Striking the Right Balance: Chronic Dizziness in the Vestibular Audiology Practice
Understanding and Diagnosing Persistent Postural Perceptual Dizziness (PPPD)
Preamble:
In this edition of “Striking the Right Balance,” Erica Zaia, MSc, RAUD, provides an overview of Persistent Postural Perceptual Dizziness (PPPD), hoping to help clinicians identify and treat this disabling vestibular disorder.
Michael Vekasi, AuD, R.Aud, Aud(C), FAAA and Erica Zaia, MSc, RAUD are coordinating the “Striking the Right Balance,” feature which will cover the latest information on ‘all things vestibular.’ If you would like to be more involved in all things vestibular, please check out and like our Facebook page by searching for “CAA National Vestibular Special Interest Group” within Facebook. You can also reach us by email at CAAvestibular@gmail.com.
The debate about what causes dizziness, vertigo, and balance disorders has been going on for centuries. In the 1870s, German physicians argued about the role of the eyes, ears, brain, and psyche in these symptoms. They described patients with fear and dread in plazas and open spaces, noting that they would be well inside their room or small spaces but would be overcome by inexplicable anxiety in a large, open space.1 Then, early in the 20th century, a dichotomy was created between a neuro-otological approach, proposed by Barany and Hallpike, and a psychological one, led by Freud and disciples. In the late 1900’s, it became clearer that there was, in fact, a relationship between these two branches in that people with neuro-otological disorders had higher rates of anxiety, and people with panic disorders were found to have higher rates of vestibular disorders. In the 1980s, groups of researchers in Germany, the US, and the UK described syndromes involving both clusters of symptoms – phobic postural vertigo, space motion discomfort, and visual vertigo. These disorders were initially described in people with vestibular disorders but were later identified in people with anxiety. Again, the field was in a conundrum trying to understand the causes of these syndromes. In the early 2000s important research showed how fear and threat negatively interfered with the balance function of normal individuals, showing that these reactions neither originated in an acute otologic issue nor a psychiatric condition. This led Jeffrey Staab to reformulate phobic postural vertigo into Chronic Subjective Dizziness. Diagnostic criteria were primarily based on physical symptoms rather than psychological. In recent years, the concept of functional disorders has been revived and applied to several areas of medicine. Functional disorders arise “from a change in the mode of action of an organ, unrelated to structural or cellular deficits”1. Functional disorders are not psychogenic or psychiatric in origin and do not reflect psychopathological abnormalities. Studies of patients diagnosed with phobic postural vertigo, space motion discomfort, visual vertigo and chronic subjective dizziness identified functional alterations in the vestibular and balance system. These findings led to the consensus on the Barany Society for the diagnostic criteria of Persistent Postural Perceptual Dizziness – PPPD
Diagnostic Criteria
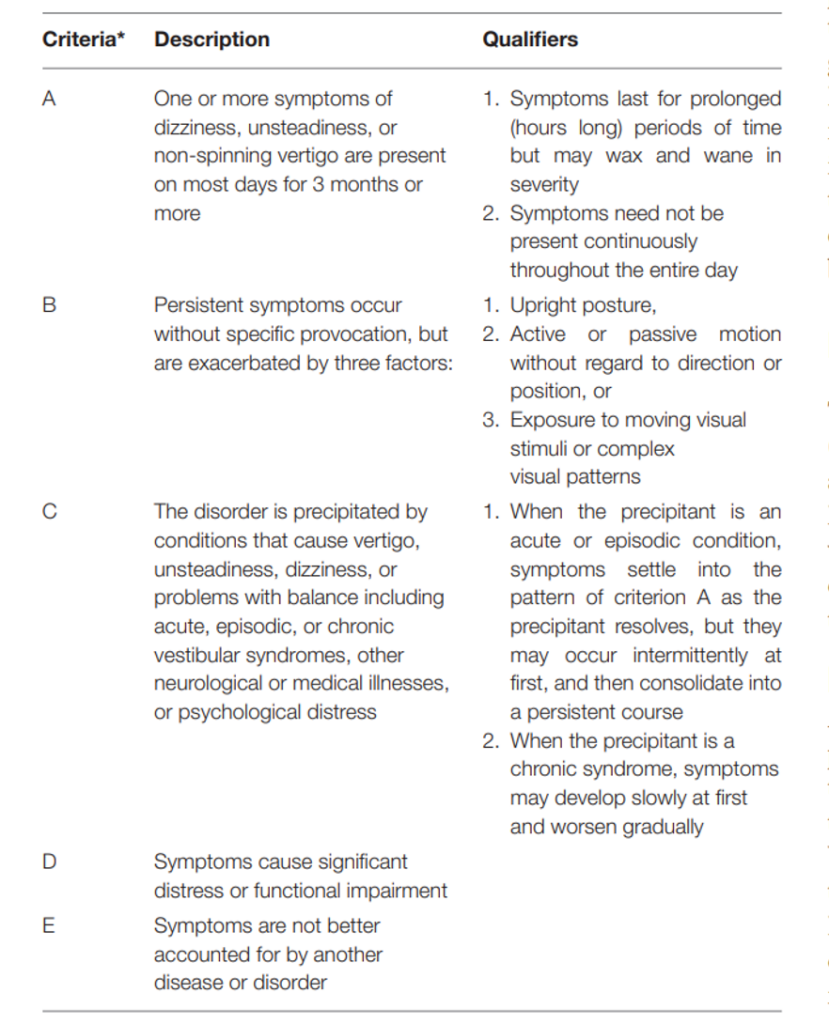
It is important to note that PPPD is not a diagnosis of exclusion and that all five conditions above must be meet for the diagnosis. Often, a traumatic event such as a panic attack or acute illness acts as a precipitant for PD. As such, underlying vestibular disorders are quite common (Table 1) and should be considered and investigated. It is, therefore, important to highlight that vestibular function testing is not always normal in PPPD – they can indeed, show signs of the primary vestibular condition.
Table 1. Frequency of Vestibular Disorders Underlying PPPD1
| Peripheral or central vestibular disorders | 25 – 30% |
| Vestibular migraine | 15 – 20% |
| Panic and anxiety attacks | 15% each |
| Concussion and whiplash | 10 – 15% |
| Autonomic disorders | 7% |
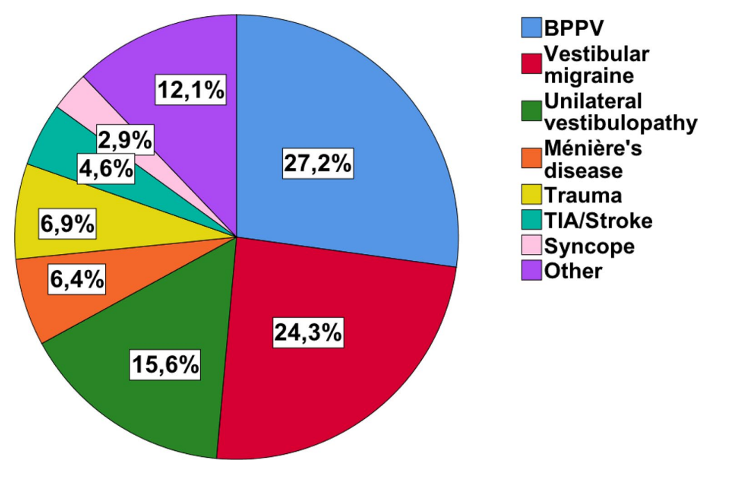
Habs and colleagues2 reported on a sample of 356 individuals diagnosed with PPPD. They examined whether the disorder was secondary to a vestibular disorder or primary, originating independently, without a previous somatic trigger. They identified that 195 patients (55%) were presented with primary PPPD, versus 162 patients (45%) for whom PPPD was secondary to a vestibular disorder. Figure 2 shows the distribution of reported vestibular disorders preceding PPPD. The authors described that in the primary PPPD group there was significantly more anxiety (20% vs. 10%) and depressive disorders (25% vs. 9%) than in the secondary PPPD group. They also noted that the individuals in the primary PPPD group were more handicapped than those in the secondary PPPD group.
From the data above, it is particularly interesting to note that a staggering 27% of the group of secondary PPPD originally presented with Benign Paroxysmal Positional Vertigo (BPPV). It certainly raises the question as to how a benign vestibular disorder, potentially easy to treat and recover from, can result in chronic symptoms of dizziness.
Trinidade and colleagues3 investigated whether certain characteristics and traits would predispose an individual to developing PPPD. Indeed, anxiety and neuroticism seemed to increase one’s chances of not fully recovering from a vestibular disorder but rather transitioning into PPPD.
They reported that people in the PPPD group had higher neuroticism, introversion, anxiety and body vigilance when compared to non-dizzy people. Neuroticism refers to relatively stable tendencies to respond to threats, frustration, or loss with negative emotions. Individuals in the PPPD group are prone to a hypervigilant state of increased introspective self-monitoring that arises from fear of further attacks of vertigo or the consequences of being dizzy. When applied to balance, these traits seem to lead to the maladaptations we will discuss later. Interestingly, only one-third of the people in the PD group believed that psychological issues were a contributing factor to their illness though. This should inform the clinician on the importance of patient education on the nature of and mechanisms leading to PPPD.
We gain significant insight into these mechanisms when understanding postural responses to threats in healthy subjects.4 When raised on a platform 10 feet above ground, healthy individuals take longer to rise to tiptoes and are even slower when on the platform's edge. Their gait speed is slower, and stride length is shorter on a high walkway these changes are even more pronounced on a narrow high walkway. The perception of lean and truncal sway was greater than the actual when high on the platform. It has also been reported that postural sway with eyes open is greater in high anxiety states. In these instances, the latency to respond to platform perturbation is shorter, and the individuals are more strongly affected by erroneous visual stimuli. In summary, fear and anxiety lead to measurable, significant changes in balance, reducing both performance and confidence.
Söhsten and colleagues5 described the posturographic profile of 20 patients with PPPD, comparing them with 15 patients fully recovered from a vestibular disorder and 15 healthy individuals. They described maladaptive stiffened postural control, high frequency of postural swaying, and co-contraction of lower leg musculature with stiffened ankle strategy in the PPPD group. In balance test conditions with eyes closed, individuals with PPPD had significantly poorer performance when compared to individuals fully recovered from a vestibular disorder. This study encourages clinicians to revisit the concept that these balance response patterns could be “non-physiological” or suggest malingering. In clinic, these clear signs on simple balance tests such as Gans Sensory Organization Performance Test are rather strong indicators of PPPD.
Another common maladaptive strategy described in PPPD is increased visual dependency for balance, leading to visually induced dizziness. This complex symptom, also sometimes named visual vertigo or visual-vestibular mismatch, is not only present in PPPD but also in other vestibular disorders such as Vestibular Migraine and Post-Concussion Syndrome. This is not a diagnosis by any means, and the patient must be educated on the physiopathological basis of visually induced dizziness. In the tripod of balance, vestibular, visual, and proprioceptive information is sent to the central nervous system. These packets of information must be processed and appropriately integrated to produce an effective harmonious motor output balance response. When the central nervous system places excessive emphasis on the visual input for balance (and not enough on the vestibular input), symptoms of visually induced dizziness arise. The individual becomes hypersensitive and symptomatic to moving or conflicting visual information. Patients describe feeling dizzy and nauseated when watching kids running around, when scanning the isles and shelves of a grocery store for a product or when driving in the rain, watching raindrops and whippers dance on the windshield.
Interestingly, fMRI studies6 showed alterations in the visual and vestibular cortical networks, with decreased functional connectivity in vestibular areas and increased functional connectivity in visual areas. Neuroimaging studies continue to reinforce the hypothesis that PPPD is not a psychological or psychiatric disorder and that there are clear “processing” issues underlying their symptoms. Indovina and colleagues7 affirm that “several cortical visuo-vestibular areas undergo anatomical and functional changes in PPPD. Decreased structural parameters are observed in the multi-modal vestibular cortex in patients with PPPD relative to controls. Functional alterations in pre-frontal and emotional regulatory areas and regions involved in visual-vestibular processing have also been repeatedly described in PPPD.”
In summary, a “perfect storm” situation is created for the individual, depicted in Figure 3.8 The white arrows show how acute vestibular insults induce necessary immediate adaptation responses of transient heightened sensitivity, which eventually subside as the individual fully recovers. Rather, in acute anxiety and body vigilance (promoting factors) the individual resorts to maladaptive balance strategies such as overreliance on visual input and stiffened postural control, leading to poor cortical integration. Chances of developing PPPD and comorbid behavioural issues are higher in individuals with neurotic temperament and pre-existing anxiety.
Understanding these processes, the treating clinician aims to break the maladaptive cycle in which PD patients are trapped. Dietrich and Staab9 list psychoeducation, cognitive behavioral therapy (CBT), medication, and vestibular and balance rehabilitation therapy as useful modalities to achieve this goal. Through psychoeducation and CBT, the individual gains awareness of the nature of PD and the role of threat assessment, fear, and anxiety-producing maladaptations that result in poor balance performance. Mindfulness and relaxation techniques are invaluable strategies in dealing with underlying anxiety.
In addition, selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs), often started at minimal dosages and titrating up if needed, have been shown helpful in treating PPPD, with positive results being consistently reported. Patients with comorbid anxiety disorders tend to have more positive response to these medications.
Several types of vestibular and balance rehabilitation exercises can be tailored to patients dealing with PPPD, aiming at specific maladaptive strategies presented.8 Relaxing and returning to normal and natural patterns of stance, postural control and gait, promoting habituation to head, eye and body movement at increased speeds, encouraging effective use of vestibular input and reducing visual dependence, decreasing fear and avoidance of movements and ultimately increasing confidence in balance, are all essential goals in the rehabilitation process, which usually lasts several months. Positive effects of vestibular and balance rehabilitation therapy have consistently been reported, including the use of virtual reality as a therapeutic modality.
Persistent Postural-Perceptual Dizziness is a prevalent, debilitating vestibular disorder, often preceded by an underlying somatic trigger, most of the time an acute vestibular episode. It is the clinician’s responsibility to properly assess and identify both PPPD and as much as possible, the underlying vestibular disorder, offering a tailored and comprehensive rehabilitation plan.
If you have patients dealing with PPPD, direct them to this patient-centered resource Persistent Postural-Perceptual Dizziness (PPPD) - Balance & Dizziness Canada (balanceanddizziness.org)
References
- Staab, J.P., et al. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Bárány Society’, Journal of vestibular research : equilibrium & orientation, 27(4), pp. 191–208, 2017.
- Habs, M., Strobl, R., Grill, E. et al. Primary or secondary chronic functional dizziness: does it make a difference? A DizzyReg study in 356 patients. J Neurol 267, 212–222 (2020).
- Trinidade, A., Harman, P., Stone, J., Staab, J.P. & Goebel, J.A. "Assessment of Potential Risk Factors for the Development of Persistent Postural-Perceptual Dizziness: A Case-Control Pilot Study", Frontiers in neurology, vol. 11, pp. 601883-601883, 2020-2021.
- Staab, J.P., Balaban, C.D. & Furman, J.M. "Threat Assessment and Locomotion: Clinical Applications of an Integrated Model of Anxiety and Postural Control", Seminars in neurology, vol. 33, no. 3, pp. 297-306, 2013
- Söhsten, E, Bittar, RSM & Staab, JP ‘Posturographic profile of patients with persistent postural-perceptual dizziness on the sensory organization test’, Journal of Vestibular Research: Equilibrium & Orientation, vol. 26, no. 3, pp. 319–326, 2016
- Van Ombergen, Angelique et al. “Altered functional brain connectivity in patients with visually induced dizziness.” NeuroImage. Clinical vol. 14 538-545. 28 Feb. 2017
- Indovina, I.; Passamonti, L.; Mucci, V.; Chiarella, G.; Lacquaniti, F.; Staab, J.P. Brain Correlates of Persistent Postural-Perceptual Dizziness: A Review of Neuroimaging Studies. J. Clin. Med. 2021, 10, 4274.
- Staab, J. Persistent Postural-Perceptual Dizziness. Semin Neurol 2020; 40(01): 130-137
- Dieterich M, Staab JP. Functional dizziness: from phobic postural vertigo and chronic subjective dizziness to persistent postural-perceptual dizziness. Curr Opin Neurol. 2017 Feb;30(1):107-113.