Striking the Right Balance: My Vestibular Migraine Journey
In this edition of “Striking the Right Balance,” Erica Zaia, MSc. RAUD documents her personal experience with vestibular migraine.
Michael Vekasi, AuD, R.Aud, Aud(C), FAAA and Erica Zaia, MSc, RAUD are coordinating the “Striking the Right Balance,” feature which will cover the latest information on ‘all things vestibular.’ If you would like to be more involved in all things vestibular, please check out and like our Facebook page by searching for “CAA National Vestibular Special Interest Group” within Facebook. You can also reach us by email at CAAvestibular@gmail.com.
By Erica Zaia
It is the first week of July and instead of planning activities for the long-awaited Summer, this sunshine-loving Brazilian is having English lessons. Someone was “nice” enough to tell me: “you look like you were pulled through a knothole backwards.” I needed to search the expression up to realize I certainly felt like that, after 4 weeks of vestibular migraine and chronic migraine headaches.
Fast rewind to early June, so you can follow my journey through the knothole backwards: I worked full-time and much more. As a clinic owner and solo practitioner, I perform all the duties, from cleaning and purchasing supplies to bookkeeping, and from office assistant, answering the phone and overseeing scheduling, to actually seeing patients, writing reports, and sending them to appropriate parties. In addition to that, I teach and mentor professionals across the country, and I am creating a course with the wonderful people at Pacific Audiology Group. I also volunteer on the Board as a president of Balance and Dizziness Canada and do more volunteer work with the Canadian Academy of Audiology (CAA) and Speech-Language and Audiology Canada (SAC). I live by myself and care for my house, car, and everything else on my own. I nurture a delicate relationship with a teenage son who lives with my ex-partner, and I was dating someone who thrived on doing strenuous physical activities, even after nights in which sleep was interrupted several times by some serious health concerns of his. And I am doing all of that while going through the interesting phase of perimenopause and playing with different hormone replacement regimens. Although I don’t suffer from motion sickness and can read leisurely in any means of transportation, I have a strong personal and family history of migraines and had my first episode of migraine with aura when I was around 8 years old. If you are not yet picturing a hurricane being generated in my brain or doing the countdown to an old building being imploded (my brain!), I will give you a different visual. Imagine a measuring tube like the ones in a chemistry lab. Now imagine all of the factors above being poured into the cylinder. It would look like this.
This the perfect depiction of the concept that migraine is a threshold disorder. Ideally, I would want to stay with what I cannot change within my lifetime: my genetic load. I was, instead, slowly adding insults to my central nervous system until I was ready for the straw that broke the camel’s back. One day in early June, I fell funny while indoor bouldering and twisted my ankle and hip. The joint pain was the last addition that sent me over the threshold, and I started having migraine headaches.
That is how it goes. Once the migraine threshold is reached, there will be symptoms – a migraine episode. For a few lucky people, going over the threshold of migraine activity in the brain only generates visual disturbances, like a kaleidoscope, a halo, a dark “filter” on the eyes. These are called ocular migraines. Episodes only last about 20 minutes and go away, in a very benign manner. The episodes most people are familiar with are migraine headaches, which by definition are moderate to severe throbbing headaches with either sensitivity to light, sound and/or nausea, that get worse with physical activity. It is the kind of pain that sends you to a dark, quiet room and that feels as though someone is splitting your head open. That is the pain I started having when I was 8 years old.
Interestingly, before that I had endured about a year of unexplained abdominal pain – which my mom thought was “psychological” because I did not like my grade 2 teacher. Abdominal migraines are common in school-aged girls who will become classic migraineurs. Many adult women who suffer from migraines continue to have gastrointestinal issues and are diagnosed with irritable bowel syndrome. The correlation between the gut and the brain has been studied recently and is by now well established – there are about 500 million neurons in the enteric system.
Migraine episodes can also manifest as vestibular symptoms. I will take you back to my Summer tale to get into those. After a few consecutive days of migraine headaches, when Ibuprofen would not even make a dent on the pain, I started having nausea, a constant low-pitched loud buzzing and roaring in my head, fullness in both ears and a sensation of being drunk, dizzy, literally bouncing off walls. I would wake up already in pain, nausea, and feeling drunk. Yet, it was June, my clinic schedule was full and all my commitments were there. I did not stop, I pushed through. I had a hard time thinking clearly and would stop speaking with patients every so often just to put my thoughts together. I needed to take breaks and nap almost every day, and even then I was still extremely tired and having difficulty concatenating my thoughts. I asked my doctor for a referral to a migraine specialist I know, and the few weeks of waiting were literally agonizing to me. I am in the roughly 40% of people for whom vestibular migraine symptoms are constant and not episodic. This presents a diagnostic challenge as this is not captured in the classic criteria for vestibular migraines that describes “episodes lasting up to 3 days”. As a vestibular audiologist and migraineur, I knew what was going on with me, and I knew I needed prescription medications. I had already started paying closer attention the first line of defense against migraines, the lifestyle strategies SEEDS for success, which is an acronym for:
- Sleep: maintaining a regular bedtime and wake-up time and striving for restorative sleep. No more sleep interruption by someone else’s health concerns was key to my recovery.
- Eat: following a diet, avoiding known migraine triggers such as dairy products, alcohol, sugar, and processed foods, among others.
- Exercise: practicing regular moderate exercise. Re-starting an exercise program was the hardest thing for me but I am glad I persisted.
- Dehydration: drinking lots of water consistently, every day.
- Stress: Working at not holding stress and engaging in mindfulness meditation and other grounding practices was lifesaving.
I increased my dosage of the supplements proven to help with migraines and vestibular migraines and went up to 400 mg of each magnesium and vitamin B2 and 2000 IU of vitamin D3.
Seeing the migraine specialist was validating, which cannot be underestimated, and invaluable. Headache abortive medications and preventative medications were prescribed and I was lucky to find drugs that did provide me with much-needed relief. There are several classes of abortive pain drugs, such as anti-inflammatories (diclofenac – Cambia powder), triptans (such as rizatriptan – Maxalt and sumatriptan – Imitrex), and gepants (ubrogepant – Ubrelvy). These are taken as needed, as soon as the headache starts. In addition, when the number of pain days exceeds 15 in a month and when other vestibular and aural symptoms are present, preventative medications, taken daily, are recommended. There are several classes of prescription medications available: low-dosage tri-cyclic antidepressants (amitriptyline – Elavil and nortriptyline – Aventyl), low dosage SNRI and SSRI (venlafaxine – Effexor and sertraline – Zoloft); low dosage anti-seizure (topiramate – Topamax); calcium-channel blockers (verapamil and flunarizine); beta-blockers (propranolol); antihistamines (betahistine – Serc); gepants (ubrogepant – Ubrelvy). I was lucky to find immediate relief in Cambia and surprised that Ubrelvy, a new, migraine-specific medication, did not even touch my pain. I was also fortunate that flunarizine, which I had taken in my 20s when I also had dizziness, helped me with all my vestibular symptoms.
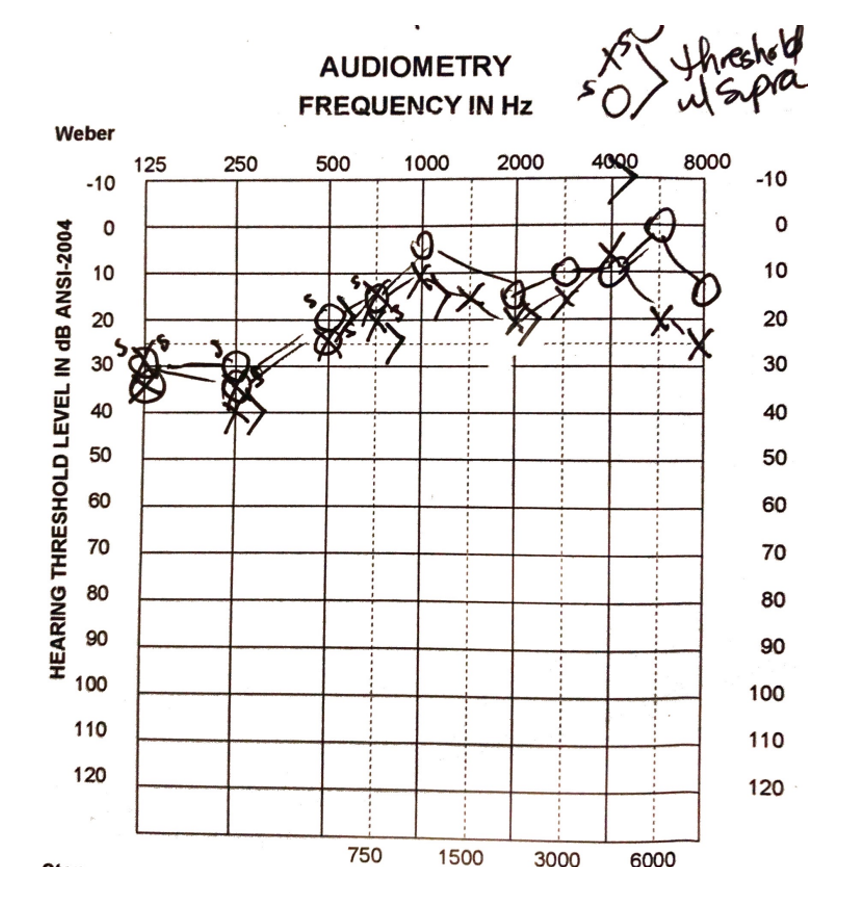
Early in August, when my aural fullness was still at its peak, this is what my audiogram looked like. I have to say that it was scary to see this hearing loss, though mild and likely temporary. We are still learning about vestibular migraine and how a neurological event causes peripheral damage. However, the aural symptoms including hearing and vestibular loss have been thought to be caused by neurogenic inflammation, causing constriction of blood vessels supplying the inner ear. I was also having intermittent vertical upbeating nystagmus, and my migraine specialist ordered an MRI to rule out any other sinister cause for my symptoms. I was relieved to see normal results on it.
I needed quite a few days of abortive medication from July to September, but with flunarizine, I started feeling more like myself in mid-August. I had a typical experience in the recovery stage. Symptoms became intermittent as opposed to mostly constant. They would be clearly triggered by overstimulation or overdoing in general and by breaking SEEDS rules: having a stressful day, eating or drinking something triggering, and not going to bed on time. I was still dealing with a lot of tiredness, and my need for rest only decreased in October.
I am now back to myself, humbled by this experience that made me feel even closer and more responsive to my patient’s needs. Knowing though that the strategies help and that getting back to normal life is possible fuels my motivation to keep raising awareness on vestibular migraine. If someone you know is affected by it, direct them to Balance and Dizziness Canada