Who Measures Otoacoustic Emissions?
From the Labs to the Clinics
Renowned auditory researcher Dr. Robert Harrison brings us up to date on information and research from the Labs. Appropriately titled “From the Labs to the Clinics”, Bob is involved in laboratory and applied/clinical research, including evoked potential and otoacoustic emission studies and behavioural studies of speech and language development in children with cochlear implants. For a little insight into Bob’s interests outside the lab and the clinic, we invite you to climb aboard Bob’s Garden Railway.
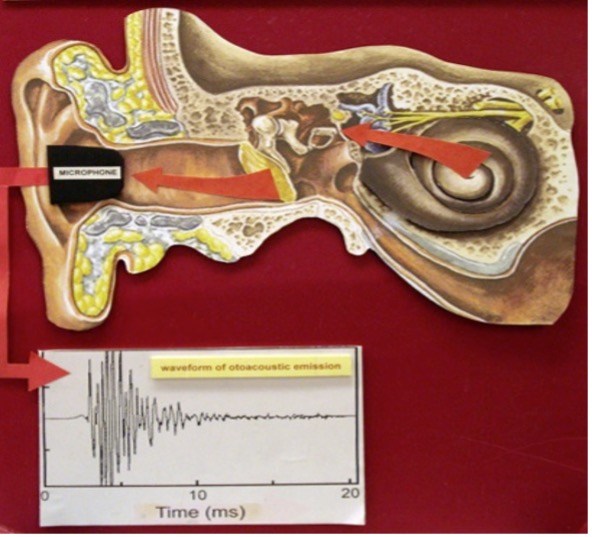
About six years ago, in my column in Canadian Audiologist, I celebrated the 40th anniversary of the discovery of otoacoustic emissions (OAEs) by David Kemp.1 I wrote about how sound coming out of the ears was initially regarded as paradoxical, and with some scepticism in the scientific and audiology community!2
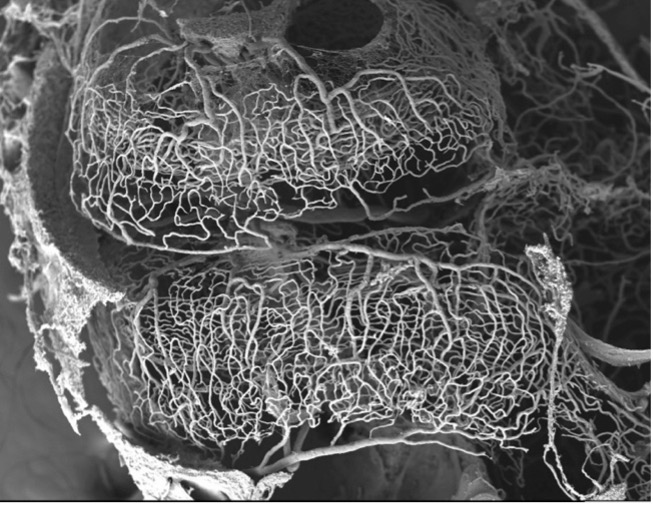
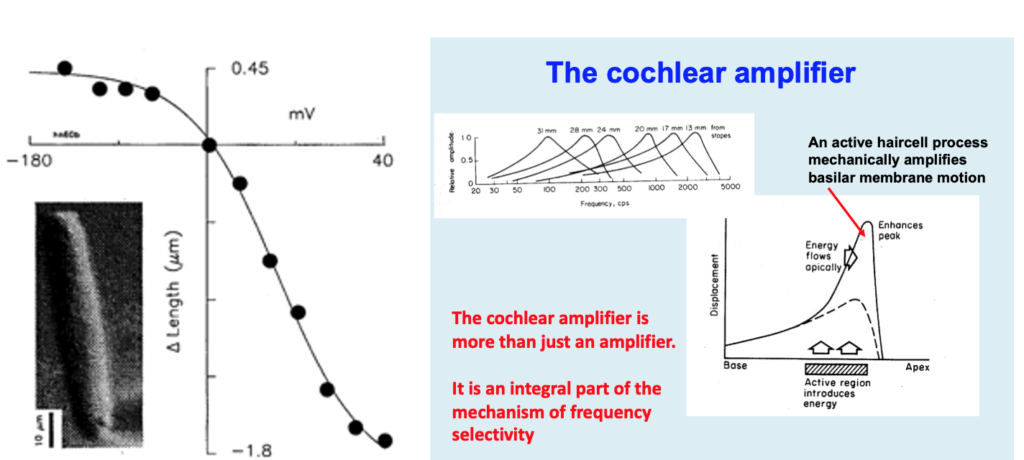
We now understand that the mechanical events that give rise to OAEs are generated by, arguably, the most important mechanism known to audiology, namely the cochlear amplifier. This is definitely my own opinion. The cochlear amplifier (so named by Hallowell Davis in the 1980s) is powered by the motility of hair-cells (mainly outer hair-cells) when they are activated.3,4 The power for this amplification effect ultimately comes from metabolic energy derived from oxygenated blood. This is why the blood capillary network of the stria vascularis is so extensive (See stria vascularis image in Figure 2).
When stimulated, small groups of outer hair-cells act in unison to amplify the movements of the Corti organ, thereby increasing the mechanical signal that activates inner hair-cell receptors. This amplification provides the exquisite (behavioural) threshold sensitivity of hearing that is most commonly measured in clinical audiometry. But the cochlear amplifier provides much more than just a signal gain. It is also responsible for the frequency analysis of acoustic signals that ultimately defines their meaning. For example, it allows coding vowel formant frequencies, speech intonation, syllable types, random versus structured noise, etc. Everything that we can hear and understand clearly, if we have normal hearing, is by virtue of the cochlear amplifier. Furthermore, the hearing deficits we most commonly encounter in subjects with sensorineural hearing loss are all caused by damage to the cochlear amplifier (Figure 3).
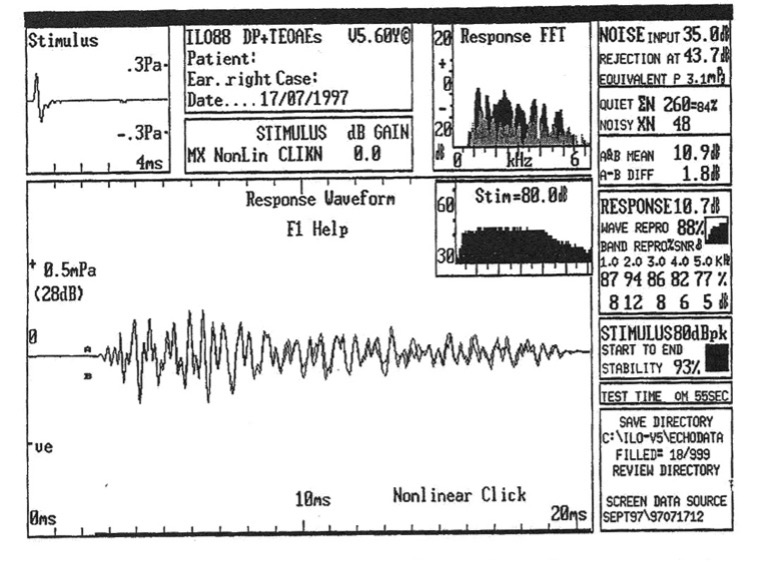
So now that we have established the importance of the cochlear amplifier, and that this mechanism generates OAEs, then it follows that OAE measurement can inform us about the core function of the cochlea. In other words, OAEs provide a window into the workings of the inner ear. At one level, we all know this because we appreciate the role that OAE testing plays in neonatal (newborn) hearing screening. But there is so much more: OAEs have an important (potential) role in defining the sub-types and the aetiologies of SNHL. Monitoring outer hair-cell function with OAEs can reveal deficits in the olivo-cochlear efferent pathways and thus how the central brain modulates cochlear function (Figure 4).
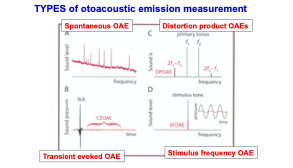
In my 2018 column, I opined that the full clinical potential of OAE tests (Figure 5) has not been reached, and I wondered (out loud) how many audiologists have used this tool in clinical practice. Since then I have found some answers. I have made a few surveys of audiology trainees that I teach worldwide in online Master’s and AuD courses. These trainees practice in countries far and wide (e.g., India, Australia, China, Iran, Saudi Arabia, Canada, UK, Germany, Israel, USA, and Columbia). The results were largely predictable. Anyone associated with hearing screening programs had experience with OAES. Those working in pediatric audiology used OAEs occasionally (e.g., for screening or for diagnosis of ANSD). Some “academic centres” had the equipment available and did occasional testing. Otherwise, in the adult realm there was next-to-no clinical use of OAE testing. Many audiology clinics did not have OAE measuring devices available. Some of my students admitted that they had never measured OAEs even during their clinical training!
As an auditory scientist I am left wondering why a methodology that can reveal the core workings of the cochlea and useful insights about pathophysiology, has not been adopted as a standard clinical tool. Given that my column is headed “from the labs to the clinics”, perhaps I should further explore why this area of knowledge translation appears to have faltered.
References
- Kemp, DT. Stimulated acoustic emissions from within the human auditory system. JASA 1978;64:1386-1391.
- Harrison RV. The biggest paradox in audiology. Canadian Audiologist 2018;Vol 5(2).
- Brownell WE et al. Evoked mechanical responses of isolated cochlear outer hair cells. Science. 1985;227:194–196.
- Brownell WE. Outer hair cell electromotility and otoacoustic emissions. Ear and Hearing. 1990;11; 82-92

