital Age Divide

An age divide exists in how older adults access different communication technologies and the types of services they use. A study by Pang et. al., reported that usage barriers of smartphones for older adults may include subjective, technological, and situational barriers.1
Subjective barriers are related to an individuals' attitudes and ability such as a lack of know-how on how to use a smartphone which might be related to a decline in both mental and physical ability. Hearing loss can be a subjective barrier in creating increased effort or an inability in knowing the phone is ringing, locating a ringing phone, knowing when speech is detected, and/or understanding speech. Technological barriers are related to interface and usability concerns. Situational barriers include economic costs.1–3
In Canada, our aging population is continuously growing. It is predicted that by 2030, seniors will make up 23 percent of Canadians. Hearing loss can affect adults of all ages, although it is much more likely to occur in older adults (78%) compared to younger adults (15-40%).4 Since hearing loss is common and a possible subjective barrier to communication technologies, especially in older adults, Audiologists serve an important role in supporting their successful use and satisfaction levels.
Telecommunication Use
Satisfaction and Adoption Rates
Hearing aid adoption influences the satisfaction of using traditional phones or cellphones for people living with hearing loss. According to MarkeTrak IX, the level of satisfaction using a traditional telephone or cellphone is improved when using hearing aids. However, those most satisfied were hearing aid owners for less than 5 years. It is important to note that these individuals were still not fully satisfied talking on a cellphone and/or landline (70%; 69%). These results emphasize the increasing significance of the audiologist's role in providing individuals with the necessary tools to successfully use telecommunications (Figure 1).5
Table 1. Marketrack IV: Satisfaction as a Function of Specific Listening Situations
| Listening Situation | Owners HA<= 5 years (n=769) | Owners HA 6 + years (n = 112) | Non-owners Returners who tried HA (n = 44) | Non-owners Never Owned (n = 2055) |
| When talking on a cellphone | 70% | 59% | 50% | 47% |
| When talking on a traditional phone | 69% | 59% | 52% | 51% |
Those living with hearing loss who do not wear hearing aids have the least amount of satisfaction when talking on a cellphone or traditional landline phone, which represents the majority of people living with hearing loss (hearing aid adoption rate for MTX was 34.1%). The most common reasons given for not getting hearing aids were financial constraint or lack of perceived need. It is important to note that MarkeTrak IX survey only examined phone use. With the increased use of virtual platforms to communicate at work and home, future surveys should include satisfaction levels using computers and virtual platforms as well.
The Communications Monitoring Report by the CRTC (2018) found the type of telecommunications people use change over time.6 In the report, Canadian households continued to abandon landline telephone service (67% down to 7.1%) in favour of mobile service (88%), (Figure 2). Importantly, phone access was different according to age group. Mobile (70%) penetration was significantly lower in the 65 years and over group compared to 18 to 34-year old’s (99%; 97%) (Figure 3).
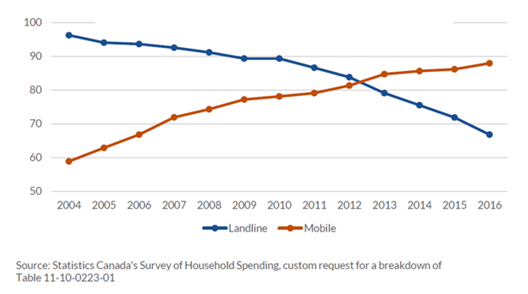
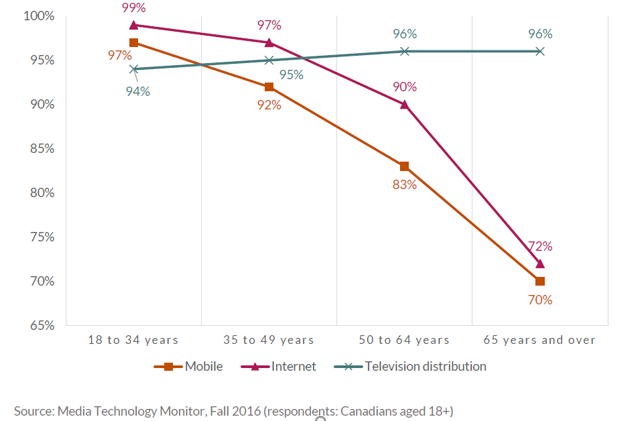
The report also showed there is still a significant number of seniors using landline phones, and economic costs remain a barrier for telephone use. While more than 99% of Canadian households have telephone service, just 3% of Canada’s highest-income households rely solely on a landline, compared to almost 30% of lowest-income households. Since different telecommunication devices are used, based partly on age and economic costs, Audiologists need to understand what the specific barriers are for all available devices.
Outcome Measurement Tools
Appendix A shows a list of common outcome measurement tools and their specific questions relating to telephones and cellphones. There is a need to modernize these measures as none of the outcome measurement tools ask about computers and the majority ask about landlines and not cellphones. Also, questions are typically open-ended and do not direct the clinician to the individual, environmental, or listening task that is causing a barrier. We propose that the development of a standardized outcome measure is essential in addressing telecommunication listening needs and would allow audiologists to better determine what features of various technologies could be used, modified, integrated, or adapted to maximize performance and satisfaction levels (for those with and without hearing aids).
Misperception of one’s own ability to use technology can be a barrier to succeeding with telecommunications. A study by Desjardins and Doherty found there was variability among people’s ability to use their telecoil function on the phone.7 In the study, a total of 50 experienced hearing aid users demonstrated how they use a phone and this task was found to be problematic in more than 75% of participants. Users with and without telecoils had difficulty using their telecoil function and positioning the phone to speak without feedback. Patients’ estimates of their hearing aid skills in usage and maintenance did not correlate with their task performance. The hearing aid skills were also lower for older participants. These findings highlight the need for using outcome measures. Hearing aid users may be struggling with the usability of certain features on the phone and may not communicate this with their audiologist since they think it is the hearing aids themselves causing the issue.
Verification of Hearing Instrument Settings
Verification of hearing instrument settings is another critical factor in optimizing user satisfaction with telecommunication devices. Two main ways to integrate amplification with telecommunications is through streaming and telecoil-based phone programs. Here are two excellent references for more information on how to maximize performance:
Verifying Monaurally and Binaurally Linked Telephone Programs
Importance of Telecommunication Accessibility
Loneliness and Social Isolation
Loneliness and social isolation are two important health outcomes affected by communication challenges. Social interaction is key to mental, emotional, and physical well-being. A study by Petersen et al., demonstrated a close relationship between social isolation and loneliness and also indicated that phone behaviour is associated with emotional state and cognitive function.8 Many scales used to assess social isolation ask participants how often they contact friends and family by phone, in addition to asking how often they are contacted in person. These results highlight the need for audiologists to look for signs of, assess, and monitor social isolation and loneliness (e.g., DG Loneliness Scale) including its relationship to phone usage.
Healthcare and Long-term Care Homes
One of the many tragic outcomes of the COVID-19 pandemic was the social isolation of seniors in long-term care homes. The Federal government recommended residents be offered smartphones, tablets, and free internet connections, if possible, to depend on virtual instead of in-person visiting.9 At times, this was the last and only way family members could connect with their loved ones before they died, shining a light on the importance of accessible telecommunications for seniors and their families.
Virtual Healthcare and Phone Accessibility
Another valuable lesson learned from the COVID-19 pandemic was the increased use of virtual health care and the differing preferences between age groups for participation in telehealth. The Virtual Care Task Force released a timely document in February 2020 entitled, Virtual Care: Recommendations for Scaling up Virtual Medical Services.” Its recommendation was for enabling and expanding the implementation of virtual care in Canada.10 To study its use further, a survey by the Canadian Medical Association was conducted with 1,800 Canadian residents from May 14 to May 17, 2020 regarding how participants felt about COVID-19 and Virtual Health Care.11 When respondents' answers were separated by age (below and above 45 years old), the older respondents reported they were more likely to prefer an in-person visit (64%) as a first way to seek a doctor’s advice compared to the younger group (49%). During the pandemic, older respondents reported they used telehealth less often (4%) compared to the younger group (10%). These results highlight the importance of exploring age differences to further understand what barriers may exist for seniors using telecommunications for virtual healthcare.
The Role of the Audiologist in Telecommunication
Finding the Right Solution: An Individualized Approach
Finding the right telecommunication technology solution(s) for each person living with hearing loss is not a one size fits all approach. Different characteristics of the individual (e.g., degree of hearing loss, speech discrimination ability, auditory processing ability), the environment (e.g., noisy, poor acoustics, reverberation) and the desired listening task (e.g., hearing phone ring from another room, speech clarity, phone ring localization, phone use, video platform use, self-advocacy, communication skills) could impact which solution(s) would be a better fit.
Individual solutions can vary on a number of factors including the current communication technologies people have access to (e.g., landline phones, cell phones, and video platforms). Another important variable is whether or not they wear hearing aids or cochlear implants, and further, how much they can integrate/stream their communication devices with their hearing technologies (e.g., t-coil, Bluetooth). Many other individual subjective variables (e.g., cognitive issues, visual impairment), technological, and situational differences are also relevant.
It is important to note that everyone, including those with and without hearing loss, might require an aural rehabilitation plan for improved use of telecommunications. This could include people who have audiograms within normal limits (e.g. auditory processing disorder), temporary hearing loss (e.g., ear infections), asymmetrical hearing loss (e.g. single-sided deafness), or those who work in noisy conditions that make hearing more challenging (e.g., call center).
The determination of patient-centred solutions based on these considerations will be explored further in part two. Some examples of ways to reduce barriers might include reducing background noise, amplified headsets/ headphones, amplified landline phones, changing tone control settings, visual and vibration alerts, captioning, video relay, TTY/TTD, communication training, integration with hearing aids or cochlear implants through t-coils or Bluetooth streaming, distributing informational brochures, and/or referring patients to non-profit groups providing ‘digital literacy’ (e.g., libraries, cellphone store learning series, non-profit digital literacy organizations) to enhance satisfaction levels depending on the individual needs of each person and their family.
Barriers to Providing Aural Rehabilitation in Clinical Practice
Demonstrating assistive technologies and modeling accessible telecommunications in audiology clinical practice is an important aspect of providing aural rehabilitation. It provides an accessible service and promotes technologies and techniques that can improve access at home and in the workplace. Accessibility, including telecommunications, is a basic human right for Canadians living with hearing loss reinforced by the Federal Accessible Canada Act, provincial accessibility laws, national building code, and the Canadian Charter of Rights and Freedoms. Audiology clinics are typically the first point of contact for individuals seeking out hearing healthcare. We need to educate people about all of their hearing health care options, including telecommunications, to fully address their listening needs as they may not get this important information or service anywhere else.
In an article entitled, “Overcoming Barriers to Aural Rehabilitation” by the American Speech-Language-Hearing Association (ASHA), authors state current barriers exist in the delivery of effective aural rehabilitation in part because of a bundled reimbursement and technocentric model of service delivery which may cause the audiologist to miss the patient's broader outcomes in listening communication, and functional well-being. They suggest professional and consumer advocacy are necessary to change the existing system to ensure that a range of adult aural rehabilitation services are available to meet the communication needs of adults with hearing loss.12
Conclusion
Telecommunication adoption, accessibility features, integration with amplification, and usage are advancing at a very fast pace. Audiologists need to re-examine their role in reducing barriers and improving satisfaction using telecommunication technologies to reduce the individual, organizational, and systemic barriers people living with hearing loss endure at home, work, and in the community.
References
- Pang N, Vu S, Zhang X, and Foo S. Older adults and the appropriation and dis-appropriation of smartphones. Lecture Notes in Computer Science. Cham, Switzerland: Springer International Publishing; 2015: 484–495.
- Pew Research Center. U.S. smartphone use in 2015. [Internet]. 2015. Available at: https://www.pewresearch.org/internet/2015/04/01/us-smartphone-use-in-2015/
- Berenguer A. Are smartphones ubiquitous: An in-depth survey of smartphone adoption by seniors. IEEE Consumer Electronics Magazine 2017;6(1);104–10.
- Statistics Canada. The 2006 Participation and Activity Limitation Survey: Disability in Canada. Statistics Canada Catalogue no. 12-89-628-X. Ottawa. Version updated Feb 2009. Ottawa; 2010. Available at: https://www150.statcan.gc.ca/n1/pub/89-628-x/2009012/fs-fi/fs-fi-eng.htm
- Abrams H and Kihm J. MT9 reveals renewed encouragement as well as obstacles for consumers with hearing loss. Hear Rev 2015. Available at: https://www.hearingreview.com/practice-building/marketing/introduction-marketrak-ix-new-baseline-hearing-aid-market
- Canadian Radio-television and Telecommunications Commission. Communications Monitoring Report. 2018. Available at: https://crtc.gc.ca/eng/publications/reports/policymonitoring/2018/
- Desjardins J and Doherty K. Do experienced hearing aid users know how to use their hearing aids correctly? Am J Audiol 2009;18(1):69–76. doi: 10.1044/1059-0889(2009/08-0022)
- Petersen J, et.al. Phone behaviour and its relationship to loneliness in older adults. Aging Ment Health Oct 2016;20(10);1084–91. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698244/
- Government of Canada. Interim Guidance: Care of Residents In Long Term Care Homes During The COVID-19 Pandemic; 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/residents-long-term-care-homes-covid-19.html#a4.4
- Virtual Care Task Force. Virtual Care: Recommendations for Scaling Up Virtual Medical Services. 2020; Available at: https://www.cma.ca/sites/default/files/pdf/virtual-care/ReportoftheVirtualCareTaskForce.pdf
- Canadian Medical Association. What Canadians think about virtual health care: Nationwide Survey Results; May 2020. Available at: https://www.cma.ca/sites/default/files/pdf/virtual-care/cma-virtual-care-public-poll-june-2020-e.pdf
- Spangler C, et al. Overcoming Barriers to Adult Aural Rehabilitation. ASHA; 2015 Available at: https://www.asha.org/Articles/Overcoming-Barriers-to-Adult-Aural-Rehabilitation/
Appendix A: Audiology Outcome Measures: Telephone Use
| Name of Outcome Measure | Question(s) about Telephones | If Yes, Specific Question Listed |
| Client Oriented Scale of Improvement | Yes | -Familiar speaker on phone -Unfamiliar speaker on phone -Hearing phone ring from another room |
| TELEGRAM | Yes | Cellphone/Landline 1-5 scale (no difficulty to great difficulty) |
| Hearing Handicap Inventory for the Elderly | Yes | Does a hearing problem cause you to use the phone less often than you would like? |
| Hearing Handicap Inventory for the Elderly - S | None | |
| Hearing Handicap Inventory for Adults | Yes | Does a hearing problem cause you to use the phone less often than you would like? |
| Hearing Handicap Inventory for Adults - S | None | |
| Hearing Disability and Handicap Scale | Yes | Do you hear the telephone ringing from another room? |
| Profile of Hearing Aid Performance | Yes | -When the telephone rings, the sound startles me -The ring of a telephone sounds ‘tinny’ |
| The Speech, Spatial and Qualities of Hearing Scale | Yes | Having conversation on telephone, follow one person speaking and telephone at same time |
| The Glasgow Hearing Aid Benefit Profile | Yes | Having a conversation on the telephone |
| The Abbreviated Profile of Hearing Aid Benefit | None | |
| The Communication Scale for Older Adults | Yes | My family is willing to make telephone calls for me |
| Satisfaction with Amplification in Daily Life | Yes | How helpful is your hearing aid device(s) on MOST telephones with no amplifier or loudspeaker |
| The Communication Profile for the Hearing Impaired | Yes | (Which type of situation really matters to you) -You’re talking on the telephone when you’re at work -You’re at home talking on the telephone - (How often the situation occurs) My job requires me to use the telephone |
| International Outcome Inventory – Hearing Aids | None |

