Hidden Hearing Loss: Revisiting the Significance of Word Recognition Scores in Standard Audiometric Evaluations
Editor’s Note: Many recent reports have failed to find what the media has colloquially referred to as “hidden hearing loss” and some reports note that while this may occur in lower mammals, it does not occur in humans. Howver, a recent publication by Grant et al., Predicting neural deficits in sensorineural hearing loss from word recognition scores. Scientific reports. (2022) has reignited our interest in “hidden hearing loss.” We caught up with one of the authors of this report, Dr. Stephane Maison, for both a summary of this important research, as well as a more general Question and Answer section that immediately follows the reference section of this summary.
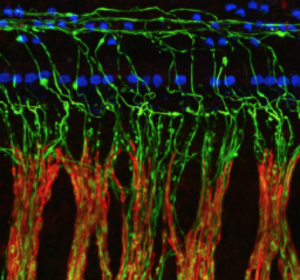
For the past decade, a large number of studies from animal models and human temporal bones on aging have shown that outer hair cell loss can be preceded by cochlear nerve degeneration (CND), whereby auditory-nerve fibers (ANFs) are disconnected from inner hair cells (for review, see.1 Remarkably, the most sensitive ANFs to aging have high thresholds and low-spontaneous discharge rates. Consequently, the loss of their unique synaptic connections with inner hair cells does not affect hearing thresholds until it becomes extreme (>80% loss), including when measured behaviorally on the audiogram. Therefore: (1) CND can be present in patients even if audiometric thresholds are within normal limits, and (2) CND is likely to be extensive in the presence of hearing loss.
Due to this insensitivity of the audiogram to CND, this phenomenon has been coined hidden hearing loss; a poor choice of words considering that the loss of these synaptic connections leads to poorer auditory processing, which may translate into a variety of quite apparent perceptual abnormalities, including one very familiar to all audiologists and widely reported by patients (with or without hearing loss): speech intelligibility difficulties in noisy environments.2–6 CND may also be key to the genesis of other perceptual anomalies associated with sensorineural hearing loss (SNHL), including hyperacusis and tinnitus.7–13
Thus, the gold standard for hearing evaluations in adults that includes a pure-tone audiogram combined with a suprathreshold word-recognition task in quiet is inadequate to fully assess CND’s hearing impairments. Bearing this in mind, we chose to revisit the significance of traditional audiometric data in a retrospective study recently published in Scientific Reports,14 testing the hypothesis that deficits in word recognition may underlie CND.
To do so, we compared the measured word scores obtained at PBmax from nearly 48,000 patients to the word scores each patient should obtain as predicted by the Speech Intelligibility Curve (SIC) associated with their audiogram. The SIC is a speech performance/intensity function derived from hearing thresholds combined with a transfer function appropriate to the speech material. In other words, this sigmoidal curve describes the predicted word score a patient should obtain as a function of the speech presentation level.15 Since the speech material is presented at suprathreshold levels (optimally at PBmax), word recognition performance is unrelated to speech audibility. Therefore, differences between measured and predicted word recognition score (WRS) reflect deficits in speech intelligibility that may arise from CND.
Unsurprisingly, WRS deficits were minimal in a cohort of patients with conductive hearing loss. Indeed, the SIC assumes hearing loss filters out speech sounds (as expected with a conductive component). However, in the same cohort, a lack of large WRS among the oldest patients suggested that cognitive decline was not a major contributor to speech intelligibility deficits assessed in traditional hearing evaluations.
On the other hand, WRS deficits increased significantly with age and degree of hearing loss in patients with presbycusis. Moreover, these deficits in speech intelligibility were even greater in SNHL etiologies known or suspected to cause greater nerve loss than age-related hearing loss, including in patients with Ménière’s disease, patients with vestibular schwannoma, and patients after sudden sensorineural hearing loss. Altogether, these results were consistent with the idea that CND significantly contributes to the loss of speech intelligibility in SNHL.
We then compared our data of speech intelligibility deficits from different SNHL etiologies with the existing histopathological data on CND in human temporal bones from donors with presbycusis only and donors with vestibular schwannomas16 and Ménière’s disease.17 As a result, we could estimate the relationship between word score as assessed in standard hearing evaluations and CND. CND must exceed 60% before word scores start to fall below 90%. Past the 60% CND mark, word scores drop rapidly with neural loss.
This predictive model of CND based on word scores could be a lot more sensitive and informative if future hearing evaluation protocols incorporate more challenging listening tasks (e.g., speech in noise; time-compressed words with reverberation). In addition, defining biomarkers of CND is key if audiologists want to identify candidates for and track the efficacy of emerging treatments meant to provide better speech intelligibility to both non-traditional hearing aid candidates and hearing aid users.
References
- Liberman MC, Kujawa SG. Cochlear synaptopathy in acquired sensorineural hearing loss: Manifestations and mechanisms. Hear Res. 2017;349:138-47. Epub 2017/01/15. doi: 10.1016/j.heares.2017.01.003. PubMed PMID: 28087419; PubMed Central PMCID: PMCPMC5438769.
- Costalupes JA, Young ED, Gibson DJ. Effects of continuous noise backgrounds on rate response of auditory nerve fibers in cat. J Neurophysiol. 1984;51(6):1326-44. Epub 1984/06/01. PubMed PMID: 6737033.
- Felder E, Schrott-Fischer A. Quantitative evaluation of myelinated nerve fibres and hair cells in cochleae of humans with age-related high-tone hearing loss. Hear Res. 1995;91(1-2):19-32. PubMed PMID: 8647720.
- Monaghan JJM, Garcia-Lazaro JA, McAlpine D, Schaette R. Hidden Hearing Loss Impacts the Neural Representation of Speech in Background Noise. Current biology : CB. 2020. Epub 2020/10/10. doi: 10.1016/j.cub.2020.09.046. PubMed PMID: 33035490.
- Wu PZ, O’’Malley JT, de Gruttola V, Liberman MC. Primary Neural Degeneration in Noise-Exposed Human Cochleas: Correlationswith Outer Hair Cell Loss and Word-Discrimination Scores. J Neurosci. 2021;41(20):4439-47.
- Resnik J, Polley DB. Cochlear neural degeneration disrupts hearing in background noise by increasing auditory cortex internal noise. Neuron. 2021;109(6):984-96 e4. Epub 2021/02/10. doi: 10.1016/j.neuron.2021.01.015. PubMed PMID: 33561398; PubMed Central PMCID: PMCPMC7979519.
- Buran BN, McMillan GP, Keshishzadeh S, Verhulst S, Bramhall NF. Predicting synapse counts in living humans by combining computational models with auditory physiology. J Acoust Soc Am. 2022;151(1):561. Epub 2022/02/03. doi: 10.1121/10.0009238. PubMed PMID: 35105019; PubMed Central PMCID: PMCPMC8800592.
- Bramhall NF, McMillan GP, Gallun FJ, Konrad-Martin D. Auditory brainstem response demonstrates that reduced peripheral auditory input is associated with self-report of tinnitus. J Acoust Soc Am. 2019;146(5):3849. Epub 2019/12/05. doi: 10.1121/1.5132708. PubMed PMID: 31795660.
- Wojtczak M, Beim JA, Oxenham AJ. Weak Middle-Ear-Muscle Reflex in Humans with Noise-Induced Tinnitus and Normal Hearing May Reflect Cochlear Synaptopathy. eNeuro. 2017;4(6). Epub 2017/11/29. doi: 10.1523/ENEURO.0363-17.2017. PubMed PMID: 29181442; PubMed Central PMCID: PMCPMC5702873.
- Hickox AE, Liberman MC. Is noise-induced cochlear neuropathy key to the generation of hyperacusis or tinnitus? J Neurophysiol. 2014;111(3):552-64. doi: 10.1152/jn.00184.2013. PubMed PMID: 24198321; PubMed Central PMCID: PMC3921399.
- Schaette R, McAlpine D. Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. J Neurosci. 2011;31(38):13452-7. Epub 2011/09/24. doi: 10.1523/JNEUROSCI.2156-11.2011. PubMed PMID: 21940438; PubMed Central PMCID: PMCPMC6623281.
- Lewis RM, Jahn KN, Parthasarathy A, Goedicke WB, Polley DB. Audiometric Predictors of Bothersome Tinnitus in a Large Clinical Cohort of Adults With Sensorineural Hearing Loss. Otol Neurotol. 2020;41(4):e414-e21. Epub 2020/03/17. doi: 10.1097/MAO.0000000000002568. PubMed PMID: 32176119; PubMed Central PMCID: PMCPMC7366362.
- Bakay WMH, Anderson LA, Garcia-Lazaro JA, McAlpine D, Schaette R. Hidden hearing loss selectively impairs neural adaptation to loud sound environments. Nat Commun. 2018;9(1):4298. Epub 2018/10/18. doi: 10.1038/s41467-018-06777-y. PubMed PMID: 30327471; PubMed Central PMCID: PMCPMC6191434.
- Grant KJ, Parthasarathy A, Vasilkov V, Caswell-Midwinter B, Freitas ME, de Gruttola V, et al. Predicting neural deficits in sensorineural hearing loss from word recognition scores. Scientific reports. 2022;12(1):8929. Epub 2022/06/24. doi: 10.1038/s41598-022-13023-5. PubMed PMID: 35739134.
- Boothroyd A. The performance/intensity function: an underused resource. Ear and hearing. 2008;29(4):479-91. Epub 2008/05/13. doi: 10.1097/AUD.0b013e318174f067. PubMed PMID: 18469711.
- Eggink MC, Frijns JMH, Sagers JE, O’’Malley JT, Liberman MC, Stankovic K. Human vestibular schwannoma reduces density of auditory nerve fibers in the osseous spiral lamina. Hearing Research. 2022;in press.
- Nadol JB, Jr., Thornton AR. Ultrastructural findings in a case of Meniere’s disease. Ann Otol Rhinol Laryngol. 1987;96(4):449-54. Epub 1987/07/01. doi: 10.1177/000348948709600420. PubMed PMID: 3619291.
Q&A
- The study suggests that cochlear nerve degeneration strongly drives discrepancies between predicted and measured speech scores. This implies that we could use discrepancies between predicted and measured speech scores to estimate cochlear nerve degeneration. However, speech measures can be quite variable with single listeners in the clinic versus 96 000 listeners in a large study (especially when using short word lists). Do you think there is a place for using discrepancies between predicted and measured speech scores to estimate cochlear nerve damage in a clinical setting?
Word recognition scores should be based on a list of 50 words. Again, though, the issue here is that word scores are typically measured in quiet. In other words, the test itself may not engage much in the high-threshold/low-spontaneous rate fibers suspected to be lost with cochlear nerve degeneration (CND). To gain more information about CND, we ought to reconsider the way we test patients and include, for example, speech testing in noise. If CND preferentially affects high-threshold fibers, speech-in-noise tests should provide a much clearer relationship between word recognition and CND. - Your data show that low-frequency hearing tended to decline more rapidly in older female than male listeners. Do you have any ideas as to why this may be?
Indeed, past the age of 65, females had more hearing loss at low frequencies. As discussed in our paper, low-frequency hearing loss in older women has been associated with vascular disease and may be related to the degeneration of the stria vascularis, which is worse in apical cochlear regions in aging humans. - It is fascinating that the data do not show any evidence for a relationship between cochlear nerve damage and reported acoustic over-exposure, except for people with thresholds in the severe range. On the other hand, the data do show evidence of cochlear nerve degeneration for people with 4 kHz notches in the audiogram.
- Is reported noise exposure simply too unreliable to help estimate the effects of noise?
Indeed. It was essential to show these results because many studies searching for CND rely on self-reported noise exposure questionnaires to define participants' groups. These questionnaires are meant to estimate the amount of noise participants have been exposed to throughout their lifetime. These questionnaires are unreliable and contribute to the discrepancies observed across studies. I can’t remember what I had for lunch 3 days ago. Can you? Can you really recall the duration, spectrum and level of your noise exposure over the course of your lifetime? When collecting the answers of our participants we had construction workers stating that they were very careful with their hearing as they played music to cover the noise of their jackhammer! Looking for a 4-kHz notch is not optimal but it at least relies on an objective yet circumstantial landmark of noise overexposure. I particularly appreciate this question because it also shows the reader that they must be careful with data interpretation. Not seeing an effect does mean it’s not there. Perhaps the method used to assess an effect is not appropriate. Question! Always question what you’re reading! - Is it safe to assume that humans with noise-induced synaptopathy will likely have thresholds shifts as well (unlike animals in laboratory studies with carefully titrated noise exposures)?
It is possible but I can’t answer this question until we have a reliable way to quantify the lifetime noise dose in humans.
- What clinical measures would you suggest for estimating synaptopathy or cochlear nerve degeneration?
A combination of speech testing that engages the high-threshold fibers of the nerve (e.g., speech in noise), combined with a measure of neural deficits (e.g., electrocochleography) and a measure of thresholds (to quantify the neural deficit that is/is not associated with a loss of outer hair cells).
- Is reported noise exposure simply too unreliable to help estimate the effects of noise?
- For listeners scoring 99% and above, the mean audiogram was roughly 15 dB to 2 kHz, sloping to 25 at 4 kHz and 35 dB at 8 kHz. Do you think this merits a reconsideration of the range that we consider to be normal hearing?
“Normal” just defines a range of hearing sensitivity. A person with hearing thresholds at -10 dB HL across test frequencies will have a different speech perception compared to a person with 20 dB HL across the board. Yet, they’re both within the same “normal” range. Hearing thresholds pretty much reflect the “status” of outer hair cells. You can have massive loss of auditory neurons and still have normal thresholds if outer hair cells are not compromised. What we ought to reconsider is making statements in the line of “your hearing is normal” based on audiometric thresholds as it can be misleading. Hearing is so much more than audibility! Many patients with a primary complaint of communication difficulties in noisy environments have “normal” thresholds. Audiometric thresholds reflect hearing sensitivity. They are not meant to measure intelligibility deficits. - Many research articles are now questioning whether “hidden hearing loss” actually exists in humans, despite evidence of its existence in lower mammals. Do you think that this study firmly establishes this phenomenon in humans?
This study, like any other conducted with living humans, can only infer, but not demonstrate, an association between CND and speech-in-noise difficulties. As mentioned earlier, I encourage the reader to question what they read. Absence of evidence is not evidence of absence. Are the results based on subjective metrics of noise exposure? Were the neural responses specific and large enough to account for the variability in the word scores? Was the filter used for electrophysiology wide enough to allow for a good visualization of the peripheral responses? Was cognition considered? Were extended high frequency thresholds recorded?
It’s indisputable that “hidden hearing loss” exists considering the number of patients reporting hearing difficulties despite having a “normal” audiogram. It is also indisputable that CND has been evidenced in human temporal bones. It’s actually the only way, to date, to provide direct evidence of CND in humans. What is questionable is whether CND plays a part in “hidden hearing loss”.