Loneliness is Not an Age-Related Problem that Audiologists Can Solve Alone
What’s New About Getting Older?
Kathy Pichora-Fuller's column “What’s new about getting older?” delves into all aspects of ageing and hearing ranging from health policy developments to neurophysical research on the aging auditory brain.
“I think I would’ve retreated into a shell and just said let the world go by, I don’t care. Like I’m not making any effort and I don’t care. Because, like I say, people don’t seem to understand and I thought, well, then that means you are alone, so that’s it.
And I always remember this blind fellow coming into the shop, just before I quit work, and he said to me, ‘You know I feel sorry for you’.
And I thought, come on, you’re blind and you’re feeling sorry for me!
But he said ‘It – it’s a world of communication, especially now’; and he said ‘it’s getting more so all the time. Communicate, communicate, communicate’. And he said ‘And you can’t communicate’. So, he said ‘That means you’re isolated’.And he said to me, ‘It’s like I would visualize it as being in a closet with the door closed’.
Interview with an older adult man who is hard of hearing (Dillon Edgett, 2002)
And I said, ‘Well, it’s not quite that bad but it’s – I sometimes tell people it’s like being in a phone booth with glass walls all around”.
And I said ‘You have a family reunion, but you are in this glass booth. And you can see everybody. You can see their mouths going, but you have no idea what they’re saying.
So, without communication, you’re alone, even in a crowd.”
The words of this older adult living with hearing loss will not surprise most audiologists. We strive to improve how well our clients can communicate. Communication enables the exchange of information that is necessary in many situations. But, perhaps more importantly, communication enables social relationships. Positive social relationships can have widespread health benefits. In promoting healthy aging, could audiologists do more to overcome the social isolation and loneliness of those living with hearing loss?
Could Social Isolation Due To Hearing Loss Cause Cognitive Decline?
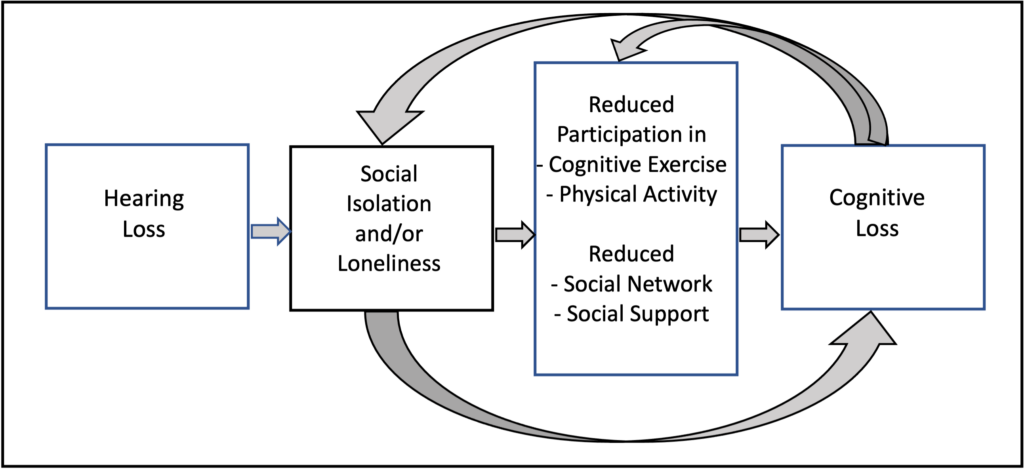
Many epidemiological studies have shown a significant association between hearing loss and cognitive decline in older adults; nevertheless, it remains unknown whether a causal basis might explain the association (Pichora-Fuller, 2023). Social isolation, the cumulative result of increasing social withdrawal, is one of the most readily understandable proposed mechanisms that might explain why hearing loss is associated with cognitive decline (Whitson et al., 2018). This possible mechanism fits with the general notion of ‘use it or lose it’. It is plausible that hearing loss results in communication difficulties and that communication difficulties may result in withdrawal from participation in social activities, ultimately resulting in social isolation. In turn, social withdrawal may reduce cognitive stimulation such that eventually, a person’s cognitive abilities may decline because they are not being used enough; for example, withdrawal from social activities such as attending lectures or committee meetings may reduce how much or how often people have opportunities to exercise their thinking and memory abilities. However, social withdrawal may also manifest in less physical activity (e.g., no longer playing team sports or joining fitness classes); in turn, physical inactivity could increase the risk of dementia (Hopper et al., 2024) and physical inactivity could also be harmful to other health conditions (e.g., diabetes) that are known to be common risk factors for both hearing loss and dementia. Furthermore, social withdrawal (e.g., going to fewer parties, belonging to fewer clubs, seeing friends or relatives less often) could result in a shrinking social network and less availability of social support; in turn, less social support could compromise how people cope with health conditions or stress (Holt-Lunstad et al., 2010), possibly increasing the risk for mental health issues (e.g., depression) that have also been associated with dementia (Brewster et al., 2021). Overall, social withdrawal may explain the association between hearing loss and cognitive decline, but the explanation is far from simple. Social withdrawal may involve many other factors related to physical and mental health that are also associated with both hearing loss and cognitive decline. To add further complication, with or without hearing loss, increased social isolation and loneliness could be caused by cognitive decline insofar as those with reduced cognitive abilities may experience reductions in their participation in cognitive and physical activities, the size of their social network, and the availability of social support. These complex possible interconnections are depicted in Figure 1. Not surprisingly, simple models testing the possibility that social isolation explains the association between hearing loss and dementia have not been convincing (Dhanda et al., 2024).
Distinguishing Between Loneliness and Social Isolation
The World Health Organization (WHO) recognizes both social isolation and loneliness as being among the most important social determinants influencing health: “The effect of social isolation and loneliness on mortality is comparable to that of other well-established risk factors such as smoking, obesity, and physical inactivity.” (https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/social-isolation-and-loneliness). However, it is important to distinguish between social isolation and loneliness. According to the WHO (2021), “Social isolation and loneliness are distinct but related concepts. ‘Loneliness’ is the painful subjective feeling – or ‘social pain’ – that results from a discrepancy between desired and actual social connections (Cacioppo et al., 2014; Perlman et al., 1981, Prohaska et al., 2020). ‘Social isolation’ is the objective state of having a small network of kin and non-kin relationships and thus few or infrequent interactions with others. Some studies have found only a weak correlation between social isolation and loneliness (Coyle & Dugan, 2012; Steptoe et al., 2013; Tanskanen & Anttila, 2016): socially isolated people are not necessarily lonely and vice versa.” Similarly, the recently published Canadian Clinical Guidelines on Social Isolation and Loneliness in Older Adults (Canadian Coalition for Seniors’ Mental Health, 2024) also differentiate between social isolation and loneliness.
How Common Is Loneliness?
The WHO (2021) estimated that up to a third of older adults are lonely worldwide. Statistics Canada (2023) found that 1/5 Canadians over 65 reported loneliness in 2019-2020 (https://www.statcan.gc.ca/o1/en/plus/4881-look-loneliness-among-seniors). It may be useful for audiologists to be aware of some of the characteristics of older Canadians who were more likely to report being lonely:
- Age: Those 85 years of age or older were more likely to report loneliness (23%) than those between 65 and 74 years of age (19%).
- Marital status: Those who were not in a marital or common-law relationship (over 80%) were twice as likely to report being lonely compared to those who were in these types of relationships (15%).
- Income: Those in the lowest income group (25%) were much more likely to be lonely than those in the highest income group (15%).
- Community Size: Those living in cities with 1 million or more people (21%) were more likely to report being lonely than those living in small towns with 1000 people (17%).
- Barriers to Social Participation: Those who reported barriers to social participation (38%) were almost three times as likely to be lonely as those who reported no social barriers (13%).
Audiologists may encounter relatively less loneliness among clients who are relatively younger older people, have high incomes, live in small towns and are in marital or common-law relationships (i.e., individuals likely to report no social barriers). Conversely, audiologists working with people over 85 years of age with low incomes who live alone in large cities may be working with more individuals who encounter barriers to social participation and are lonely. In addition to hearing loss, other health declines and intersecting stigmas may exacerbate barriers to social involvement and loneliness. Whether loneliness and social isolation co-occur may depend on other demographic and health factors. Importantly, for some older adults, loneliness, and availability of social support may need to be addressed in rehabilitation in addition to or instead of addressing barriers to participation and social withdrawal or isolation. According to the socio-emotional selectivity theory, it seems adaptive for older adults to focus on better quality relationships with a few people rather than being concerned with the size of their social network or how many activities they pursue (Carstensen, 2021).
Does Hearing Loss Increase Social Isolation and Loneliness in Older Adults?
A systematic review found that hearing loss is associated with both social isolation and loneliness, but the association was more consistent with social isolation than loneliness (Shukla et al., 2020). It is not surprising that older people living with hearing loss may withdraw from participating in social activities and are at risk for becoming socially isolated. However, the reports often heard by audiologists are that, even when clients are not socially isolated, and they do continue to participate in social events (e.g., family parties), they feel alone. This experience of loneliness, even when participating in social activities, is reflected in the opening quote from an interview with an older man with hearing loss (Dillon Edgett, 2002). Alternatively, it is possible that older people who live solitary lives do not feel lonely (Newall & Menec, 2019). Few studies have examined the associations between hearing loss and both social isolation and loneliness. A study based on data from the Canadian Longitudinal Study of Aging examined multiple constructs: social participation, social network, social support and loneliness. The main findings were that those who self-reported hearing loss did not differ significantly from those who self-reported no hearing loss on the number of activities they participated in or the number of people in their social networks (i.e., social isolation). Still, significant differences were found between those with and without hearing loss regarding social support and loneliness (Mick et al., 2018). Of course, declines in the other WHO ICOPE (https://www.who.int/publications/i/item/WHO-FWC-ALC-19.1) key capacities (vision, mobility, cognitive, mental health, or vitality/nutrition) may combine with hearing loss to affect outcomes. Notably, on all four measures (participation in activities, social network size, availability of social support, loneliness), those with dual sensory loss had significantly poorer outcomes than those without sensory loss (Mick et al., 2018).
What Are the Implications for Audiologic Rehabilitation?
The importance of social support in rehabilitative audiology has been highlighted in research showing that social support is a better predictor of satisfaction with hearing aids than many well-known hearing-specific questionnaires (Singh et al., 2015). Furthermore, fostering social support is key in delivering family-centered hearing care (Grenness et al., 2016). Less attention has been paid to older adults with hearing loss who may not have family or friends who could provide social support, but at least one example of a social model of audiologic rehabilitation for older adults who would otherwise be socially isolated and lonely has been successfully implemented at Baycrest in Toronto for years (Reed, 2012). A scoping review found that people who are hard of hearing often report social isolation and loneliness and that, based on a small number of studies, there was encouraging evidence that hearing interventions could effectively reduce social isolation and loneliness (Bott & Saunders, 2021).
Importantly, there is an imperative for new approaches to audiological rehabilitation whereby audiologists ensure hearing accessibility as part of social prescribing for older adults with hearing loss who may be socially isolated and lonely. The older adults who are likely at greatest risk may be those who have multiple disabilities for whom an integrated, person-centered, inter-professional approach to care and healthy aging is needed.
What Is Social Prescribing?
Social prescribing is a practice that is becoming widespread as a way to promote healthy aging and counter-acting social isolation and loneliness in older adults. When a healthcare provider becomes aware that social isolation and loneliness may compromise an older adult’s health, they may provide a social prescription. Social prescribing enables healthcare providers to refer people to local, non-clinical services, including community and social services. The WHO provides training resources for health professionals to learn about how to implement and support social prescribing (https://openwho.org/courses/social-prescribing-WPRO) and there is also a Canadian Institute for Social Prescribing (https://www.socialprescribing.ca/). It seems obvious that older adults with hearing loss will require hearing accessibility to benefit from the community programs that might be prescribed. Audiologic rehabilitation should be planned to optimize the benefits intended to be realized by social prescriptions to address social isolation and loneliness. This solution is inherently collaborative and could be implemented in inter-professional primary care teams and age-friendly community initiatives and programming to promote healthy aging.
References
- Bott, A., & Saunders, G. (2021) A scoping review of studies investigating hearing loss, social isolation and/or loneliness in adults. International Journal of Audiology, 60(sup2), 30-46.
https://doi.org/10.1080/14992027.2021.1915506 - Brewster, K. K., Hu, M.-C., Zilcha-Mano, S., Stein, A., Brown, P. J., Wall, M. M., Roose, S. P., Golub, J. S., & Rutherford, B. R. (2021). Age-related hearing loss, late-life depression, and risk for incident dementia in older adults, The Journals of Gerontology: Series A, 76(5), 827–834, https://doi.org/10.1093/gerona/glaa242.
- Cacioppo, J. T., Cacioppo, S., & Boomsma, D. I. (2014). Evolutionary mechanisms for loneliness. Cognition and Emotion, 28(1), 3–21. https://doi.org/10.1080/02699931.2013.837379.
- Canadian Coalition for Seniors’ Mental Health (2024). Canadian Clinical Guidelines on Social Isolation and Loneliness in Older Adults. https://ccsmh.ca/areas-of-focus/social-isolation-and-loneliness/clinical-guidelines/
- Carstensen L. L. (2021). Socioemotional Selectivity Theory: The role of perceived endings in human motivation. The Gerontologist, 61(8), 1188–1196. https://doi.org/10.1093/geront/gnab116.
- Coyle, C. E., & Dugan, E. (2012). Social isolation, loneliness and health among older adults. Journal of Aging and Health, 24(8), 1346-1363. https://doi.org/10.1177/0898264312460275.
- Dhanda, N., Hall, A., & Martin, J. (2024). Does social isolation mediate the association between hearing loss and cognition in adults? A systematic review and meta-analysis of longitudinal studies. Frontiers in Public Health, 12, 1347794. https://doi.org/10.3389/fpubh.2024.1347794.
- Dillon Edgett, L. (2002). Help-seeking for advance rehabilitation by adults with hearing loss: An ecological model. PhD Dissertation, University of British Columbia. https://open.library.ubc.ca/collections/ubctheses/831/items/1.0090827
- Grenness, C., Meyer, C., Scarinci, N., Ekberg, K., & Hickson, L. (2016). The International Classification of Functioning, Disability and Health as a framework for providing patient- and family-centered audiological care for older adults and their significant others. Seminars in hearing, 37(3), 187–199. https://doi.org/10.1055/s-0036-1584411
- Hämäläinen, A., Phillips, N., Wittich, W., Pichora-Fuller, M. K., & Mick, P. T. (2019). Sensory-cognitive associations are only weakly mediated by social factors in the Canadian Longitudinal Study of Aging. Scientific Reports, 9(1), 19660. https://doi.org/10.1038/s41598-019-55696-5
- Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316.
- Hopper, S., Wister, A. V., Cosco, T. D., & Best, J. R. (2024). Social isolation, physical activity, and subsequent changes in cognition among middle- and older-aged adults: Results from the Canadian Longitudinal Study on Aging. Psychosomatic Medicine, 86(2), 107–115. https://doi.org/10.1097/PSY.0000000000001271
- Mick, P., Parfyonov, M., Wittich, W., Phillips, N., Guthrie, D., & Kathleen Pichora-Fuller, M. (2018). Associations between sensory loss and social networks, participation, support, and loneliness: Analysis of the Canadian Longitudinal Study on Aging. Canadian family physician Medecin de famille canadien, 64(1), e33–e41.
- Newall, N. E. G., & Menec, V. H. (2019). Loneliness and social isolation of older adults: Why it is important to examine these social aspects together. Journal of Social and Personal Relationships, 36(3), 925-939. https://doi.org/10.1177/0265407517749045
- Perlman, D., & Peplau, L. A. (1981). Toward a social psychology of loneliness. In: Gilmour, R., & Duck, S., editors. Personal relationships (pp 31-56). London: Academic Press. https://peplau.psych.ucla.edu/wp-content/uploads/sites/141/2017/07/Perlman-Peplau-81.pdf
- Pichora-Fuller, M. K. (2023). Is hearing loss in older adults predictive of later development of dementia and does hearing care modify dementia risk? Canadian Audiologist, January, 2023. https://canadianaudiologist.ca/issue/volume-10-issue-1-2023/is-hearing-loss-in-older-adults-predictive-of-later-development-of-dementia-and-does-hearing-care-modify-dementia-risk/
- Prohaska, T., Burholt, V., Burns, A., Golden, J., Hawkley, L., Lawlor B, Leavey, G., Lubben, J., O’Sullivan, R., Perissinotto, C., van Tilburg, T., Tully, M., Victor, C., & Fried, L. (2020). Consensus statement: Loneliness in older adults, the 21st century social determinant of health? BMJ Open Public Health Communication 10:e034967 http://dx.doi.org/doi:10.1136/bmjopen-2019-034967.
- Reed, M. (2012). The hard of hearing club: A social model of hearing rehabilitation for seniors. International Journal of Integrated Care, 12(9). https://doi.org/10.5334/ijic.1106
- Shukla, A., Harper, M., Pedersen, E., Goman, A., Suen, J. J., Price, C., Applebaum, J., Hoyer, M., Lin, F. R., & Reed, N. S. (2020). Hearing loss, loneliness, and social isolation: A systematic review. Otolaryngology--Head and Neck Surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery, 162(5), 622–633. https://doi.org/10.1177/0194599820910377.
- Singh, G., Lau, S.-T., & Pichora-Fuller, M.K. (2015). Social support predicts hearing aid satisfaction. Ear and Hearing, 36(6), 664-676. https://doi.org/10.1097/AUD.0000000000000182.
- Steptoe A, Shankar A, Demakakos P, & Wardle J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings National Academy Science U S A., 110, 5797–801. http://dx.doi.org/doi:10.1073/pnas.1219686110.
- Tanskanen, J., & Anttila, T. (2016). A prospective study of social isolation, loneliness, and mortality in Finland. American Journal of Public Health, 106(11), 2042–2048. http://dx.doi.org/doi:10.2105/AJPH.2016.303431.
- Whitson, H. E., Cronin-Golomb, A., Cruickshanks, K. J., Gilmore, G. C., Owsley, C., Peelle, J. E., Recanzone, G., Sharma, A., Swenor, B., Yaffe, K., & Lin, F. R. (2018). American Geriatrics Society and National Institute on Aging Bench-to-Bedside Conference: Sensory Impairment and Cognitive Decline in Older Adults. Journal of the American Geriatrics Society, 66(11), 2052–2058. https://doi.org/10.1111/jgs.15506.
- World Health Organization. (2017). Integrated care for older people (ICOPE): guidelines on community-level interventions to manage declines in intrinsic capacity. Geneva, Switzerland. https://apps.who.int/iris/handle/10665/258981.
- World Health Organization. (2021). Social isolation and loneliness among older people: Advocacy brief. Geneva, Switzerland. https://iris.who.int/bitstream/handle/10665/343206/9789240030749-eng.pdf?sequence=1.

