Striking the Right Balance
In this edition of “Striking the Right Balance,” Janine Verge, AuD, Michael Vekasi, AuD, Sue Ehler, Shannon Phillips, Ben Kuai, and Josh Creppin, MSc, write about the use of fall risk screening tools in an Audiology practice, paying tribute to November being Fall Prevention month!
Michael Vekasi, AuD, R.Aud, Aud(C), FAAA and Erica Zaia, MSc, RAUD are coordinating the “Striking the Right Balance,” feature which will cover the latest information on ‘all things vestibular.’
If you would like to be more involved in all things vestibular, please check out and like our Facebook page by searching for “CAA National Vestibular Special Interest Group” within Facebook. You can also reach us by email at CAAvestibular@gmail.com.
Using Fall Risk Screening Tools in Audiology Practice: A Step-by-Step Guide
Fall prevention is within the scope of practice of audiologists based on numerous studies linking the patient population we see, those with hearing and vestibular impairment, with being more at risk of falls. Hearing impairment and audiology clinic visits are related to increased fall risk and documented falls. Compared to individuals with no noted impairments, individuals with hearing impairments are associated with a significantly greater risk of developing chronic health problems (arthritis, depression, high blood pressure, high cholesterol, diabetes, and vision issues) that can contribute to an increased risk of falling. For example, arthritis, high blood pressure, and high cholesterol may contribute to decreased physical activity, leading to muscle weakness, putting the individual at a greater risk of falling. Hearing loss and depression are suggested to lead to social isolation and cognitive decline, which is an additional risk factor for falls. Regarding chronic dizziness or imbalance, older seniors with these symptoms are 2 to 3 times more likely to fall than older people who do not experience these issues.
Multiple studies provide evidence supporting the link between hearing impairment and increased fall risk. A meta-analysis of 13 studies showed a greater number of falls documented in participants with hearing loss relative to participants with normal hearing. Overall, this meta-analysis concluded that falls were 2.39 times more likely to occur in participants with hearing loss than with those with normal hearing. Another study noted that 50% of patients seen in an audiology clinic reported at least one fall within a year prior to the appointment. More specifically, 68% of audiology patients reported a recent fall within the last 12 months compared to 28% of non-audiology patients. These audiology patients were also more likely to report multiple falls within the year (64.7% compared to 42.9%). An additional study demonstrated that for every 10dB increase in PTA thresholds, a history of falls was 1.4 times more likely to be present in individuals aged 40–69 years old. Overall, the evidence suggests that fall risk increases with greater severity of hearing loss, and hearing loss prevalence increases with age. The majority (83%) of the audiological clinical caseload are aged 60 years old or greater.
Falls are a public health crisis, with an estimated one-third of Canadian seniors expected to experience a fall within the following year. Additionally, half of Canada’s long-term care facility residents fall annually, resulting in a serious injury in 1 out of 10 people. The Public Health Agency of Canada defines a fall as “a sudden and unintentional change in position resulting in an individual landing at a lower level such as on an object, floor or the ground, with or without injury.” Seniors aged 65 and older are at the most significant risk of falling. More so, seniors in long-term care facilities or persons with cognitive impairment or dementia are at an even greater risk. Falls are the leading cause of hospitalization for children, young adults, and seniors. Therefore, fall prevention is important for people of all ages, not specifically seniors. Falls are associated with detrimental physical, mental, and financial consequences, which is why audiologists need to get involved in fall prevention.
CAA 2017 Fall Prevention Survey Results and Fall Risk Screening
A CAA survey of audiologists on fall prevention strategies was conducted in 2017 and found that of the 53 respondents, over 75% reported they do not conduct any fall prevention screening tools despite it being within our scope of practice. In addition, researchers Patterson and Honaker surveyed 275 audiologists, of which 62.1% reported no experience with risk of falls assessments despite the majority working with geriatric patients (83%). They suggest that although audiologists support the risk of falls assessment, further education is warranted.
Falls can potentially be preventable if individuals with high fall risk are identified early enough, so it is crucial to identify those at risk to receive appropriate supports and interventions. Fall risk screening tools are quick to administer, do not require extensive training to use, and enable an easy way to gain insight into a patient’s real-world limitations. These short tests are practical for use in all clinical practices.
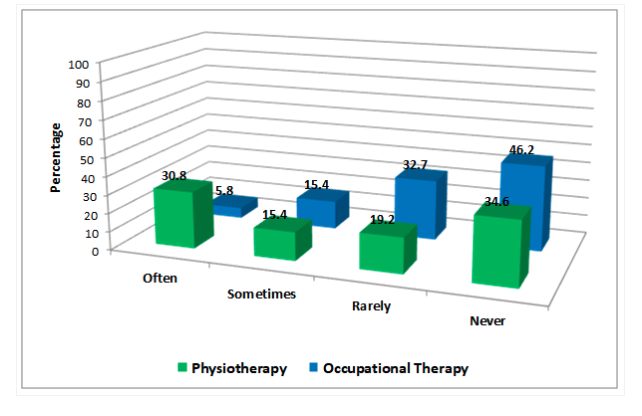
Survey responses on referral patterns suggest that most audiologists rarely or never suggest a referral to occupational therapy or physiotherapy when someone has a history of falls. Of those that do (often or sometimes), physiotherapy (46.2%) is more commonly suggested compared to occupational therapy (21.2%). Falls are an interdisciplinary issue, and understanding the roles of other professionals on the team and when to refer is essential. These survey results demonstrate that the lack of fall risk screening tools in audiological practice serves as a significant barrier to making referrals to relevant health care professionals. Therefore developing a fall screening protocol is an essential first step. Audiologists are encouraged to reach out to their local physiotherapists and occupational therapists and ask about referral pathways for private and public services to know how and when to suggest a referral. The extra benefit of creating this dialogue will be reciprocal referrals which will enhance services for patients. Some clinics or hospitals offer an interdisciplinary Falls Clinic specifically targeting those at risk of falls. Make sure you understand how and when to refer to these specialty clinics (see Figure one).
For a further review of survey results, please click the following link:
https://canadianaudiologist.ca/striking-the-right-balance-4-6-feature/
November is Fall Prevention Month! To help support Audiologists, the following step-by-step guide was developed outlining how to perform and score three common fall risk screening tools: the Four Stage Balance Test, the 30-Second Chair Stand, and the Timed Up and Go. These tests are simple to perform and can be used by all health care professionals. In addition, they are recommended by the CDC STEADI Initiative for health care providers to screen, assess, and intervene to reduce fall risk.
Step-by-Step Guide to Fall Risk Screening
Four Stage Balance Test
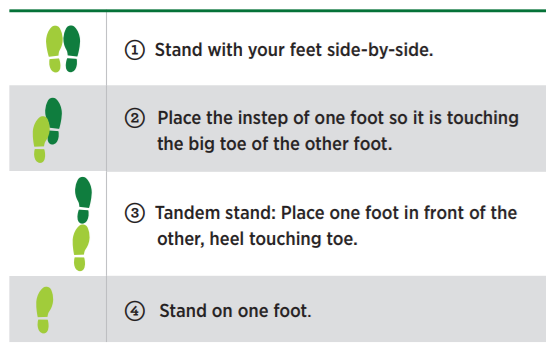
Purpose
The Four-Stage Balance Test screens patients’ static balance – the ability to maintain a stable position, which is a critical component in postural stability. This ability can deteriorate in patients with impaired vestibular organs and/or other disorders like Parkinson’s disease. This test involves putting the patient into 4 different standing positions, each becoming increasingly difficult, and the patient must attempt to maintain each position for at least 10 seconds.
Equipment
- Stopwatch
Steps
- Make sure the testing environment is safe and remove any potential hazards.
- Tell the patient that you will describe and demonstrate four different standing positions; they must try to stand in each position for 10 seconds. They can hold their arms out and move their body to maintain balance but must not move their feet. Their eyes should be open.
(Note: Patient should not use assistive devices like canes or walkers during the test)
- Stand next to the patient, hold their arm, and help them assume the correct foot position. When the patient is steady and ready to begin, let go of the patient and begin timing with a stopwatch.
- If the patient can hold a position for 10 seconds independently without assistance or moving their feet, stop the timer and move onto the next position. If the patient cannot do so, stop the test. Be ready to assist the patient should they be unable to maintain balance independently.
Sample instruction to patient: “I will show you four different positions. Try to stand in each position for at least 10 seconds. You may hold your arms out or move your body to maintain balance but do not move your feet. Maintain the position until I say “stop.”
Interpretation
Fall risk
If the patient cannot hold positions 2 or 3 for 10 seconds or longer, or if they cannot stand on one foot for 5 seconds or more, it may suggest increased fall risk, and further assessments and interventions may be required.
30-Second Chair Stand
Purpose
The 30-second chair stand is a functional assessment of leg strength and endurance in older adults. It also assesses postural hypotension and, when used in combination with other balance screening tools, it can indicate if an individual may be at risk
Equipment
- Stopwatch
- Armless chair with solid back
Steps
- Begin by placing the chair up against a solid wall to ensure it does not move during testing. Then, demonstrate the task to the patient by performing a few chair stands both slowly and quickly.
- Seat the patient in the middle of the chair with their feet placed flat on the ground, shoulder-length apart, and their heel placed slightly back from the knees. Place one foot slightly in front of the other to help maintain balance and have the patient cross their arms at the wrists and place their hands on the opposite shoulder.
- Have the patient do a practice set of 2-3 chair stands before starting the test. Ensure they are keeping their back straight and their arms against their chest.
- Inform the patient that they should attempt to complete as many stands as possible over a 30-second timeframe. The patient must completely sit between each stand for their stands to count.
- Inform the patient to begin on “Go” and have the clinician start their timer. This is where the patient will begin to perform as many chair stands as possible for 30 seconds. Stand next to the patient for safety in case they begin to fall.
- The clinician must tally each stand performed by the patient within the 30-second timeframe. At the end of the 30 seconds, if the patient is more than halfway up to a stand, it counts as a full stand. Incorrectly executed stands are not counted. If the patient must use their arms to stand, stop the test and score them with a 0. If you feel that the patient is at risk for falling during testing, stop the test and take their current score.
Interpretation
Depending on the population being assessed, there are different normative values that should be considered, including age or specific health conditions.
Normative data have been established for moderately active older adults by Rikli & Jones and regular community-dwelling adults. Ensure the correct normative values are being used depending on the activity level of the patient. Pediatric normative values have not yet been established.
Table 1. Average Chair Stands per 30 Seconds by Age
| Age Group (years of age) | Average Chair Stands (Women) | Average Chair Stands (Men) |
| 60-64 | 12-17 | 14-19 |
| 65-69 | 11-16 | 12-18 |
| 70-74 | 10-15 | 12-17 |
| 75-79 | 10-15 | 11-17 |
| 80-84 | 9-14 | 10-15 |
| 85-89 | 8-13 | 8-14 |
| 90-94 | 4-11 | 7-12 |
Table 2. Average Chair Stands per 30 Seconds for Moderately Active Older Adults
| Age | # Of Stands (Women) | # Of Stands (Men) |
| 60-64 | 15 | 17 |
| 64-69 | 15 | 16 |
| 70-74 | 14 | 15 |
| 75-79 | 13 | 14 |
| 80-84 | 12 | 13 |
| 85-89 | 11 | 11 |
| 90-94 | 9 | 9 |
Table 3. Osteoarthritis Normative Scores
| Osteoarthritis Population | Average Chair Stands |
| Hip OA | 10.1 (+/- 4.4) |
| OA of hip/knee (does not need gait aid) | 7.3 (+/- 2.8) |
| OA of hip/knee (requires gait aid) | 4.5 (+/- 3.3) |
Timed Up and Go (TUG)
Purpose
Falls can be a great threat to the elderly population due to various risk factors that they possess, and the TUG assesses some of those risk factors, including impaired postural stability. In this test, the patient must stand up from a chair, walk back and forth, and then sit back down, all of which require postural stability. In addition, the time it takes an individual to complete this task has been correlated with fall risk.
Equipment
- Stopwatch
- Chair with arms
- Measuring tape
- Place marker of choice* (e.g., tape on the floor)
*Ensure place marker is not something that the patient could trip on
Steps
- Set up: Place a chair with the back resting against a wall to minimize chair movement during the test. Measure 3 meters distance in front of the chair and place your marker of choice at that distance. Ensure that the room choice is appropriate to perform the test (open space, no obstacles).
- Patient instructions: The patient will begin by sitting in the chair. Instruct the patient that on “Go,” they will stand up from their seated position, walk forward until they reach the place marker, turn around, walk back, and sit back down in the chair.
- Let the patient know that they will be timed for this task, but walk at a safe and comfortable pace.
- If the patient requires a walking aid, ensure that it is accessible.
- If needed, have the patient repeat back the test instructions to verify that they understand the task.
- Begin the test. The patient is allowed one practice round to familiarize with the test, and the second time they should be timed.
Interpretation
The scoring for this test is straightforward. If the patient takes 13.5 seconds or less to complete the test, that is considered a typical result. If the patient takes more than 13.5 seconds, they are considered to be at a higher risk of falling. This test will typically be done in conjunction with a variety of other screening tools to get an overall impression of the patient’s fall risk (low, moderate, or high), and you would include this in your report. It is important to remember that this is a screening tool, so a typical result does not necessarily mean that you will never fall.
Bibliography
- American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148–57.
- Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:993–998. DOI: http://dx.doi.org/10.15585/mmwr.mm6537a2
- Centers for Disease Control and Prevention. (2021, July 26). STEADI - Older Adult Fall Prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/steadi/index.html.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web–based Injury Statistics Query and Reporting System (WISQARS) [online]. Accessed August 5, 2016.
- Criter RE, and Honaker JA. Audiology patient fall statistics and risk factors compared to non-audiology patients. Int J Audiol 2016; 55(10):564–70.
- Criter R. Falls in audiology patients [PowerPoint slides]. As presented at the World Congress of Audiology XXXIII on September 20, 2016 in Vancouver, BC.
- Danhauer JL, Johnson CE, Newman CW, et al. An open letter to Dennis: We can do more to educate our patients about falls risk. Audiol Today 2011;23(5):58–69.
- Jacobson GP and Shepard NT.Balance Function Assessment and Management (Second Edition).Plural Publishing Inc; 2016.
- Jiam NT, Li C, and Agrawal Y. Hearing loss and falls: A systematic review and meta-analysis. Laryngoscope 2016;126(11):2587–96.
- Ko CW, Hoffman HJ, and Sklare DA. Proceedings from 29th mid-winter meeting of the Association for Research in Otolaryngology (ARO): Chronic Imbalance or Dizziness and Falling: Results from the 1994 Disability Supplement to the National Health Interview Survey and the Second Supplement on Aging Study. Baltimore, MD; 2006.
- Lin FR and Ferrucci L. Hearing loss and falls among older adults in the United States. Arch InternMed 2012;172(4):369–70.
- Patterson JN and Honaker JA. Survey of audiologists’ views on risk of falling assessment in the clinic. J Am Acad Audiol 2014;Apr;25(4):388-404. doi: 10.3766/jaaa.25.4.10. PMID: 25126686.
- Physiotutors. The Timed Up and Go Test (TUG) | Fall Risk Assessment [Video]. Youtube. 2016. https://www.youtube.com/watch?v=grrYoBucNPE&ab_channel=Physiotutors
- Public Health Agency of Canada. Seniors’ Falls in Canada: Second report. Ottawa: Author 2014. Available at: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/seniors-aines/publications/public/injury-blessure/seniors_falls-chutes_aines/assets/pdf/seniors_falls-chutes_aines-eng.pdf
- Rikli RE and Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Activity 1999;7:129-161.
- Rikli RE and Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60-94. J Aging Phys Activity 1999;7:162-181.
- Shumway-Cook, A, Brauer S and Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther 2000;80(9):896-903.
- Wright AA, Cook CE, et al. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther 2011; 41(5):319-327.