Realizing the Benefits
of Group Aural Rehabilitation in Newfoundland
An Innovative Knowledge Translation Approach to Improve Outcome for Hearing Loss in a Specific Rural Environment
Introduction
Funded by a 2019 IDA Institute clinical research grant, audiologists Anne Griffin and Taylor Burt aimed to explore how the benefits of group aural rehabilitation1-6 could be made accessible to people with hearing loss in rural Newfoundland. At the Genomic-Based Research and Development Centre for Health7 in central Newfoundland, input from research participants and community members with hearing loss has identified gaps in care for hearing loss and created an opportunity for applicable research and service. Specific common concerns seem ideal for group discussion and learning, where experience and resources shared by peers and clinicians could provide valuable help for mitigating hearing loss impact in these domains. However, low and inconsistent attendance have discouraged audiologists from attempting group learning sessions in rural Newfoundland. A person-centred approach8,9 was proposed, focusing on topics reflecting real-life concerns of participants and tailoring delivery to the rural context of Central and Western Newfoundland, where the majority of hearing loss clients drive a considerable distance to access services.10,11 Investigators hoped to illuminate a way for clinicians to leverage the power of group connection to enhance care for hearing loss and optimize resources.
Due to the pandemic, the completion of the project was delayed by one year. This was unexpectedly advantageous for the assessment of the outcome. Gillian Ash (audiology candidate) and Katelyn Adey (health sciences student) recruited two additional team members to complete follow-up and strengthen the project for current conditions by adding a trial of group aural rehab delivered online.
Method
Three stand-alone workshops were developed to address three identified needs: the difficulty of hearing in community activities, the impact of hearing loss on close relationships, and the desire to be better informed about hearing technology. Of the four planned sessions per workshop, nine were conducted between July and November 2019 in Grand Falls-Windsor and Corner Brook, two towns that serve as hubs for rural services.11 Each workshop was prominently advertised as hearing accessible, and 35 participants from multiple communities affected by hearing loss of widely variable severity registered for one or more workshop(s), choosing their preferred location and time of day.
Each workshop was designed to provide insight on hearing loss and communication breakdown, build knowledge and capacity, and facilitate personal goal setting for actions that could result in sustained benefit. Communication partners were welcome at all workshops.
Inclusiveness for full participation was enabled through three modalities of accessibility technology (amplification, FM, and live remote transcription) and seating arranged to ensure line of sight for all participants, presenters, projected slides, and captions. All participants were oriented to the accessibility measures, asked to try them out personally and continue using them if they made understanding easier. Everyone was also respectfully requested to ensure accessibility for all by waiting for the microphone, holding it correctly to speak, and not blocking the line of sight for others.
Individual ratings on Ida Institute’s tool “The Line”12 were requested as the workshop began and ended, and again at the follow-up interview, as a simple method for participants to identify changes indicative of learning and benefit. Three topic-related questionnaires were selected as an additional measure of beneficial change, administered before each workshop and during the follow-up interview. Other Ida Institute tools were used to facilitate interaction. Local clinicians with expertise relevant to the topic were involved in workshop development and presentation. As initially planned, follow-up interviews were conducted 18-24 months post workshop instead of 3-6 months post-workshop.
Workshop 1: Living with Hearing Loss in Your Community: Challenges and Strategies for Community Interaction
Sixteen participants first completed the Telegram13, a tool to rate hearing difficulty and knowledge in 8 areas (Telephone, Employment/education, Legislation (re accessibility), Entertainment, Groups, Recreation, Alarms/alerting signals and family Members).
Using the Living Well tool12, participants then shared situations in community life where hearing is challenging and how they adapt accordingly. Capacity building focused on knowledge of accessibility legislation,14 and strategies, and resources for working in their community to enact change. Participants were encouraged to identify a specific barrier, resources required and set one personal goal for positive action.
Workshop 2: Hearing Loss and Close Relationships: Stresses and Solutions
Communication partners were invited to engage with participants in this exploration of the impact of hearing loss on close relationships. Sixteen participants first completed the Self-efficacy for Situational Communication Management Questionnaire (SESMQ).15 A psychologist or social worker joined each session to discuss mental health in relationships, assist communication partners in reflecting on how hearing loss impacts their own journey, and provide support in potentially stressful discussions of communication breakdown and maladaptation.
Ida Institute tools, including the Communication Rings, the Patient/Partner journey, and the Circle12 were used to facilitate reflection and discussion. Tools were modified for ease of use in a group and for understanding. For example, the Circle tool was simplified, and stages gave interpretative sub-titles, such as “not on my radar,” to explain the “pre-contemplation” stage of behavioural change. The Goal Sharing for Partners exercise12 was combined with instruction on setting SMART goals (Specifc, Measurable, Achievable, Relevant and Timely).16
Workshop 3: Technology for Hearing Loss: Getting the Best Value for Your Hearing and Your Life
The Hearing Aid Skills and Knowledge Inventory – Self –Administered (HASKI-self)17 was selected as the independent questionnaire but was abandoned on finding it either inapplicable or too burdensome for registrants to complete. A local clinical audiologist helped develop and deliver this workshop which aimed to identify and validate questions about technology, provide context and information, and facilitate increased confidence and competence to optimize interaction with providers and technology. The Box tool12 was used informally during the discussion to help participants recognize criteria critical to their choices. The eleven participants were encouraged to set one goal related to improving their hearing experience through effective use of technology.
Follow-up Interviews
Participants had selected either phone call, facetime call, or email as their preferred modality for follow-up communication; however, all participants ultimately preferred to be interviewed by phone, even when this critical interpretation required help from a family member.
Given the interval of nearly 2 years between workshop attendance and follow-up, participants were first assured that memory of workshop details was unnecessary to provide valuable input. Therefore, interviews were conducted as a conversation about the topic, the experience of participating in the workshop, and personal progress. During the interviews, the line exercise and questionnaires associated with Workshops 1 and 2 were also completed. The seven participants who attended more than one workshop were interviewed about each on separate occasions. Thirty-seven interviews of a possible 43 were conducted, a response rate of 86% overall.
Key Findings
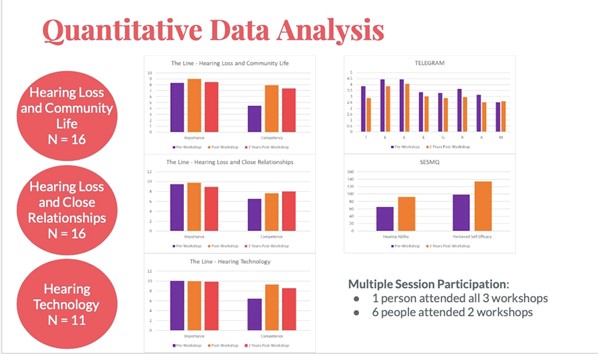
From the Line exercise, ratings of the importance of topic were high for all workshops and remained high, indicating the salience of these person-centered topics to participants. Though statistically significant differences in competence ratings were only seen for workshop #1, competence ratings for all workshops trended upward from pre- to post-workshop and remained high even 2 years post-workshop.
Results from the Telegram questionnaire do not vary with statistical significance from pre-workshop to follow-up interview but appear to trend downward, suggesting increased difficulty in almost all areas assessed. Changes in Telegram scores were somewhat difficult to interpret given a lack of norms, and some scoring ambiguity. However, the change in scores may reflect additional difficulty experienced in community situations due to barriers, masks, and social distance implemented since the workshop.
Results from the SESMQ showed a significant increase in both hearing ability and perceived self-efficacy from pre-workshop to 2 years post-workshop. Though it is difficult to know if pandemic-related reduced listening environments and communication partners may have influenced scores, this finding suggests sustained benefit.
Qualitative/Interpretive
Follow-up interviewing provided insight on specific benefits perceived by participants and topic-related examples of positive action that improved outcomes. Benefits described are categorized in three distinct themes; connection and support from the group experience, awareness and learning achieved, and examples demonstrating increased self-efficacy and personal empowerment related to the workshops attended.
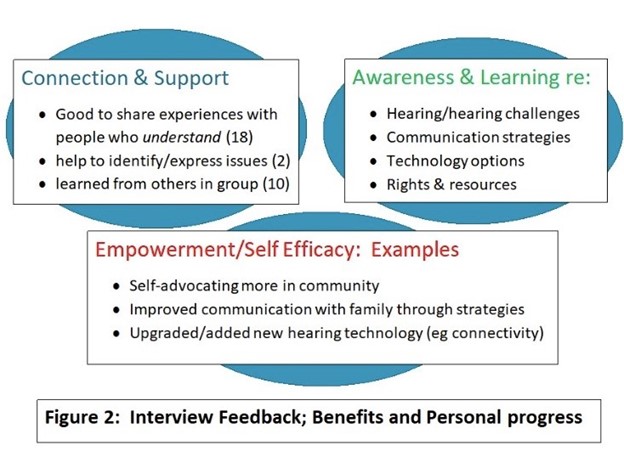
These findings illuminate and reinforce quantitative indications of sustained benefit related to workshop attendance. In contrast to concerns that follow-up interviews would be less revealing after the extended interval, participants had more time to translate gains from workshop attendance to positive action and improved outcome, and data was richer than expected. Of particular interest were participants who reported that listening to other participants helped them find words to express their own concerns. Examples of improved communication reduced frustration within families by implementing agreed-on signaling and seating strategies. Communication partners also said increased understanding of hearing challenges and increased capacity to be supportive, though no specific benefit related to their own journey impacted by hearing loss was mentioned.
Some participants, hesitant to describe personal progress when asked directly, revealed significant progress when speaking freely about the time since the workshop. The interviewer was then able to reflect and reinforce positive change, enabling participants to acknowledge their own achievements.
Post pandemic inspiration: Development and trial of an online workshop
Advances in virtual learning accelerated by pandemic-related reduction of in-person human contact have propelled the profession of audiology to incorporate teleaudiology services. Workshops offered remotely could make attendance more feasible by eliminating travel time, expense, and risk, reducing delivery costs, and avoiding current in-person precautions, including masks and distancing. However, virtual meetings present challenges for people with hearing loss full participation. The viability of this modality for group aural rehabilitation was investigated by developing a new online version of workshop 1 and testing it with a total of 12 invited participants affected by a wide range of hearing loss severity. Participants were asked to notice and report on caption accuracy, transitions between screen-shared slides and face-to-face discussion, and effectiveness of communication guidelines and strategies. Connection instructions and a pre-workshop trial connection were offered. Ratings on The Line exercise were shared via private chat. Informal input from each participant was received within 2 days of the session attended.
Benefits reported included the opportunity to share experiences with people from diverse and widespread communities and increased awareness of accessibility rights and technology options. An example of research done in this province to improve speech understanding in challenging environments18 was particularly appreciated: it seemed to validate a shared experience of communication challenges in community settings, exacerbated by but not exclusive to hearing loss.
Some participants encountered minor difficulty connecting and using features such as chat and mute. However, when combined with observance of communication ground rules (turn-taking, clear speech), participants who depend on visual input for understanding found the auto-captions satisfactory. Participants stated they would attend more online workshops and recommend this session to others. In addition to increased feasibility for participant attendance, the online version is highly cost-effective to deliver, eliminating the need to hire a CART transcriber for accessibility and greatly reducing the time and person-power required to organize, set up, and deliver the workshop.
Conclusions and Future Directions
Benefits and Feasibility
This project met goals to realize the benefits of a person-centered approach to group aural rehabilitation and assess factors important to feasibility and uptake by clinicians (Figure 3).
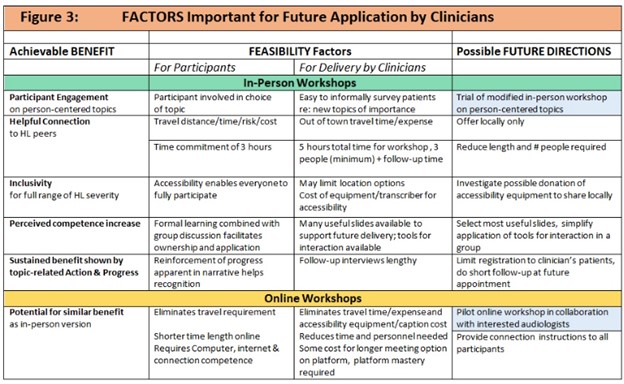
The perceived high importance of all topics and gains in perceived competence and demonstrated self-efficacy suggests these workshops could provide significant benefit in either in-person or online form. The in-person workshops involved several factors which challenge the feasibility of delivery but could be modified and piloted with clinicians who see an opportunity to improve client outcomes by leveraging the connection and resources a group can provide. The online workshop trial also provided a meaningful opportunity to examine the issue of accessibility and de-stigmatize hearing loss in community life and has the potential as a highly cost-effective opportunity to realize the benefits of group connection and learning. It was also noted that having all faces equally visible reinforces a person-centered approach to discussion. All participants, including presenters, are community members working together to identify challenges, share insight and expertise, and envision solutions for their respective communities.
Additional conclusions:
Opportunities to hear participant narratives during workshop discussion and in conversational follow-up interviews were meaningful to other participants and helpful investigators for interpretation of other benefit indicators. Recognizing genuine interest from the group and interviewer seemed to establish trust in the encounter and confidence to share. Though specific goals were not observed from goal-setting exercises during workshops, the discussion may have influenced subsequent positive action and improved outcomes.
Participant engagement and benefit were also achieved in the evaluation process through self-recognition of positive change on repeated administration of the line tool, SESMQ, and Telegram, and through assisted recognition of actions resulting in personal progress reflected by the follow-up interviewer.
Acknowledgements
The authors are grateful for IDA Institute funding and support and sincerely appreciate the additional assistance and encouragement assistance provided by multiple individuals and organizations, including Canadian researchers and hearing loss advocates Mary Beth Jennings, JP Gagne, Sheila Moodie, and Gael Hannan, Canadian Hard of Hearing Association (NL chapter and Exploits Valley Branch), Veronica Hutchings, ARC-NL and Grenfell Campus of Memorial University (Corner Brook), research participants and staff members Heather Brown, Ashley Baker and Debra Knight-Noble of Genomic-Based Research and Development Centre for Health, Angela Seaward and management of Central Health, Michelle Miller, Devon Huning and other staff of Maico Hearing Centre, Mihaela Botea of Western Health, Elks Club Corner Brook, Bell Aliant, multiple workshop volunteers and most essential of all, the project’s participants and their communication partners.
References
- Boothroyd A. Adult aural rehabilitation: What is it and does it work? Trends Amplificat 2007;11:63-71.
- Ferguson MM, Henshaw H, and Heffernan E. Evidence-based interventions for adult aural rehabilitation: That was then, this is now. Seminars Hear2019;40:68-84.
- Bennion AS, and Forshaw MJ. Insights from the experiences of older people living with hearing impairment in the United Kingdom: recommendations for nurse-led rehabilitation. Int J Older People Nurs 2013;8:270-278. doi:10.1111/j.1748-3743.2012.00318.x
- Hawkins DB. Effectiveness of counseling-based adult group aural rehabilitation programs: a systematic review of the evidence. Trends Amplificat 2005;16:485-493.
- Collins M, Liu C, Taylor L, Souza P, and Yueh B. Hearing aid effectiveness after aural rehabilitation: Individual versus group trial results. J Rehab Res Dev 2013;50:585-598.
- Abrams HP. The effects of intervention strategy on self-perception of hearing handicap. Ear Hear 1992;13:351.
- Genomic-Based Research and Development Centre for Health in Grand Falls-Windsor. A collaboration of Memorial University Faculty of Medicine with the Town of Grand-Falls Windsor, to serve mutual interests in scientific advancement of knowledge and knowledge translation through education and commercialization. A video explaining activities at the centre (which features this Ida Institute project at minute 4:25-6:56) can be accessed here: https://www.youtube.com/watch?v=WKXI8TBnYpM
- The Ida Institute. Person-Centered Care. Available at :https://idainstitute.com/what_we_do/
- Gagné J and Jennings M. Incorporating a client-centered approach to audiologic rehabilitation. ASHA Leader 2011;16:10-13.
- Statistics Canada. Table 17: Population estimates. 2021-09-29 Available at: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901
- Government of Newfoundland and Labrador, Public Engagement and Planning Division. Rural Lens: Assessing Regional Policy Implications 2019. Available at: https://www.gov.nl.ca/pep/
- The Ida Institute. Tools. Available at: https://idainstitute.com/tools/
- Thibodeau L. Plotting beyond the audiogram to the TELEGRAM, a new assessment tool. Hear J 2004;57(11):46-51.
- Accessibility Legislation in Canada: includes The Universal Declaration of Human Rights (1948), the Canadian Charter of Rights and Freedoms (1982), The National Building Code (2015), and the Accessible Canada Act (2019).
- University of Western Ontario. Self-Efficacy for Situational Communication Management Questionnaire (SESMQ). Available at: https://www.uwo.ca/nca/research/sesmq.html
- Bard CCE. SMART goals. Available at: https://cce.bard.edu/files/Setting-Goals.pdf.
- Doran G, Miller A, and Cunningham J. There’s a S.M.A.R.T. way to write management’s goals and objectives. Manag Rev 1981;70(11):35–36.
- Bennett RJ, Meyer CJ, Eikelboom RH, Atlas MD. Evaluating hearing aid management: Development of the Hearing Aid Skills and Knowledge Inventory (HASKI). Am J Audiol. 2018 Sep 12;27(3):333-348. doi: 10.1044/2018_AJA-18-0050
Additional Resources
- Ash, Gillian, 2020, Undergraduate Honours Thesis (unpublished; Supervisor Dr. Peter Stewart), Memorial University (Grenfell), Department of Psychology.
- Tønnesen, H. (Ed.). (2012). Engage in the Process of Change; Facts and Methods. Copenhagen, Denmark: World Health Organization.
- Choi, J. S., Kyoo, S. S., Kunhwa, K., Neman, C. L., Mamo, S. K., Lin, F. R. & Han, H. (2016). Understanding hearing loss and barriers to hearing health care among Korean Americanolder adults: A focus group study. Journal of Applied Gerontology, 1-24. doi:10.1177/0733464816663554
- Heacock R., Montano J., and Preminger J. 2019, Adult Children’s Perspectives on Their Role in Their Parent’s Hearing Healthcare Processes. J Am Acad Audiol 30:871–882 (2019). DOI: 10.3766/jaaa.17124
- Claesen, E. & Pryce, H. (2012). An exploration of the perspectives of help-seekers prescribed hearing aids. Primary Health Care Research & Development, 13, 279–284. doi:10.1017/S1463423611000570.
- Heffernan, E., Coulson, N. S., Henshaw, H., Barry, J. G., & Ferguson, M. (2016). Understanding the psychosocial experiences of adults with mild-moderate hearing loss: An application of Leventhal’s self-regulatory model. International Journal of Audiology, 55, 3-13. doi:10.3109/14992027.2015.1117663
- Jennings, M. B., Southall, K., & Gagné, J. P. (2013). Social identity management strategies used by workers with acquired hearing loss. Work, 46, 169-180. doi:10.3233/WOR-31760
- Lambert, J., Ghadry-Tavi, R., Kniff, K., Jutras, M., Siever, J., Roque, C., …Jones, C.A. (2017). Targeting functional fitness, hearing and health –related quality of life in older adults with hearing loss: Walk, Talk ‘n’ Listen, study protocol for a pilot randomized controlled trials. Trials, 18, 47. doi:10.1186/s13063-017-1792-z
- Granberg, S., Pronk, M., Swanepoel, D.W., Kramer, S.E., Hagsten, H., Hjaldalh, J., Moller, C., & Danermark, B. (2014). The ICF cores sets for hearing loss project: Functioning and disability form the patient perspective. International Journal of Audiology, 53, 777-786. doi:10.3109/1414992027.2014.938370

