Feasibility of Using Tele-Audiology in the Canadian Marketplace as An Alternative To Live Appointments for Follow-Up Services
As audiologists, we are unavoidably immersed in a field that merges technology and healthcare. In recent years household names such as Uber, Netflix and Airbnb have used technology focused on connectivity to disrupt their respective industries and challenge traditional business models.1 As such, we too must be prepared to embrace new technology focused on connectivity that may be applied to healthcare, such as tele-audiology, as this has the potential to enhance the delivery of care to patients and alter our current business structure.
The World Health Organization’s declaration of a global pandemic surrounding the novel coronavirus, COVID-19, in March 2020 sparked renewed interest in tele-audiology. Clinicians have been forced to balance the health and safety of their patients, social isolation and distancing, and the competing needs of caring for patients while needing to limit traditional face-to-face interactions.
Prior to this event, the use of telecommunication in health care has shown continuous annual growth in response to an evolving societal landscape and advancements in telecommunication technology. Wide application of technology focused on connectivity in health care has led to the terminology “telehealth”, meaning health care at a distance.2 The use of telehealth technologies has grown rapidly in recent years due in large part to the widespread availability of internet access supporting these services. Telehealth has proven beneficial in bridging the gap between patients and health care providers, thereby overcoming economic and geographical barriers as well as supplementing face-to-face services.3 The United States Department of Veterans Affairs have been an early pioneer of tele-audiology in our industry and have demonstrated the potential effectiveness of assessment and treatment using telehealth technology.4
Estimates that close to 80% of those with hearing loss do not have access to hearing health care has been a major argument in favour of adopting tele-audiology in our field.5 Access to audiology services in developed countries such as the United States and Australia has also been called into question and this may be of special interest to the Canadian marketplace when we consider our low population density and numerous rural and remote communities.6 However, the majority of the Canadian population lives in urban centers which risks leading some clinicians to the conclusion that tele-audiology is not relevant to their urban practices. Conversely, evidence suggests that access can also be difficult in urban areas and tele-audiology has the potential to improve efficiency in the health care system regardless of rural or urban inhabitance.7,8
Professional bodies such as the College of Audiologists and Speech Language Pathologists of Ontario (CASLPO) have updated the scope of practice guidelines for audiology to include tele-audiology as an alternative method of service delivery when it is in the patient’s best interest. In fact, CASLPO indicates that some electronic forms of delivering care may fall under the same definition as a “face-to-face” encounter.9
Furthermore, a growing body of evidence has demonstrated that numerous audiological services delivered remotely have been found to be feasible and as efficient as services provided face-to-face.10 With careful implementation, tele-audiology therefore has the potential to facilitate patient centered-care and enhance current practices. As such, this study aimed to better understand the feasibility of implementing tele-audiology services to adult patients in an urban Canadian private practice setting as an alternative to certain traditional live appointments. It also sought to capture quantitative and qualitative data on patient interest in those services, as well as potential barriers to implementation.
Methodology
Eight clinicians, each at a unique urban clinic, who reported motivation to use tele-audiology in their regular audiology practice were selected to participate in this pilot study. They were trained using the commercially available “Remote Support” option found in Phonak Audeo Marvel hearing aids and Phonak Target software. This feature enables clinicians to make adjustments to hearing aid settings remotely from their office computer in real time while the patient is connected to the internet elsewhere. Simultaneously, a live real time video conference is established with the patient using streaming technology linking the users hearing aids and a smartphone to the clinician’s computer. The clinicians were instructed to offer each patient fit with a Phonak Marvel hearing aid their routine post fitting recheck appointment via tele-audiology using these Remote Support features rather than the traditional live appointment. Clinicians were asked to document the frequency of actual recommendations for tele-audiology, acceptance and completion of recheck via tele-audiology, and any qualitative data relevant to the patient’s or clinician’s decision-making process in an excel template (Appendix A). Qualitative data was coded and counted in order to arrange in meaningful groups. The clinicians collected data for 6 months and were given reminders at 1 month and 3 months post training. This study took place in 2019.
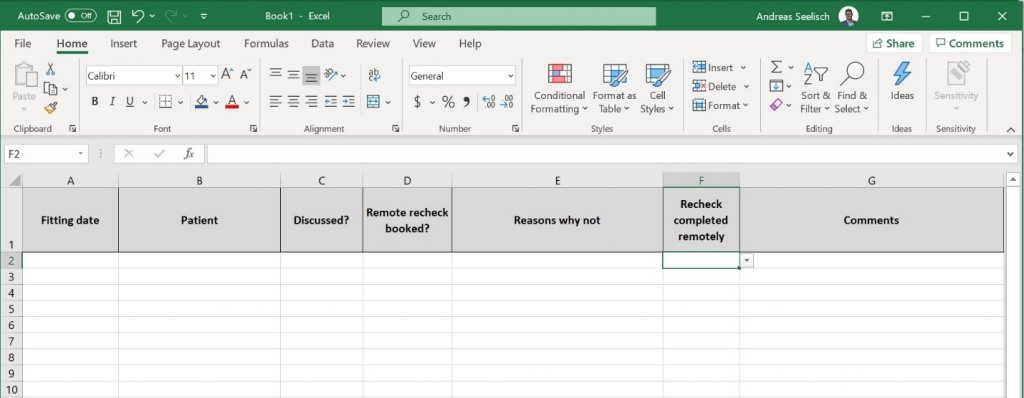
Appendix A. Template used for data collection.
Results
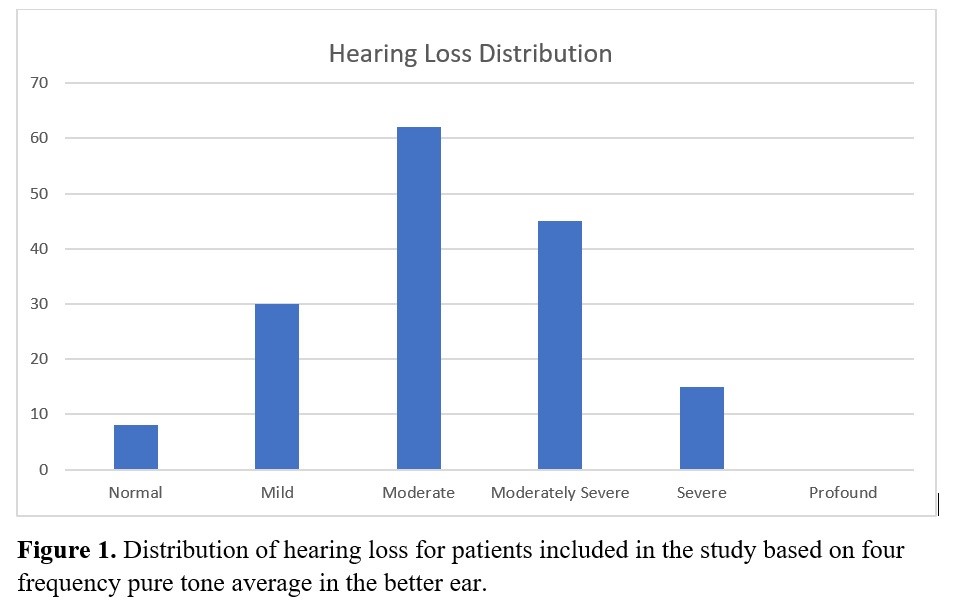
A total of 206 patients (112 men and 94 women) between the ages of 21 and 97 (mean = 72; median=74) were fit with Phonak Marvel hearing aids during a span of six months. Patients demonstrated a wide distribution of hearing losses consistent with a typical practice and illustrated by Figure 1.
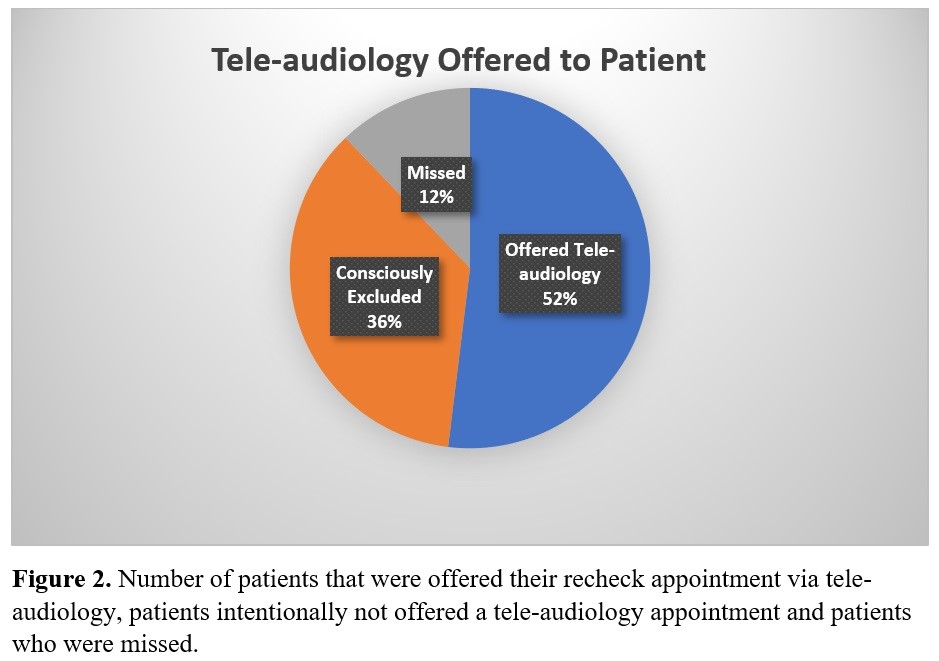
Data were compiled into an excel template that captured patient demographics, fitting date, whether tele-audiology was discussed, whether a tele-audiology recheck appointment was booked, whether a tele-audiology appointment was completed (and reasons why not), and any open format comments the clinician felt were relevant. Of the 206 patients included in this study, 107 patients (52%) were offered the recheck appointment remotely. Despite being instructed to offer tele-audiology to every patient fit with an eligible device, 99 patients were never offered tele-audiology by the treating clinician and were therefore excluded. The majority of these patients were consciously excluded for a reason deemed appropriate by the clinician (such as limited English, not being “tech savy”, or not having the required smartphone and internet access (n=74; 75%). The remaining 25 were not offered the service due to reasons such as “forgot”, “ran out of time” or in some instances a reason was not indicated (25%).
Of the 107 patients offered a tele-audiology recheck appointment, only 7 patients (7%) accepted the remote appointment. Thirty individuals (28%) did not have the necessary smartphones. Twenty-five (23%) dropped out due to implementation problems (e.g., “email request expired,” “waiting for download,” “email sent” etc.) and importantly, in these cases, the process to set up the tele-audiology appointment was not completed prior to the follow-up appointment. Thirty-two (30%) indicated that they were not interested or preferred the option of a live appointment for the recheck. Tele-audiology recheck appointments were successfully completed in only 2 cases (29%) with the reasons for drop out including: needing to see the clinician live prior to the scheduled tele-audiology appointment (n=2;29%), technical issues (n=1; 14%), services not being available in home country (n=1; 14%) and simply changing their mind (n=1; 14%.)
Discussion
At first glance, these results appear to draw the conclusion that tele-audiology is not feasible given the total number of people accepting or completing appointments using “remote support.” However, there remains a great deal to be learned from this data. Past research has shown that acceptance by clinicians is a key factor in determining success with telemedicine interventions.14 Despite clinicians initially indicating that they were interested in tele-audiology, nearly half of all subjects were not even offered the service, highlighting a major barrier to its use. In our study, 25 patients were deprived of the opportunity to even indicate their willingness to participate due to limited time or a failure to consider tele-audiology as an option for particular patients given the novelty of the service. In considering the 74 patients whom clinicians decided were not good candidates for tele-audiology, the reasons provided for not offering the service (e.g., “not into technology”) frequently involved assumptions about patients without discussion of these assumptions with the patient (n=6; 8%.) This paternalistic approach is certainly at odds with our current focus on patient centered care. While some of these assumptions may hold true, for example for the large number of patients who did not have a phone or email address, patients may have chosen to overcome these barriers by enlisting the support of a significant other to complete the tele-audiology appointment if offered.
In a recent survey of audiologists, Eikelboom and Swanepoel found that even though positive attitudes towards telehealth and associated technologies were common, only 15.6% had utilized tele-audiology in their routine clinical practice.11 As was the case in our study, all clinicians recruited had positive attitudes towards tele-audiology but actual utilization might be limited by numerous other barriers and as clinic operators, we need to uncover those barriers if we desire higher levels of utilization. This is certainly a research gap which should be addressed in order to optimize the success of tele-audiology.
For instance, within our study, 2 of the 8 clinicians reported high rates of drop out (35% and 60%) specifically among patients with whom tele-audiology had been discussed. Upon further review, this was likely due to failure to complete the required steps necessary to conduct the tele-audiology appointment. Documented explanations included: “email expired”, “waiting for download” or “email sent”. This suggests flaws with implementation, and likely highlights the importance of placing the onus to facilitate the next steps on the clinician, rather than on the patient themselves. It also calls into question the manner in which the clinician counselled on this service. In contrast, more engaged clinicians reported barriers such as “phone did not have enough space to download app” which clearly indicates an active approach aimed at ensuring their patient is optimally set up for the tele-audiology appointment to be successful.
In order to buy in to this new model of care, patients will need to feel that there is confidence in the way care is delivered, and therefore, not surprisingly, if the next step was not facilitated by the clinician this would account for a high rate of drop out. This is consistent with Berg which reports that 75% of telemedicine attempts fail.12 As such, we believe that implementation is a key element to the successful utilization of tele-audiology in a private practice setting. Implementation strategies should include working with the patient at the time of fitting to arrange the “Remote Support” appointment and ensuring the appropriate tools are already in place, as opposed to passing the burden of success onto the patient. Similar processes are already used for live appointments such as arranging a firm appointment time, providing an appointment reminder and ensuring the patient has good clarity on the next step in the rehabilitative pathway. A successful tele-audiology appointment likely requires these same strategies, with added steps to ensure an optimal set-up for the tele-audiology appointment to be successful. For example, this might include ensuring the invitation email was received, downloading the app and possibly even testing it before the patient leaves. The dropout rate and associated reasons for drop out in our pilot study reinforce the belief that the clinician is the most important initial gatekeeper for success with telemedicine interventions.13
One strength of our pilot study is the qualitative data collected, as opposed to using a purely quantitative approach. For instance, this study did not predefine specific exclusion criteria for patients. Services were intended to be offered to all patients fit with the Marvel hearing aid as the only requirement necessary for participation with no specifics with regards to patients themselves. We are therefore able to better understand candidacy based on the qualitative data collected. For example, barriers due to a lack of a smart phone, cell phone and internet access/email were frequently reported. Of the 107 patients who were offered the service, 29 (27%) did not have a phone, smartphone or internet/data access and an additional patient was excluded as services were not available in their home country despite interest in tele-audiology.
Finally, reviewing the entire group of 198 patients for whom qualitative data was collected reveals an additional 55 patients who were not offered tele-audiology because they were also lacking the needed technologies. We therefore have begun to establish what proportion of the population does not have access to the necessary connective technology needed to conduct an appointment remotely (42%; n=84.)
This data also therefore also implies that more than half of patients did have access to the technology required to support a tele-audiology appointment which is not only encouraging for the future of tele-audiology but also aligns with research that shows global internet access has increased from 16% of the world population in 2005 to 47% in 2016.14 Similar data on smart phone ownership suggests 42% of the population above the age of 65 in the US owns a smart phone, and there are additional reports from countries such as the UK where 65% of those between 65 and 75 were observed to be smartphone adoptors.1
Singh et al. suggested that tele-audiology could pose a threat to patient practitioner relationship quality.15 Some of the observed qualitative findings in this pilot study are quite relevant to that concern or the potential fear of tele-audiology replacing face-to-face interactions. A large portion of those offered tele-audiology services (n=31) suggested they preferred live appointments. Reported reasons for this preference varied with examples including “lives close,” “prefers to come in” or “too complicated.” This indicates that 44% of patients with the appropriate technology to facilitate a tele-audiology appointment still prefer a live face-to-face appointment. As such, we do not believe there is a risk of completely replacing live appointments with tele-audiology but rather expect services such as Remote Support to supplement them. Our data also revealed an additional 9 patients who were excluded by the clinician from being offered a tele-audiology appointment due to barriers such as limited English or French, visual impairments, cognitive limitations, or services not being available in their home country again highlighting that tele-audiology may not be suitable for all populations and should not be considered a replacement for live appointments.
Low overall acceptance may also be explained by the narrow scope of this project in which only the initial post fitting recheck was being replaced with a tele-audiology appointment. For instance, it is noteworthy that 8 of the 32 (25%) individuals who preferred a live recheck appointment also indicated that they might be interested in the future. This was a common theme as numerous other subjects in this group as well as others reported clear interest in the near future such as a desire to set it up at the live recheck appointment (n=7) or simply indicating “later” (n=3.) There were also 2 individuals who were highly interested but excluded as the services were not available in their home country. As such, interest in tele-audiology appears to be greater than our acceptance rate would imply.
Interest in tele-audiology appeared to range from active to contemplative to disinterested. In an attempt to better understand interest, we might consider categorizing qualitative responses into groups of “Active,” “Passive” and “Disinterested” groups. The active group can be characterized by those who accepted or made plans to defer their first tele-audiology appointment to after their recheck appointment. The disinterested group would include those patients who expressed clear preference for live appointments without indicating future interest in tele-audiology. Finally, the passive group could be characterized by those who indicated they might be interested at a later time or who passively accepted the offer of tele-audiology but ultimately did not participate as the set-up process was never completed. This group would be the most heterogeneous and may include patients who were truly actively interested but encountered barriers, or alternatively who had no interest but felt inclined to accept due to the social pressure of pleasing an offering clinician. This is a general flaw with the method in which the qualitative data was collected as it is ultimately reported from the perspective of the clinician. There is a risk therefore that assumptions have been made about patients and preferences which may not be accurate.
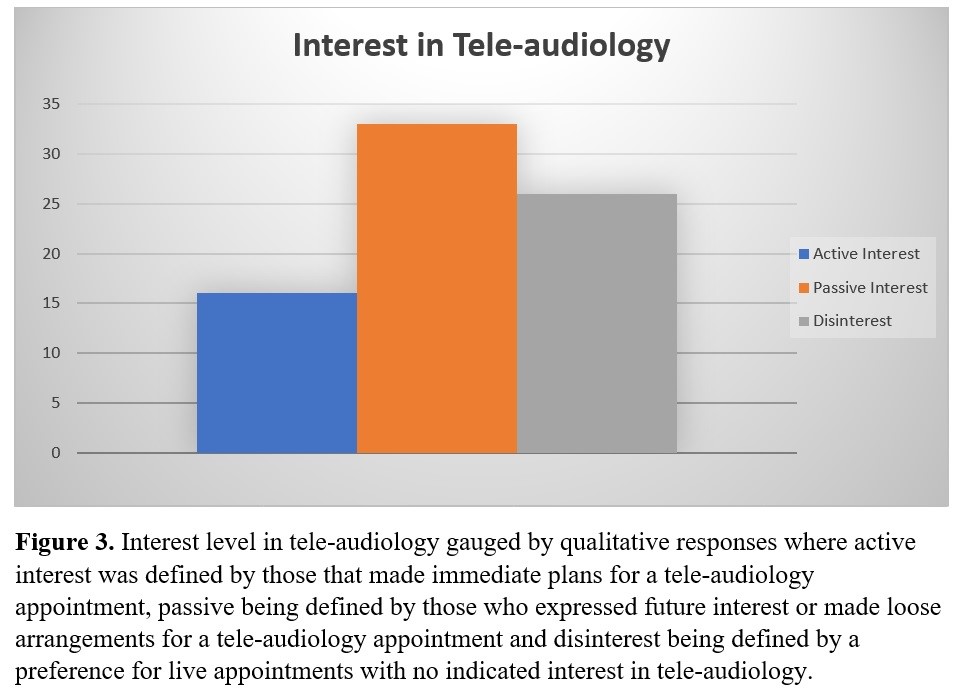
These findings support the idea that tele-audiology is relevant to typical caseloads found in urban practices as a majority of patients who had access to the technology that would have supported a tele-audiology appointment demonstrated at least some interest in it.
While the sample size was small, those who completed tele-audiology appointments reported high levels of satisfaction and a preference to use remote appointments in the future. This is consistent with Angley et al. who found that tele-audiology procedures were feasible, that participants preferred remote over face-to-face, and had a positive reaction to receiving care in this manner.10 Gladden also supports this with patient outcome data collected over several years showing satisfaction with tele-audiology as the same or better than traditional office visits.16
Our drop out data among those who chose to complete tele-audiology recheck appointments raises several other points of discussion. For instance, two individuals (29%) unexpectedly needed to see the clinician prior to the scheduled tele-audiology recheck appointment, and therefore completed their recheck in person. This reinforces the point that the need for some face-to-face appointments will persist. Further, there were an additional 3 patients who knew at the time of their initial fitting that they needed to return to the clinic at recheck for supplies such as an earmould or wax guards, and therefore ended up completing the recheck in person, rather than by tele-audiology despite their interest in using it. Similarly, there was an instance in which technical issues prevented a successful tele-audiology appointment resulting in a negative experience. This stresses the importance of seamless implementation as testing systems in advance may have resulted in more successful implementation for this individual.
Conclusion
Our study clearly shows a large portion of our patient population in urban practices have access to technology that would support tele-audiology appointments and that there is sufficient interest to warrant offering it. As such, offering tele-audiology services should be considered further as a potential part of regular clinical practice. However, in order to be successful, it is imperative that clinicians have a systematic approach to both offering tele-audiology services as well as implementing care. Further training and guidance to ensure clinicians are able to implement this with confidence is required. If successful, clinicians should not expect tele-audiology to replace live appointments but rather supplement them as has been seen in various other branches of health care.
Finally, this study was completed in the first half of 2019, prior to a radical shift in societal attitudes towards social distancing as a result of the global coronavirus pandemic. Further research is required to see what lasting impact this would have on interest in tele-audiology, voracity of recommendations by clinicians and acceptance of tele-audiology services by patients in the current societal landscape.
References
- Montano J, Angley G, Ryan-Bane C, et al. eAudiology: Shifting from theory to practice. Hear Rev 2018;25(9):20–24.
- Wootton R, Patil NG, Scott RE, and Ho K. Telehealth in the Developing World. London: Royal Society of Medicine Press Ltd; 2004.
- Fabry D. Applications of telehealth for hearing care. Audiol Today 2010;22:18–25.
- Dennis KC, Gladden C, and Noe CM. Telepractice in the Department of Veterans Affairs. Hear Rev 2012;19(10):44–50.
- Swanepoel D. 20Q: Audiology to the people – combining technology and connectivity for services by telehealth. 2013; AudiologyOnline, Article 12183.
- Swanepoel DW, and Hall JW III. A systematic review of telehealth applications in audiology. Telemed e-Health 2010;16(2):181–200.
- Nemes J. Tele-audiology, a once-futuristic concept, is growing into a worldwide reality. Hearing J 2010:63;19–24
- Swanepoel D. 20Q: Audiology to the people – combining technology and connectivity for services by telehealth. 2013; AudiologyOnline, Article 12183.
- College of Audiologists and Speech-Language Pathologists of Ontario. Use of Telepractice Approaches in Providing Services to Patients/Clients, 2–5; 2014.
- Angley GP, Schnittker JA, and Tharpe AM. Remote hearing aid support: The next frontier. J Am Acad Audiol 2017;28(10):893–900.
- Eikelboom RH and Swanepoel W. International survey of audiologists’ attitudes toward telehealth. Am J Audiol 2016; 25(3S):295–98.
- Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform 1999;55(2):87–101.
- Whitten PS and Mackert MS. Addressing telehealth's foremost barrier: provider as initial gatekeeper. Int J Technol Assess Health Care 2005;21(4):517–21.
- International Telecommunication Union (ITU). ICT facts and figures 2016. Geneva: International Telecommunication Union (ITU); 2016.
- Singh G, Pichora-Fuller MK, Malkowski M, et al. A survey of the attitudes of practitioners toward tele-audiology. Int J Audiol 2014;53:850–60
- Gladden C. 20Q: Teleaudiology - The future is now. 2018; AudiologyOnline, Article 22121.

