Some Interesting Cases in APD Evaluations
Interesting cases come our way every now and then. Here are a few to share with you on attention, unique response patterns to dichotic tests, and in assisting psychologists and families in understanding reliable auditory processing disorder (APD) test processes and results.
Understanding Reliable Test Administration
A mother indicates that her son’s teacher would like to know if indeed the child could be found with an APD four years after being diagnosed as not having an APD. The child’s clinical history is negative for a head injury or illness in these past four years. He has been evaluated by a neurologist to rule out attention issues. The mother was reassured that her son was reliably diagnosed without APD as attention was controlled and out of three CAP tests he showed no errors on two of the tests; and only two errors out of 160 possible errors on the third measure. The child did not receive a comprehensive psychological evaluation, as suggested four years ago, to rule out attention or learning issues. The mother reassured the clinician that she will pursue the comprehensive psychological evaluation!
Psychologists Controlling for Fatigue and Attention on APD Screening Measures
A psychologist inquires as to why some children are found without APD even though they have failed the APD screening measure 1 that he routinely administers as part of his psychological test battery. Reasons as to why audiologists control for fatigue and attention were explained: including providing the AP tests at morning sessions, in quiet surroundings and even when the client receives his/her prescribed medication for attention deficits. The psychologist changed his delivery mode to provide the AP screening test only at morning sessions and receives less false positive screening test results!
Expertise with the CAP Tests Assists to Decipher Unique Test Responses
A 12-year-old female presents with normal peripheral hearing and a negative comprehensive psychological evaluation. She demonstrated normal test results on the first two administered CAP tests. She received breaks between the peripheral hearing assessment and after the second CAP test.
The 3rd administered CAP test2 is a dichotic test of 40 sets of 4 words: 20 sets delivered first to the right ear alternating with 20 sets delivered to the left ear. The child provided exact errors of omitting the third word in each ear regardless if the right ear or the left ear first received the stimuli. See the below chart for examples of the child’s response pattern.
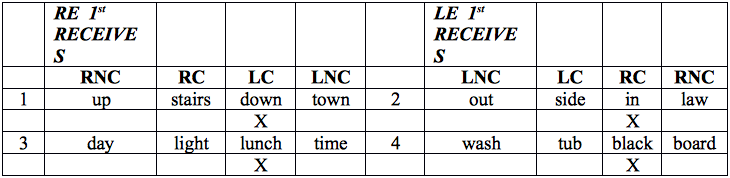
RC = right competing; LC = left competing; LNC = left noncompeting; RNC = right noncompeting. X: an error (in this case – omission of the test word)
The child provided the above response pattern for the first half of this test on all 20 sets. The dichotic test was stopped and the child was rescheduled to return in two weeks. Why? This response pattern was showing severe LC and RC error patterns – indicating two types of APDs: Decoding (RC errors), and Auditory Memory (LC errors). In 20 years I had never seen such a response. How could there be a severe RC score when the child has no clinical symptoms of Decoding APD? Yes, there could be an auditory memory issue, even though the psychological evaluation was negative on working memory deficit; however I was suspicious of such a ‘clean’ response pattern in only showing omission on the third word of each set. The child returned two weeks later and produced only four total errors out of 160 possible errors on this dichotic test. The child presented with normal auditory processing after also having a passing score on a fourth APD test!
If ‘inattention’ was the culprit, then the response pattern would have errors in all four of the measures: RC, RNC, LC, and LNC. This child, for some unknown reason, just omitted the third word on this dichotic test for all 20 sets. Fatigue you say? This is possible – although she had breaks and her response mode was identical for all 20 sets of words (the first half of the test). Usually we notice more errors toward the second half of the test when attention and fatigue are involved. What a unique case!
A Second Opinion
When a client arrives for a re-evaluation, six months or longer after the initial diagnosis, I remain blind to the previous test scores until I have completed the test battery. Then, I compare the previous and current test results after I have administered the APD test battery, scored all test results and discussed the current results with the client/family. For all evaluations I encourage the parent(s) to attend the session to observe the child’s strengths (e.g., responds appropriately to all stimuli) or weaknesses (e.g., shows omissions, delays, quick responses, need for re-instruction, etc.).
An eight-year-old male presented with normal peripheral hearing and inattention issues in the school setting. He ‘failed’ an APD evaluation eight months prior at another clinic. His pediatrician provided a letter to the school indicating that inattention was a diagnosis (without a true evaluation for this diagnosis). The school provided the child with extended test taking time, and he did not receive APD therapy in the past eight months. (The school professionals were concerned with the initial APD evaluation results).
These are the errors obtained on the current and previous dichotic test, eight months apart:
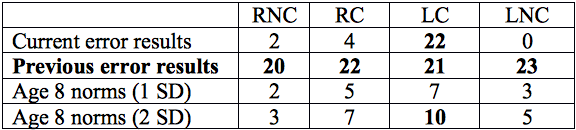
It was alarming to observe the previous test results, showing that all test scores were quantitatively similar and all were at 50% errors. (There are 40 possible errors for each of the four measures.) This test outcome indicates a serious organic pathology or the clinician did not control for attention. Incidentally, the client’s pediatrician ordered an MRI with negative results.
The current evaluation of 22 LC errors is a classic error pattern for the Tolerance-Fading Memory (TFM) (auditory memory deficit) and possibly Integration APD. The normal LNC and RC errors rule out Decoding type of APD.
The parents, who observed the current evaluation session, were educated on test score comparisons. The child will be receiving APD therapies and strategies for his types of APD, and a comprehensive psychological evaluation with a reputable psychologist to ascertain of any attention or learning issues. The child’s school professionals were relieved that the current APD evaluation revealed reliable test results.
Was attention a factor at the previous evaluation? Probably – due to the negative MRI and that all four measures had identical quantitative scores. If we could review the test scoring form of the child’s responses we could check for:
- the last half of the test responses versus the first half of the test responses. It is common to see the last half of the tests having more errors than the initial half of the test when inattention is an issue.
- the type of errors: omissions versus a word error
- any notation of provided breaks
- the presence of quick responses resulting in forced errors.
All of this information provides qualitative and quantitative test response data associated with types of APD or possible inattention.
References:
- Keith RW. SCAN-3:A Tests for Auditory Processing Disorders in Adolescents and Adults (SCAN-3:A). SCAN-3:C Tests for Auditory Processing Disorders for Children (SCAN-3:C). San Antonio, TX: Pearson; 2009.
- Katz J and Fletcher CH. Staggered Spondaic Word (SSW) Test. Vancouver, WA: Precision Acoustics. Available at: http://precisionacoustics.org/.

