Other People’s Ideas
Other People's Ideas
Calvin Staples, MSc, will be selecting some of the more interesting blogs from HearingHealthMatters.org which now has almost a half a million hits each month. This blog is the most well read and best respected in the hearing health care industry and Calvin will make a regular selection of some of the best entries for his column, Other People’s Ideas.
I hope you all had a Merry Christmas and a belated Happy New Year to all! The 2015 year was an interesting year for Canadian Audiology. We saw new faces on the industry side, some old faces changing positions, a truly amazing CAA conference (the committee should be thanked over and over again), and some interesting developments south of the border. I chose to make this submission a potpourri to reflect on 2015.
Have a great 2016! Happy reading!
And Our Greatest Enemy Is…Facing Back at Us in the Mirror
Originally posted at HHTM On January 13, 2015. Reprinted with permission.
I read the 4-week Perfect Storm Series, by Jerry Northern, that ran this past fall at Hearing Views, with great interest. Ultimately, Dr. Northern’s analysis into many of the ills that plague our profession today should resonate with most audiologists–especially those in private practice.
Apathy, without a doubt, has been our greatest enemy for far too long.
Cheaper Unit Cost Alone Will Not Save Independent Audiology
Except for maybe the manufacturers, I don’t think anyone can argue against lower-priced hearing aids being a positive development and beneficial to many in private practice.[1] Like the unexpected drop in gasoline prices stimulating the national economy, this could certainly help the bottom line for many. However, is this not a temporary solution?
Do we genuinely believe that cheaper pricing alone will be the savior of independent practices and put the Big Box stores out of business?[2]
Really think about that one for a moment.
Time to Focus on the Future
It seems to me that too much of our time is spent arguing about who’s right: ASHA, AAA or ADA. As a result, people who may be in the middle wind up getting completely turned off to the process.
We plateau, rather than progress.
While political issues, such as achieving greater autonomy, are critical to the profession in the long term, I think we need to begin placing more focus on how to prepare for our future within our present reality: What do we bring to the table that is unique and less likely to be commoditized?
“…unfortunately, to the general public, there is little apparent difference between the various types of providers and their wares – so it often comes down to a comparison of costs.” –Jerry Northern, PhD
It may be a hard pill to swallow, but after all the years of opportunity to showcase the unique value that audiologists bring to the realm of hearing healthcare, the general public still doesn’t distinguish between hearing care providers.
A Future Without Hearing Aids?
Yes, the thought of a future in Audiology without hearing aids seems implausible. So many of us today live and breathe hearing aids on a day-to-day basis–it’s what we know! It’s very easy to get caught up in a world of the latest and greatest features, iPhone Apps, etc., and then promote these wonderful innovations to our patients.
The future of audiology lies in the prevention, diagnosis, management, and treatment of hearing and balance disorders; a fully-rounded healthcare profession. Audiology is not, and cannot afford to be, a one-trick pony.
It’s time we began focusing less on hearing aids in our marketing and outreach to potential patients. While hearing aids will continue to play a role in our professional lives, the future of audiology is NOT in hearing aids.
It’s easy to blame large retail chains for a litany of issues the profession is facing today. It’s much harder to look in the mirror.
It’s easy to blame large retail chains for a litany of issues the profession is facing today. It’s much harder to look in the mirror.
Just as Optometrists didn’t give up glasses and contact lenses 20 years ago when the retail chains began to seriously disrupt the status quo, we won’t give up hearing aids. They’ll still be around,[3] but basic economics will likely force us to finally get outside the traditional bundled-service hearing aid delivery model.
We’ve reached a tipping point. Overall average retail costs for hearing aids are likely going down, while wholesale prices (to independent practices) are likely to keep going up. Meanwhile, consumers are continuing not only to demand lower prices, but they are simultaneously demanding MORE services to go along with it.
If you aren’t unbundling in your clinic now, you won’t have a choice in the future–unless, perhaps, you like to work for free.
Preparing for a Brave New World
“Find the niche you can scratch!” is a piece of advice every practicing audiologist should remember. You can’t just be another hearing aid office–you must find a niche in which you can serve and excel. We need look not only to our roots, but also to our future.
Since we can’t count on hearing aids alone to sustain our practices in the future, it’s time to unequivocally own hearing loss prevention, tinnitus treatment and vestibular evaluation/management, etc.
With the advent of the AuD as the standard in Audiology, isn’t it time that we stopped being our patients’ “Hearing Aid Guy” or “Gal”? Do you call your dentist “My Tooth Guy?” or your Optometrist the “Eye Lady”? Maybe some of you do….but, my guess is no.
If we believe Audiologists are overdue in finally being recognized as Limited License Physicians(LLP),[4]we must [re]brand the profession accordingly. We must also educate accordingly: by operating under the assumption that all future AuDs will have greater autonomy and responsibility in patient care (i.e., LLP status).
ENT physicians, like hearing aid dispensers, are our colleagues, not our enemies. Our future is with them, not opposed to them. We each bring a unique skill set to the table to help our patients.
I recently spoke with a prominent ENT physician who said there is “no reason” Audiologists shouldn’t have prescriptive rights, but that our profession needs to make a few relatively small changes in our educational process so that our profession and the greater medical community are “speaking the same language.”
We should be embracing the medical community and building alliances, not burning bridges.

MicroClinic: The next evolution in hearing healthcare? Coming to a mall or pharmacy near you! Image of HealthSpot booth.
The Future Is Only Scary if We Make It So…
The future is rife with risks and potential threats to the long-term viability of audiology. However, the future also holds tremendous opportunity for positive change.
Audiologists need to begin the debate today as to what the appropriate rules should be for emerging technologies, such as tele-audiology. What can you or can’t you perform “virtually” and what services are allowed reimbursement and by whom?
If we don’t seriously consider the long-term implications of this (and other) technology, and its uses, it could easily be co-opted by larger corporate interests that may or may not be friendly to us.
Time to Put Down the Kool-Aid
 Don’t fool yourselves: Costco and the Big Box stores aren’t going anywhere.[5] They make for an easy scapegoat, but they certainly aren’t the reason audiology finds itself in its present state. It’s time to move forward.
Don’t fool yourselves: Costco and the Big Box stores aren’t going anywhere.[5] They make for an easy scapegoat, but they certainly aren’t the reason audiology finds itself in its present state. It’s time to move forward.
Lower unit price alone is not going to save audiology.
Other major players will, no doubt, join in the fray and continue to disrupt the comfortable existence we’ve been able to maintain for such a long time while other industries/professions have experienced their share of major disruptions.
As Brian Taylor pointed out back in 2012, “The Era of Low-Hanging Fruit is Over“. In 2015, I propose we stop looking back with nostalgia at how we think “it should be” and instead focus on the real issues facing us today and in the future. We have no other option but to embrace our new reality and continue to find ways we can thrive within it.
Michael Collins, AuD is an audiologist with experience in private practice and within industry working for a major hearing aid manufacturer. Dr. Collins believes that independent hearing care practitioners can and will continue to thrive in the future, but only if they shift their focus away from technology alone, and instead commit to best practices and greater personalization of the patient experience.
Footnotes
- not to mention, many patients as well!
- I don’t want to discount the efforts to unify the profession, which are truly laudable, but we need to be realistic that this is not the one and only solution to all of our ills. The issues plaguing the profession go far beyond something as simple as high-priced hearing aids
- We can certainly take some lessons from our Optometry colleagues on a number of issues, not the least of which is insurance coverage. Studies over the years have indicated a much higher likelihood to purchase hearing aids if there was at least somecoverage provided. Yet, in hearing healthcare, we often see companies droppinginsurance coverage for aids rather than adding it. It may be time audiologists rallied behind the idea that hearing aids should be included among the essential health benefitsin all 50 states
- as now even AAA explicitly supports
- As a matter of fact, one could make a very good argument that this alternate model deserves some credit for increasing hearing aid adoption among a cohort of people that would normally never consider casting their shadow within 100 feet of a traditional audiology or hearing aid clinic. Food for thought!
Postural Lightheadedness: Break It Down
Originally posted at HHTM On August 25, 2015. Reprinted with permission.
My informal estimate is that about ten percent of all patients referred to me over the years for “dizziness” are, in fact, complaining of postural lightheadedness. They have no symptoms while sitting or lying down, no symptoms while rolling over in bed, but when they get up? Watch out! The patient usually describes it as “dizzy”, but when given a forced choice between “Is it more like spinning, or more like you could faint?”, most choose the latter.
Further questioning likely reveals that the lightheaded sensation and accompanying loss of balance settles out in a minute or two. At this point, I am suspicious that they may be dealing with a temporary drop in blood pressure when they first stand up, a condition known as Orthostatic Hypotension. I have covered Orthostatic Hypotension (OH) in some detail previously.
A review of their medications and past medical history may reveal some suspected causes. OH is often caused by medications that lower blood pressure by keeping the blood vessels dilated. Another common cause is autonomic dysregulation which can be the result of diabetes. Since hypertension and diabetes are both common in the older population, is there a way to get clarity on which might be responsible? Maybe.
I say “maybe” for two reasons:
- I am not a medical doctor, my doctorate is in Audiology
- OH is very variable (meaning you may see nothing abnormal at the time of exam, yet at other times the patient may experience a significant drop in blood pressure and associated symptoms on rising).
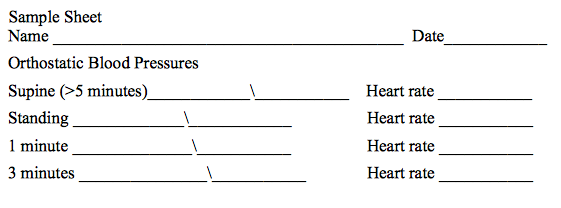
A 2011 article in the journal American Family Physician outlines various patterns associated with postural lightheadedness, and states that certain patterns can help distinguish the source of the problem. he outline below is closely excerpted from a table in this article that describes interpretation of possible responses to tilt table testing, but can give you some idea of patterns to look for. Finally, at the end of this blog is a sample of a sheet that may be used for documenting changes in blood pressure and heart rate over time.
Normal – Blood pressure maintained or increased on rising, heart rate increased by 10 -15 beats per second
Orthostatic Hypotension –decrease in systolic of 20 mmHg or more OR decrease in diastolic of 10 mmHg or more within 3 minutes of rising
Autonomic Dysfunction – Immediate decrease in both systolic and diastolic blood pressure on rising, no change in heart rate
Neurocardiogenic – Sudden decrease in Blood pressure and simultaneous decrease in heart rate on rising
POTS (Postural Orthostatic Tachycardia Syndrome) – Heart rate increases by 30 beats per second, or persists at greater than 120 beats per second on rising
ADA Supports PCAST; Offers Additional Guidance
Originally posted at HHTM On November 17, 2015. Reprinted with permission.
LEXINGTON, KENTUCKY — Following their annual meeting in Washington DC, the Academy of Doctors of Audiology (ADA) issued a position statement on the recent PCAST report.[1] In a press release, authored by recently elected ADA president Rita Chaiken, ADA supports the PCAST report because the recommendations “present significant opportunities for audiologists to reach more patients and offer additional compensated services.”
The PCAST position statement outlines ADA’s qualified support of these PCAST recommendations and also provides suggestions to encourage consumers to seek comprehensive evaluation and treatment for suspected hearing and balance disorders.

Kim Cavitt, AuD
In a detailed, 7-page letter to President Obama, out-going ADA president Kim Cavitt, addressed the importance of the delivery of evidence-based preventative, diagnostic and rehabilitative audiologic care, and how this care is instrumental to patient success with any amplification device.
The letter offers broad concurrence to all four of the PCASTs recommendations to the President, along with the following important caveats and considerations:
- Any type of over-the-counter hearing device be very specifically labeled and include a “strong recommendation that a patient seek a comprehensive audiologic evaluation from an audiologist or physician prior to purchase any device….”
- In support of the appropriate use and labeling of PSAPs, ADA advises that PSAPs be labelled with a strong recommendation that the user seek comprehensive audiologic care from an audiologist or physician prior to purchase. Further, ADA recommends that all PSAP products be labeled as “not-FDA registered devices,” and that it develops industry standards sanctioned by the American National Standards Institute (ANSI).
- The letter highlighted the PCAST finding that “64% of people with the most serious hearing loss reported that they could not afford hearing aids” and emphasized the fact PSAPs are not appropriate for many (moderate-severe to profound) of these hearing losses.
- ADA believes all programmable hearing devices sold in the US should be delivered on an open platform, so that any licensed hearing professional can adjust and program them. An open platform format, according to ADA, will result in increased patient access to care, improved buying power and improver portability of care between providers.
- In order to spur more competition in an “insular” hearing aid marketplace, ADA encourages the manufacture of more value-based alternatives offered at a price point similar to what is currently dispensed in both the VA and Big Box retail. Additionally, price should be transparent and itemized to the consumer.
- To address the barriers to hearing device adoption, Medicare Plan B must better align with current best practices in patient care and allow for more direct access to audiologists (through the Audiology Patient Choice Act– HR 2519) and greater reliance on telehealth. According to the letter from Dr. Cavitt these are the types of initiatives that will lead to greater awareness among both the public and medical professionals of the long-term deleterious effects of age-related hearing loss and the importance of early detection and remediation.
Far from Broad Consensus
In a November 12 letter to the president, which was also posted on the Healthy Hearing website[2], Paul Dybala, PhD, outlined four points that he believes PCAST “got wrong about hearing aids.” Below is a summary of his concerns contained in the letter:
- PSAPs generally contain comparatively poorer levels of sound processing technology to modern hearing aids. Thus users of these devices would be less likely to have satisfactory listening experiences due to the lower levels of technology.
- The analogy comparing PSAPs to reading glasses is flawed as most hearing loss is sensorineural, which means that the hearing organ has been damaged and/or non-functional. Therefore, the job of a hearing aid is more complex than just increasing the volume of the sounds sent to the ear.
- The labeling of OTC hearing devices (such as PSAPs) is essentially a non-issue for consumers. Most consumers purchasing PSAPs are not aware of the exact amount of hearing loss they have, so the current system of warning consumers to avoid use with severe hearing loss is somewhat meaningless.
- The vast majority of hearing care professionals already offer a copy of the hearing test results upon request to the consumer. It is standard clinical practice for professionals to provide a copy of the hearing test to the patient at no additional cost. Dr. Dybala goes to say that spending taxpayer dollars to institute legislation to enforce what is already occurring as standard practice would be a waste of time and money.

Paul Dybala, PhD
Additionally, Dr. Dybala made note of the fact that PCAST had no committee members with any extensive experience in the hearing loss or hearing aid fields from industry, clinical, research or consumer perspectives. Thus PCAST lacked any applied or scientific experience with hearing loss and treatment.
Dr. Dybala Offers PCAST the Following Four Recommendations:
- Mandate all health insurance to cover hearing aids as a preventative care measure.
- Support initiatives to promote hearing aids as a healthy choice.
- Mandate a national best practices protocol for hearing aid fittings.
- Mandate package labeling for risk of hearing loss on various consumer electronic devices
Healthy Hearing is not the only organization to oppose the PCAST recommendations to date. The International Hearing Society has also come out to strongly opposes the PCAST recommendations.
*HHTM will continue to monitor and report any press releases and position statements from other professional organizations and industry firms regarding the PCAST report.
Footnotes
- Aging America & Hearing Loss: Imperative of Improved Hearing Technologies.
- Healthy Hearing is a subsidiary of the William Demant Group
A Baker’s Dozen: School Recommendations for Families With Students Who Are Deaf or Hard of Hearing
Originally posted at HHTM On August 25, 2015. Reprinted with permission.
The typical school classroom can be a very difficult listening situation for a child with a hearing loss. Children with hearing differences must overcome three primary challenges when listening in a classroom, including: background noise, distance from the teacher and other communication/instruction sources, and reverberation. As we approach the beginning of the academic school year for many of our children, the following are some of the key recommendations that should be strongly considered for adoption into a child’s Individual Education Plan/Program (I.E.P.) in order to reduce the above-noted challenges:
- FM (Frequency-Modulation) or IR (Infra-Red) technology is a non-negotiable item for implementation. For group instruction, that includes the student with hearing loss, the teacher should be required to make use of a microphone/transmitter which should be coupled to a boom microphone or a collar microphone versus a lavaliere-type microphone (unless the lavaliere mic has been determined to be omni –directional — head movements to either side by the teacher reduces the signal-to-noise ratio/SNR due to the loss of consistent mic-to-mouth distance of approximately 6 inches). A pass-around microphone/transmitter should also be used by the student’s peers, in order that all of the students, along with the teacher, can have their voices amplified and delivered to the room’s speaker/s (or the child’s individual hearing aid/s and/or cochlear implant/s). In this way, the student will have access to the teaching and discussion of all members of the classroom.
- Acoustic ceiling tiles, and areas of soft, sound-absorbing surfaces in order to reduce reverberation (“bouncing of sound waves”) in the classroom (tennis balls on chair/desk legs-feet, use of bulletin boards, and window treatments).
- Carpeted floor in teaching space/s.
- Removal or “noise-treatment” of assorted noise sources (both internal and external noise in the classroom can be ameliorated by closing the classroom door, windows, and the treatment of heating, cooling, and other ventilation systems.
- Small class size.
- Preferential seating (however, to quote a marvelous article by Flexer, Wray, & Ireland, 1989, “Preferential Seating is NOT Enough!”). This may not automatically mean front and center of the classroom). The key is the physical placement of the child in the classroom, so that the teacher’s voice and his/her visual (speechreading) cues are best received by the student.
- Teacher/s with clear, appropriately intense (but not “Loud”), minimally accented voices/speech production skills and abilities.
- Teacher/s with an accepting attitude for teaching a child who is deaf or hard of hearing being placed in his/her classroom.
- Reasonable teaching accommodations such that visual/written cues (especially as the student becomes a “reader”) are routinely used to supplement the auditory instruction. For example, printed class schedules on the board; use of transparencies and PowerPoint; captioned videotapes/films, etc.
- Pre-teaching of schoolwork as needed/as appropriate. Parents should be provided with loaning of class textbooks and weekly materials for pre-teaching of vocabulary words and pre-teaching/review/reinforcement of upcoming schoolwork.
- Inservice as required to inform all school personnel about the student’s hearing loss, hearing aids/cochlear implants, use of other sensory technology, teaching needs, ways to facilitate communication between and among the family members, school personnel, school- and other service providers (special educators).
- Other acoustic/physical and teaching accommodations, as outlined by the student’s IEP/504 Plan team members.
Finally, #13 — families are encouraged to be in touch with their Audiologist, the school’s educational audiologist, their cochlear implant team members, and if available, “Outreach” personnel at their State’s School for the Deaf — who all can serve as valuable resources for the family and the school personnel in the implementation of reasonable accommodations for the student with hearing loss.
RESOURCES
Flexer, C., Wray, D., & Ireland, K. (1989). Preferential seating is not enough. Language, Speech, and Hearing Services in Schools, 20(1), 11-21.
Johnson, C.D., & Seaton, J. (2012). Educational audiology handbook (2nd ed.).
Clifton Park, NY: Delmar/Cengage Learning.
Mangiardi, A. (1993). A child with a hearing loss in your classroom? Don’t Panic: A guide for teachers. Washington, DC: AG Bell Association for the Deaf.
www.phonicear.com
Classroom simulations of FM/HA technology
Cochlear Implant Manufacturers
Advanced Bionics – “Tools for Schools: Helping Children with Cochlear Implants Succeed in School” ToolsforSchools@AdvancedBionics.com
Cochlear Americas – HOPE Program
MED-EL – BRIDGE to Better Communication; “Educator Packet: Resources for Education and Rehabilitation Professionals” www.medel.com
Preferred Hearing Aid?
Originally posted at HHTM On August 25, 2015. Reprinted with permission.
What Would be a Preferred Hearing Aid Performance?
Would a consumer select the same hearing aid performance as was recommended by an audiologist if given a choice among different signal processing schemes? The topic of a preferred hearing aid has been the topic of this series of posts over the last three weeks.
Results show that there is not agreement, at least for four different hearing aid algorithms (different hearing aid operating systems) as reported in this study. This post will conclude the series, providing results of consumer preference comparisons from two countries for the same study, the preferred algorithms in different listening environments, speech intelligibility in noise with their preferred algorithms, and SNR intelligibility comparisons among the provided algorithms.
Country Comparisons
Results from the past three posts were from a study conducted in the U.S. Would the results be similar to those found in the U.S. if conducted with subjects in a different country – in this case, the Netherlands? Individual algorithm preferences in the Netherlands showed the same inconsistency between the subject algorithm preferences versus those recommended by a group of audiologists. Because individual algorithm preferences in the Netherlands showed the same inconsistency between audiologists’ recommendations and subject preferences, they will not be duplicated here. Instead, a few graphs have been selected to provide additional information not measured in the U.S. study.
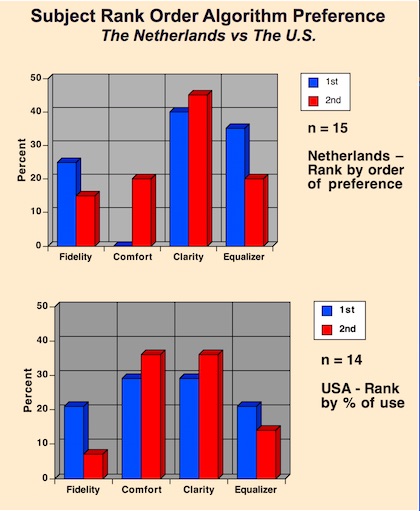
Figure 1. Signal processing algorithm rank order preference differences between subjects from The Netherlands and the United States, for the same study.
Subject algorithm preferences between the two countries for first and second rank order are shown in Figure 1. The Clarity algorithm was ranked highest for first and second choice by subjects in The Netherlands. In the U.S., the Comfort and Clarity algorithms were rank ordered the same, with both being the preferred algorithms. The Comfort algorithm showed the greatest difference between the two countries. There seems to be no logical explanation for this. In general, the results show that there appears to be little consistency in how subjects rank order the algorithms they prefer, regardless of country.
Preferred Algorithm in Different Listening Environments
Subjects were asked to rank order their algorithm preferences when listening in the following common environments in The Netherlands study: quiet, party, car, street, and music (Figure 2). The Clarity algorithm was the clear winner, ranking first or tied for first in every listening environment other than music. This was followed closely by the Equalizer algorithm.
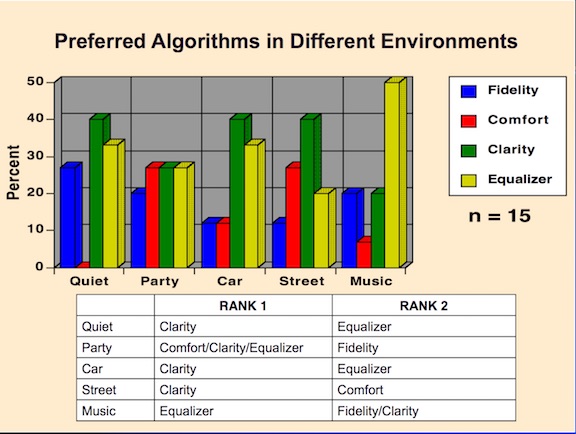
Figure 2. Subjects’ preferred algorithms (rank ordered 1 and 2) when listening in the environments identified, and when allowed to adjust between the four different algorithms used in this study.
Speech Intelligibility in Noise with Preferred Algorithm
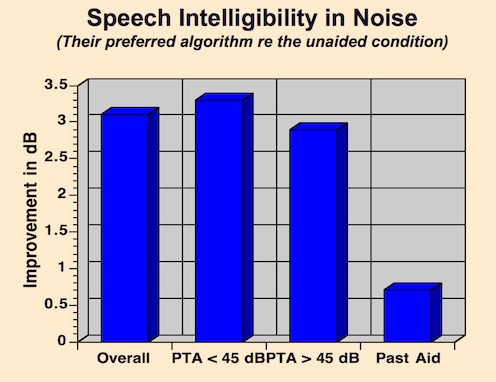
Figure 3. Speech intelligibility (SNR) when listening in noise. Each 1-dB improvement translates to a 9.6% intelligibility score increase.
The results of speech intelligibility, as expressed in signal noise ratio (SNR) when listening in noise, is shown in Figure 3 for the subjects’ preferred listening algorithm. The graph shows the overall score for all fifteen subjects, for those having a pure-tone audiogram less than 45 dB, for those having a pure-tone average greater than 45 dB, and a comparison to their past hearing aid. The algorithm subjects preferred provided improved listening in noise when compared with their current hearing aid, regardless of the hearing levels as expressed by the pure-tone average (PTA).
SNR Intelligibility Improvement by Algorithm
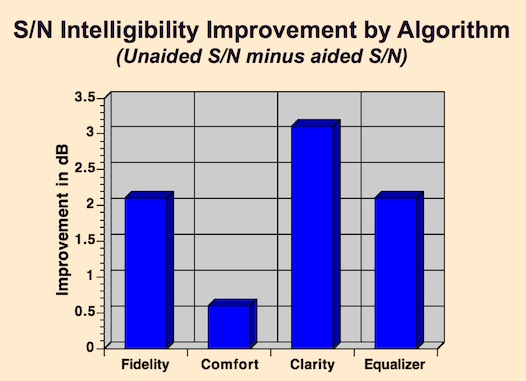
Figure 4. Average SNR (signal noise ratio) improvement for each of the algorithms when all subjects are measured on each algorithm.
Do each of the algorithms provide equal SNR improvement when compared with each other? Figure 4 showed the SNR improvement with subjects when tested across all algorithms. It shows that the Clarity algorithm provided the best SNR improvement, with the Comfort algorithm showing the least SNR improvement. So, for the algorithms under investigation, it appears that the algorithms do not provide equal SNR improvement.
Summary
Experienced hearing aid wearers were provided with an open platform system in which they were allowed to move back and forth and select between four different but common algorithms (meaning four different hearing aid operational characteristics). These algorithms, (Fidelity, Clarity, Comfort, and Equalizer) are not to be confused with selecting among different listening environments (Quiet, Noise, Music, Restaurant, etc.), which is a common feature in current hearing aids. In essence, each algorithm is essentially a different hearing aid. The study purpose was to determine if the algorithm recommended by an audiologist would be the same as what the consumer would prefer following a two-month period during which subjects wore this system (BTE hearing aid and remote algorithm selector). Results showed that there was essentially no agreement.
The investigation results provide lingering questions about hearing aid selection – what do we really know about hearing aid selection? Overall, results from this study show:
- Similar hearing thresholds are not satisfied by the same hearing aid signal processing scheme,
- Appropriate hearing aid circuitry is not as accurately predicted as one might be led to believe,
- Signal processing preferences by hearing aid users change over time,
- Patients/clients/consumers’ signal processing preferences bear little resemblance to recommendations made by audiologists,
- Patients/clients/consumers are interested in participating in their hearing aid selection.

