Striking the Right Balance — To Normalize or Not to Normalize? That is the Question!
Vestibular evoked myogenic potentials (VEMP) are now a common evaluation method in audiology to assess otolithic function. This test comprises the cervical and the ocular vestibular evoked myogenic potential (cVEMP and oVEMP). The oVEMP assess the utricular function by measuring the evoked potentials at the level of the inferior oblique muscle (under the eye) contralateral to the stimulated ear. The cVEMP assess the saccular function by measuring the evoked potentials at the level of the sternocleidomastoid (SCM) muscle ipsilateral to the stimulated ear. Both the cVEMP and the oVEMP are of great interest in the evaluation of different vestibular pathologies such as semicircular canal dehiscence, Ménière’s disease, and vestibular neuritis.1–3
One particularity of the cVEMP is the correlation between EMG contraction level and cVEMP amplitude. Indeed, it is known from healthy participants that the greater the SCM contraction level, the greater the cVEMP amplitude. This is because the stimulation of the saccule induces a reduction in the background EMG activity at the level of the ipsilateral SCM. To be able to measure this reduction in EMG activity, a sufficient contraction level is needed before stimulation. However, the greater the contraction, the greater the difference between EMG background activity and the induced inhibition will be, thus creating a larger cVEMP response.
Therefore, the relationship between EMG activity and cVEMP amplitude could lead to an increase in the variability of the results and could potentially mislead the interpretation of the results. For example, it is known that a significant asymmetry in contraction level can produce a clinically significant amplitude asymmetry in normal healthy participants. To overcome this problem two options are available: (1) EMG contraction monitoring or (2) normalization.
- EMG contraction level monitoring aims at recording cVEMP response when EMG reaches a given pre-determined contraction level. EMG monitoring can be done using a simple blood pressure cuff or using an EMG monitor associated with visual feedback usually built-in in your VEMP equipment. The blood pressure cuff requires the individual to be tested to push their chin against the cuff to reach a certain level of pressure and maintain this contraction for the entire recording. On the other hand, an EMG monitor associated with a visual feedback system allows the individual to adjust the contraction level to be within a given range of EMG activity in real-time, during the recording. Usually, VEMP systems with EMG monitoring can be set up to reject responses that are not within the chosen EMG range.
- A second possibility is to normalize the cVEMP amplitude using pre-stimulus EMG activity. This method uses an algorithm that allows normalizing the cVEMP response by dividing its amplitude by the pre-stimulus EMG activity. This function averages the absolute value of the pre-stimulus EMG (20 ms before stimulus onset) and divides each one of the data points (response amplitude) by this value. This method of normalization is based on the fact that a linear relationship exists between the EMG contraction level and the cVEMP amplitude response,4 which can be described by: y= ax+b (where y: cVEMP amplitude; a: slope of the regression; b: constant). The concept of linearity between EMG activity and cVEMP amplitude is crucial for normalization. However, cVEMP linearity remains a matter of debate in normal healthy individuals as some authors suggest a linear relationship5–7 while others suggest a non-linear relationship at lower and higher EMG level.8–10 To better demonstrate this concept, we replicated the graph found in Rosengren et al.10 using preliminary data acquired by our group in normal healthy participants (Figure 1). Panel A, on the left, demonstrates the correlation between EMG level measured before stimulation and the evoked (non-rectified) cVEMP amplitude. Panel B, on the right, shows the correlation between amplitude ratio (non-rectified amplitude/ EMG activity before stimulation) and EMG level. Panel A also shows the formulae that estimate the linear correlation between these variables for each participant. These results are similar to those reported by Rosengren et al. (2015),10 where the constant (b) is always negative, indicating a possible overestimation of EMG activity. This would be a result of the surface electrode capturing EMG activity not only from SCM but other surrounding muscles. This seems to underestimate the cVEMP amplitude for lower contraction levels, as demonstrated in panel B - data points with lower contraction levels are under the dashed line. The graph shows that for some individuals the amplitude ratio is a good estimator of the slope (dashed line) across most EMG contraction levels. For these individuals, therefore, normalization would be appropriate. On the other hand, the amplitude ratio was not a good estimate of the slope in two other participants (blue and yellow). Finally, panel B demonstrates that at the highest level of EMG contraction, the amplitude ratio decreased for most participants suggesting a saturation effect. This saturation effect may potentially explain the results of a study conducted by our group investigating the test-retest reliability of cVEMP amplitude in normal healthy participants.11 We compared VEMPs obtained in normal healthy participants at two different sessions. We concluded that to minimize test-retest variability it was best to monitor EMG activity and to normalize the amplitude. This allows keeping EMG activity within an acceptable range, increasing the chances to have a linear relationship and making the normalization process more efficient.
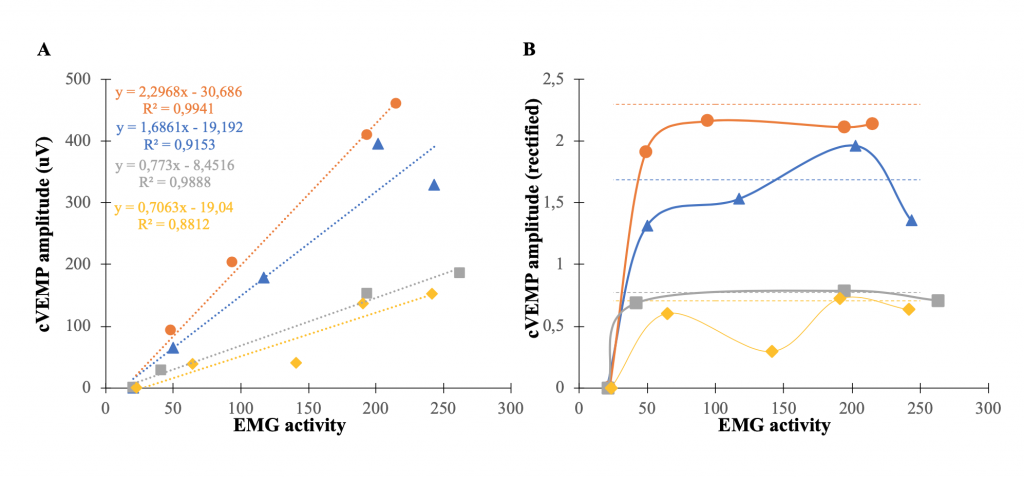
Figure 1. (A) Representation of the correlation between EMG activity and unrectified cVEMP amplitude. Dashed lines represent linear regression between EMG activity and unrectified cVEMP amplitude for each participant. Each participant is represented by a different color. (B) Normalized cVEMP amplitude (unrectified cVEMP amplitude/background EMG activity) with the different EMG activity levels. If rectified cVEMP amplitude is appropriate (linear correlation) each point should be close to the dashed line.
Having considered all these factors, one major piece of information is still lacking in the literature. All of the previous research cited in this article studied normal healthy participants. To date, it is unknown whether common vestibular pathologies (i.e., Ménière's disease, vestibular migraine, semicircular canal dehiscence) affect the linearity. One could hypothesize that the linearity could be affected in different ways by certain vestibular disorders and have a significant influence on the interpretation of the results, but this remains to be determined.
But the question still stands: to normalize or not to normalize? In other words, as a clinician evaluating individuals with various possible vestibular disorders, as opposed to only studying normal healthy individuals, what should you do? Based on the data described in this article and until further research is completed, the interpretation of cVEMP normalized amplitude is not recommended as a rule. Indeed, as we do not have a complete understanding of the concept of linearity in healthy controls and, most importantly, how the various vestibular disorders commonly encountered in the clinic may affect this crucial concept of normalization, such manipulation of the data is not the best option. However, one strong recommendation is to control for the level of EMG activation to reduce misinterpretation of asymmetry ratio and to ensure better test-retest variability. This could be performed as discussed earlier, either by using a blood pressure cuff or built-in EMG monitors. This essential step in testing allows for better comparisons between healthy and affected individuals and within individuals (test-retest reliability). Interestingly, McCaslin et al’s findings supported that the use of an optimal activation technique, having the individual lay in a semi-recumbent position, with the head elevated and turned away from the stimulated ear, is sufficient to maximize cVEMP amplitude and to reduce variability in subjects of all ages.12 Additionally, the authors suggested that the use of visual target (to elicit a specific degree of contraction) and/or normalization did not significantly reduce variability. However, these authors noted that normalization should be used specifically in people who received a suboptimal procedure to elicit cVEMP response.
The use of cVEMPs in audiology clinics is of great interest in the identification of several vestibular disorders. However, great attention to the methodology used is needed as several factors may affect the results. Among others, the EMG activity before stimulation needs to be controlled to ensure proper interpretation. Until further research is done and if EMG is carefully controlled, using optimal activation method as described by McCaslin et al., or by direct EMG monitoring, there should be no need for normalization.12
References
- Murofushi T. Clinical application of vestibular evoked myogenic potential (VEMP). Auris Nasus Larynx 2016;43(4): 367–76. doi: 10.1016/j.anl.2015.12.006.
- Maheu M, Alvarado-Umanzor JM, Delcenserie A, and Champoux F. The clinical utility of vestibular-evoked myogenic potentials in the diagnosis of Ménière’s disease. Frontier Neurol 2017;8:415. doi: 10.3389/fneur.2017.00415.
- Rosengren SM,Colebatch JG, Young AS, et al. Vestibular evoked myogenic potentials in practice: Methods, pitfalls and clinical applications. Clin Neurophysiol Pract 2019;4:47–68. doi: 10.1016/j.cnp.2019.01.005.
- Noij KS, Hermann BS, Rauch SD, and Guinan JJ Jr. Toward optimizing vestibular evoked myogenic potentials: normalization reduces the need for strong neck muscle contraction. Audiol Neuro-otol 2017;22(4-5):282–91. doi: 10.1159/000485022.
- Akin FW, Murmane OD, Panus PC, et al. The influence of voluntary tonic EMG level on the vestibular-evoked myogenic potential. J Rehabil Res Develop 2004;41(3B):473–80.
- 7. Isaacson B, Murphy E, Cohen H. Does the method of sternocleidomastoid muscle activation affect the vestibular evoked myogenic potential response? J Vestib Res 2006;16 (4-5):187–91.
- Bogle JM, Zapala DA, Criter R, Burkard R. The effect of muscle contraction level on the cervical vestibular evoked myogenic potential (cVEMP): usefulness of amplitude normalization. J Am Acad Audiol 2013;24(2):77–88. doi: 10.3766/jaaa.24.2.2.
- McCaslin DL, Fowler A, Jacobson GP. Amplitude normalization reduces cervical vestibular evoked myogenic potential (cVEMP) amplitude asymmetries in normal subjects: proof of concept. J Am Acad Audiol 2014;25(3):268–77. doi: 10.3766/jaaa.25.3.6.
- Rosengren SM. Effects of muscle contraction on cervical vestibular evoked myogenic potentials in normal subjects. Clin Neurophysiol 2015;126(11):2198–206. doi: 10.1016/j.clinph.2014.12.027
- Bethani L, Maheu M, Delcenserie A, et al. State-of-the-art assessment allows for improved vestibular evoked myogenic potential test-retest reliability. Audiol Res 2018;8(2):212. doi: 10.4081/audiores.2018.212.
- McCaslin DL, Jacobson GP, Hatton K, et al. The effects of amplitude normalization and EMG targets on cVEMP interaural amplitude asymmetry. Ear Hear 2013;34(4):482–90. doi: 10.1097/AUD.0b013e31827ad792.

