Age Adjustment in Audiometric Tests: Updated Results and Interpretations
Editor’s note – Dr. Gregory Flamme will be a speaker at this year’s CAA annual conference in Kelowna, British Columbia Oct. 6-9, 2024
Age adjustment is intended to represent the typical longitudinal hearing changes associated with age. In the US, age adjustments are not recommended by the National Institute for Occupational Safety and Health (NIOSH) or permitted by the Department of Defense. They are optional for workers within the scope of the US Occupational Health and Safety Administration (OSHA) (i.e., general industry) and other regulatory bodies. Uses of age adjustment include informing interpretations of threshold changes during audiometric monitoring (e.g., US 29 CFR 1910.95), group-level review of hearing conservation program effectiveness, and compensation for work-related hearing damage (e.g., WorkSafeBC, 2024; WorkplaceNL, 2019; WCB Nova Scotia, 2017). In a perfect scenario, age-adjusted data from an exposed group show the longitudinal changes in hearing thresholds that would be expected in that group if they were unexposed.
Age adjustments approximate group tendencies obtained in the past but are applied to individuals in the present. The “best” adjustments reproduce group tendencies (i.e., median trends) despite considerable errors for individuals (i.e., who fall anywhere in the 1st to 100th percentile). The accuracy of a given set of adjustments can decline as time progresses (Hoffman, Dobie, Losonczy, Themann, & Flamme, 2017, 2018). For these and other reasons, the commonly used term “correction” is inappropriate because the adjusted distributions of thresholds can never be truly correct, particularly as the group size declines toward a person.
Age adjustments are derived using cross-sectional trends, while they are intended to represent a hypothetical longitudinal change, and these are not the same. It is indisputable that a snapshot from 20-year-olds will have better average hearing sensitivity than a snapshot from a cohort of 70-year-olds. This cross-sectional trend is not derived from longitudinal measurements. The person who, at a young age, had better hearing sensitivity than 90 % of their peers at age 20 is not guaranteed to retain that relative advantage at age 70. Accidents, diseases, general health conditions, and other hazards can alter one’s standing relative to their peer group.
Conversely, absent such hazards, the person with worse hearing sensitivity than 90 % of their peers at age 20 might retain hearing sensitivity better than their peers and improve their relative standing by age 70. It is reasonable to ask, “Why, then, are cross-sectional data used for age adjustments?”. The response is equally sensible. A study with a sufficiently large and generalizable group of people with no significant health conditions or exposures, followed from childhood to old age, would be excessively complicated and costly. Suitable longitudinal datasets simply do not exist.
Cross-sectional trends overestimate typical longitudinal changes, which can be demonstrated via numeric simulation. Briefly: Assume that the hearing sensitivity of a large cohort of otologically-normal people is followed from a young age (e.g., age 5). In each 5-year interval, assume there is a small (e.g., 5%) chance of a threshold shift associated with the whole array of hazards to hearing. Over a follow-up period of decades, these hazards will worsen thresholds from affected individuals. Still, the thresholds from unaffected individuals will only change within the limits of audiometric uncertainty (see ISO 8253). Collectively, the distributions of thresholds for this cohort will flatten and grow more skewed. Changes to the distributions of thresholds will impact the percentiles in cross-sectional data while influencing longitudinal changes minimally due to the small (individual-level) chance of threshold shift. For simplicity, this simulation includes no “natural” reduction in hearing sensitivity with age. Accordingly, the simulation (Figure 1) shows no sustained longitudinal change in hearing sensitivity. On the other hand, cross-sectional trends reflect the changes to the distributions of thresholds for this cohort. Trends from lower percentiles of cross-sectional distributions better represent longitudinal changes, and this finding is consistent with the recommendations from US NIOSH to the US Federal Railroad Administration more than a decade earlier (Federal Railroad Administration, 2006).

Recent population-based estimates of cross-sectional trends in hearing sensitivity have been developed using data from the US (Flamme et al., 2020). This study utilized data from 9937 participants (ages 12 to 85+) in the 2005-2012 US National Health and Nutrition Examination Survey (NHANES) cycles. Unpublished analyses, including more recent NHANES cycles, revealed no significant differences from published values. Quantile regression curves approximating the 25th percentile revealed (expected) differences in cross-sectional trends between men and women. Differences between people who identify as Non-Hispanic Black race/ethnicity and all other self-reported race/ethnicities also led to separate age adjustment values.
Cross-sectional trends were curvilinear, indicating little or no differences at younger ages (e.g., through age 40 or 50), with increasing differences in later decades. These trends differed from the age “correction” values used in the US (OSHA Standard 1910.95 Appendix F), wherein the regulatory values assumed too much age-related change at younger ages and too little at older ages – including no additional age adjustments calculated after age 60.
Using a large longitudinal occupational hearing conservation database, the age adjustments reported by Flamme et al. (2020) matched median longitudinal changes for 9340 male New York City firefighters and emergency medical service (EMS) workers within 5 dB from 1 to 35 years of service (over 75,000 tests). A suitably sized dataset of women was not available. Firefighters and EMS workers are exposed to auditory hazards, including noise, asphyxiants, and chemical agents, thus the age adjustments reported by Flamme et al. may overestimate the contributions of age alone. The Flamme et al. (2020) age adjustments are identified and recommended in the US OSHA Technical Manual (https://www.osha.gov/otm/section-3-health-hazards/chapter-5, updated July 6, 2022) in cases where age adjustments are applied.
Some Canadian provinces have regulations that involve age adjustment. Many of these regulations involve subtraction of expected age effects for purposes including worker compensation. Adjustments are made based on average thresholds (0.5, 1, 2, 4 kHz in Quebec; 0.5, 1, 2, 3 kHz in many other provinces). The typical adjustment to the average is 0.5 dB per year, starting at 50 or 60 years of age, but the starting age can be as high as 75. The slope of 0.5 dB/year can be compared with the results of Flamme et al. (2020)(Figure 2 and Figure 3). The 0.5 dB/year slope provides a reasonable approximation of average trends for women aged 53 to 73 years but a shorter range of years for those who do not self-identify as women. For large groups, age adjustments beginning at 50 years better approximate the results reported by Flamme et al. (2020), but the curvilinear relationships show an accelerating rate of change at older ages.
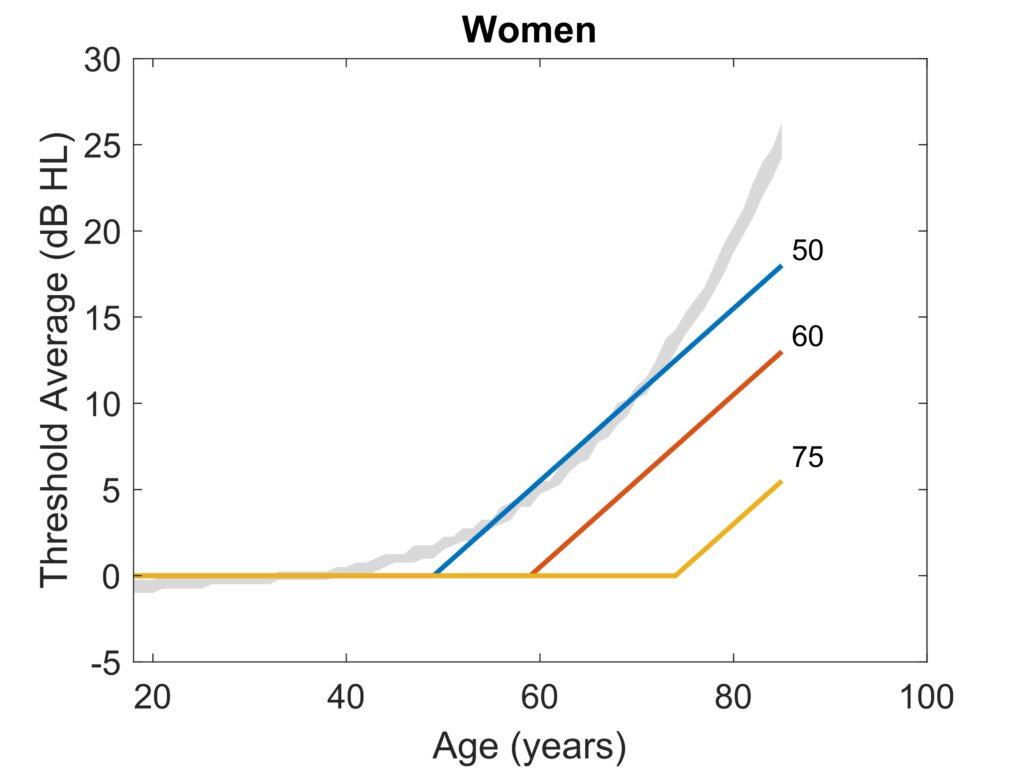
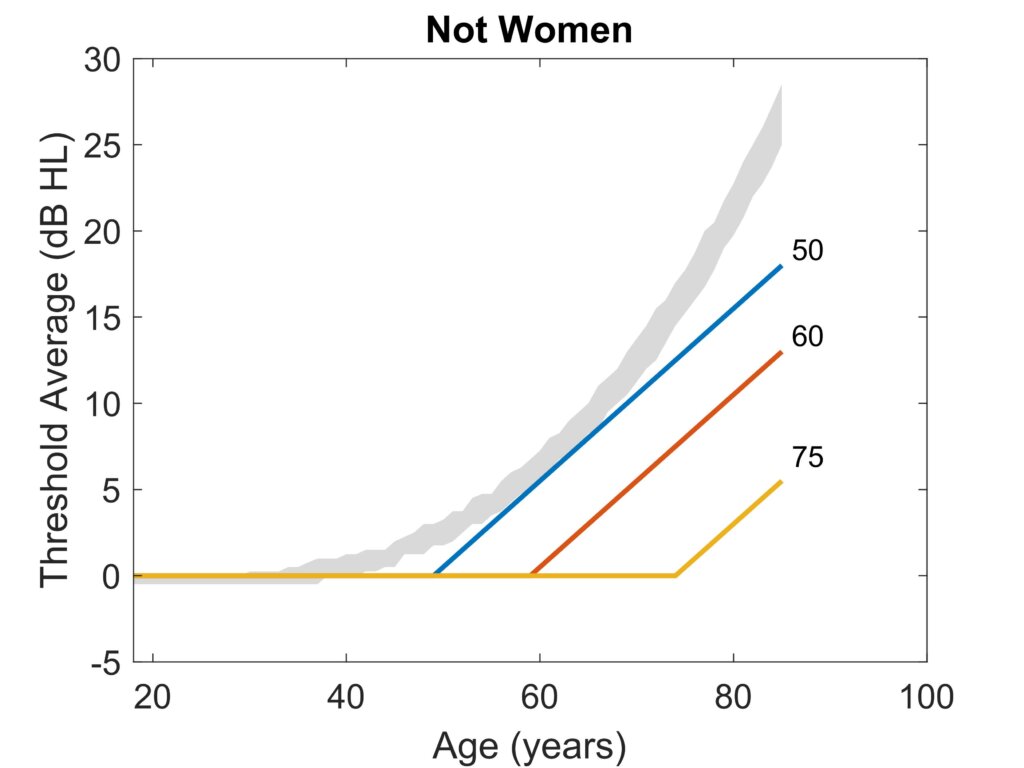
Age adjustments are often used to hypothesize the longitudinal changes that would have occurred in a large group of people if they had no hazardous exposures. In a hearing conservation program, allocating between changes due to exposure versus those that were unavoidable consequences of aging is a reasonable goal. Whether used for interpreting audiometric monitoring data or for worker compensation purposes, inaccurate estimates of age effects are problematic. In audiometric monitoring, over-adjustment for age can reduce the effectiveness of the hearing conservation program by obscuring occupationally-induced hearing changes. Under-adjustment can lead to incorrect attributions of hearing changes to occupational exposures without effect. It is incumbent on the hearing conservation program to err on the side of protecting workers (Canadian Centre for Occupational Health and Safety, https://www.ccohs.ca/oshanswers/phys_agents/noise/hearing_conservation.html, last accessed April 9, 2024), so under-adjustment for age is the better error to make, particularly as group sizes approach the individual level. In the context of compensation for occupational hearing impairment, the same concerns apply but are amplified because they are used for individuals, and except for improved hearing with increasing age, it is impossible to ascertain what a person’s hearing sensitivity would have been if not for their occupational exposures. So, despite the closer match of the Flamme et al., 2020 results to adjustments starting at age 50 (Figure 2 and Figure 3), it might be wiser to use age adjustments beginning at age 60 or greater to ensure that workers are not systematically disadvantaged. We must emphasize that the Flamme et al., 2020 results were valid for workers exposed to risk factors for hearing loss and, therefore, may still include some effects of those exposures. Until a large longitudinal population-based dataset is identified, the size of the exposure component cannot be known. However, it is clear from the results of Flamme et al. (2020) that age adjustments based on mean or median cross-sectional datasets overestimate age effects significantly, which disadvantages hearing conservation programs and workers alike.
Turning to clinical practice, it is reasonable to expect that clinical populations (e.g., individuals seeking audiometric care for hearing difficulty) would often have worse hearing sensitivity or show greater rates of longitudinal change than found in Flamme et al. (2020). Comprehensive history and diagnostic testing (including physician evaluations) should be used to rule out previously undetected exposures or systemic disease/conditions before assuming the atypical results are due to aging. Accurate estimates of unavoidable age effects can improve hearing outcomes and better hearing healthcare.
References
- Federal Railroad Administration. (2006). Occupational Noise Exposure for Railroad Operating Employees, 49CFR, part 227. In (Vol. 71 FR 63065). Washington, DC: Code of Federal Regulations.
- Flamme, G. A., Deiters, K. K., Stephenson, M. R., Themann, C. L., Murphy, W. J., Byrne, D. C., Cone, J. E. (2020). Population-based age adjustment tables for use in occupational hearing conservation programs. Int J Audiol, 59(sup1), S20-s30. doi:10.1080/14992027.2019.1698068
- Hoffman, H. J., Dobie, R. A., Losonczy, K. G., Themann, C. L., & Flamme, G. A. (2017). Declining Prevalence of Hearing Loss in US Adults Aged 20 to 69 Years. JAMA Otolaryngol Head Neck Surg, 143(3), 274-285. doi:10.1001/jamaoto.2016.3527
- Hoffman, H. J., Dobie, R. A., Losonczy, K. G., Themann, C. L., & Flamme, G. A. (2018). Kids Nowadays Hear Better Than We Did: Declining Prevalence of Hearing Loss in US Youth, 1966-2010. Laryngoscope. doi:10.1002/lary.27419
- ISO. (2010). Acoustics -- Audiometric test methods. In Part 1: Pure-tone air and bone conduction audiometry (ISO 8253-1:2010).
- Occupational Safety and Health Administration (OSHA). (1983). Occupational Noise Exposure; Hearing Conservation Amendment (29 CFR 1910). (29 CFR 1910). Washington, DC: Federal Register Retrieved from https://www.osha.gov/sites/default/files/laws-regs/federalregister/1983-03-08.pdf.
- Workers’ Compensation Board of Nova Scotia. (2018). WCB Nova Scotia Policy Manual. Nova Scotia.
- WorkplaceNL. (2019). Client Services Policy Manual: Hearing Loss, Entitlement. (EN-12). Newfoundland & Labrador. Retrieved from https://workplacenl.ca/site/uploads/2023/09/EN-12-Hearing-Loss-2019-06-18.pdf.
- WorkSafeBC. (2024). Rehabilitation Services & Claims Manual Volume II. Province of British Columbia. . Current Rehabilitation Services and Claims Manual, Volume II | WorkSafeBC. Retrieved from https://www.worksafebc.com/en/resources/law-policy/rehabilitation-services-and-claims-manual-volume-ii/rehabilitation-services-and-claims-manual-volume-ii/rehabilitation-services-and-claims-manual-volume-ii?lang=en

