Striking the Right Balance – Posterior Canal BPPV Clinical Variation: Beyond the Commonest Type!
Benign paroxysmal positional vertigo (BPPV) is a mechanical peripheral vestibular disorder which may involve any of the three semicircular canals by displaced otoconia, making them gravity sensitive. It is characterized by brief positional episodes of spinning vertigo. Because of its anatomical position, the posterior canal (PC) is by far the most frequently involved. Classical type of posterior canal benign paroxysmal positional vertigo (PC-BPPV) produces a characteristic upward and torsional nystagmus directed toward the down ear (the upper pole of the eye beating towards the affected ear) when the individual is placed in the Dix-Hallpike (DH) position1.
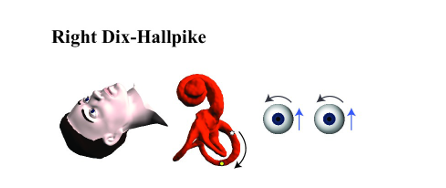
Figure 1
The free-floating otoconia settle in the most inferior portion of the PC and move away from the ampulla when placed into the DH position, creating deflection of the cupula within the PC ampulla. According to Ewald’s second law, this ampullofugal flow of endolymphatic fluid results in excitation of the respective PC, and the stereotyped pattern of nystagmus are observed.1
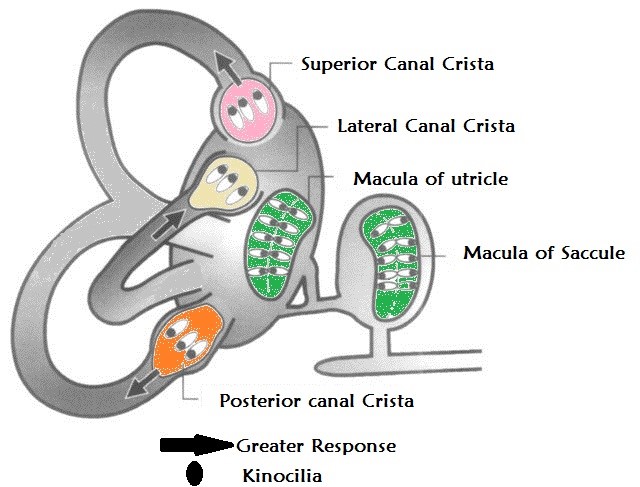
Figure 2 shows Ewald’s Laws of labyrinthine Function: 1st: The axis of nystagmus parallels the anatomic axis of the SSC that generated it 2nd: Ampullopetal endolymphatic flow produces a stronger response than ampullofugal flow in the lateral canals 3rd: The opposite is true of the vertical canals.
However, if the otoconia are instead aggregated outside of long arm of the PC, in the distal, non-ampullary arm of the posterior canal, close to the common crus Dix-Hallpike testing may produce an atypical pattern of nystagmus due to the altered direction of endolymphatic flow (ampullopetal). In the DH position, the otoconia fall away from the common crus but fail to enter the long arm of PC canal. This results in ampullopetal endolymphatic flow, deflecting the cupula in a manner that inhibits the PC.2
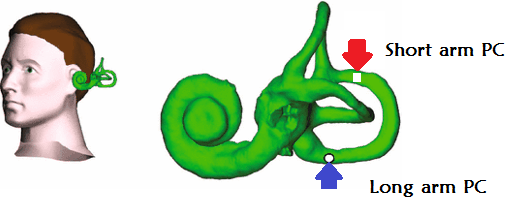
Inhibition of the PC produces a fast phase nystagmus that is downbeating with a torsional component directed away from the involved ear.2 This atypical variant of PC-BPPV has been named ‘apogeotropic’ PC-BPPV, as the downbeating nystagmus is directed away from the ground during DH testing, contradictory to the up beating or ‘geotropic’ direction of nystagmus seen with Typical pattern of PC-BPPV.2 In patients with apogetropic PC-BPPV, the positional nystagmus is not only perverted, but is characterized by a low intensity and persistent pattern, a stark contrast to the brief and robust Nystagmus associated with Typical PC-BPPV.2–4 Additional features of apogeotropic posterior canal BPPV (APC-BPPV) positional nystagmus include provocation with either DH, an immediate onset of symptoms and/or nystagmus, an inability to fatigue the nystagmus on repeat positional testing, and stronger symptoms when moving into an upright position from supine without a reversal of positional nystagmus.2
Califano et al. has found a tendency for APC-BPPV to produce stronger torsion, where Vanucchi et al. describes a mild torsion with more pronounced downbeating.2–4
Apogetropic PC BPPV Management: Two treatments have been proposed: the second half of the Semont maneuver, which the patient begins by sitting upright with legs hanging over the edge of the bed, the head rotated toward the unaffected ear; then whilst maintaining this head position, lying onto the unaffected side, allowing the otoconia to fall into the common crus and finally into the vestibule.2 The second treatment, termed the “45-degree forced prolonged position”, requires patients to lie on the unaffected side with the head turned 45° downwards, to bring the non-ampullary arm of the affected posterior canal into a draining position, and to maintain this position for 8 hours.
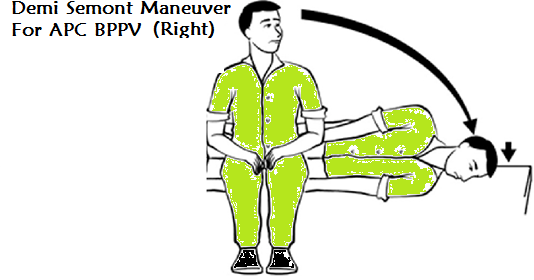
Figure 4
Three Clinical Gems
1. When an individual presents with down-beating and torsional nystagmus during DH testing, it is not immediately evident whether the nystagmus is secondary to excitation of the AC ipsilateral to the direction of torsion, inhibition of the PC contralateral to the direction of torsion, or as a result of altered central processing.2,6–8 The above characteristics of Apogetropic PC-BPPV can guide the clinician toward an appropriate diagnosis; however, a clear diagnostic guideline has yet to be developed. A thorough history and clinical exam must be completed in patients with positional down-beating nystagmus to rule out traditional causes of positional down-beating nystagmus including anterior canal BPPV (AC-BPPV) and central positional nystagmus.5,6,8–10
| Pattern of positional Nystagmus | Provocating Test | BPPV Variant |
| Up beating and torsion toward the affected side | Dix-Hallpike in affected side | Typical (Geotropic PC BPPV ) |
| Down beating and torsion away from affected side | Dix-Hallpike on either side | Apogetropic PC BPPV |
| Down beating and torsion toward the affected side | Dix-Hallpike in either side | Anterior Canal BPPV |
2. Presence of deviations to the diagnostic criteria for benign paroxysmal positional vertigo (BPPV), additional nystagmus characteristics of latency, duration, fatigue, and response to repositioning maneuvers must be considered in order to differentiate central positional nystagmus (CPN) from the peripheral nystagmus (PN) attributed to BPPV and its variants.10
3. It is important to note that BPPV is very common and may co-exist with brain structural/functional pathology. With this in mind, the presence of features atypical for BPPV should warrant further investigation, even if BPPV has been diagnosed. Similarly, positional vertigo may be the only precursor symptom of a central nervous system disorder.11
References
- Gold DR, Morris L, Kheradmand A, et al. Repositioning maneuvers for benign paroxysmal positional vertigo. Curr Treat Options Neurol 2014;16:307.
- Vannucchi P, Pecci R, Giannoni B, et al. Apogeotropic posterior semicircular canal benign paroxysmal positional vertigo: Some clinical and therapeutic considerations. Audiol Res 2015;5:38–43.
- Vannucchi P, Pecci R, Giannoni B. Posterior semicircular canal benign paroxysmal positional vertigo presenting with torsional downbeating nystagmus: an apogeotropic variant. Int J Otolaryngol 2012;2012:1.
- Califano L, Salafia F, Mazzone S, et al. Anterior canal BPPV and apogeotropic posterior canal BPPV: two rare forms of vertical canalolithiasis. Acta Otorhinolaryngol Ital 2014;34:189–97.
- Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. J Clin Neurol 2015;11:262–67.
- Casani AP, Cerchiai N, Dallan I, et al. Anterior canal lithiasis: diagnosis and treatment. Otolaryngol. Head Neck Surg 2011;144:412–18.
- Buttner U, Helmchen C, Brandt T. Diagnostic criteria for central versus peripheral positioning nystagmus and vertigo: a review [Internet]. Acta Otolaryngol 1999;119:1–5.
- Choi JY, Glasauer S, Kim JH, et al. Characteristics and mechanism of apogeotropic central positional nystagmus. Brain 2018;141:762–75.
- Macdonald NK, Kaski D, Saman Y, et al. Central positional nystagmus: a systematic literature review. Front Neurol 2017;8:141.
- Choi J-Y, Kim JH, Kim HJ, et al. Central paroxysmal positional nystagmus: characteristics and possible mechanisms. Neurology 2015;84:2238–46.
- Bertholon P, Antoine JC, Martin C, Michel D. Simultaneous occurrence of a central and a peripheral positional nystagmus during the Dix-Hallpike manoeuvre. Eur Neurol 2003;50:249–50.10.1159/000073868.

