Striking the Right Balance – Vestibular Migraine
In this edition of “Striking the Right Balance,” Dr. Jamie M. Bogle of the Mayo Clinic Arizona highlights the current knowledge and offers important information on vestibular migraine.
Michael Vekasi, MClSc, R.Aud, Aud(C), FAAA and Erica Zaia, MSc, RAUD are coordinating the “Striking the Right Balance,” feature which will cover the latest information on ‘all things vestibular.’
If you would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by simply emailing CAAvestibular@gmail.com to let us know you want to be a part. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
Migraine is one of the most common disorders in the world, impacting 16% of the world’s population over the course of a lifetime1 and an estimated 2.7 million Canadians are impacted by migraine.2 Migraine has long been associated with dizziness symptoms – up to 69% of patients diagnosed with migraine also report at least occasional vertigo or dizziness.3 While complex and poorly understood, the relationship between migraine and dizziness may be due to anatomical and pathophysiological factors, such as neural pathway and neurotransmitter overlap and vascular and inflammatory processes.4,5
Updated Diagnostic Criteria
Dizziness and headache have long been associated; however, the definition of this disorder has been unclear and variously defined. Researchers have used several descriptions over the years to describe this relationship between dizziness and headache: migraine-associated vertigo, migrainous vertigo, vertiginous migraine, migraine-associated dizziness to name a few. In 2012, the Bárány Society6 and the International Headache Society7 provided consensus documents for proposed criteria for vestibular migraine (Figure 1) in order to better evaluate and manage these patients.
Figure 1. Current diagnostic criteria for +vestibular migraine and probable vestibular migraine.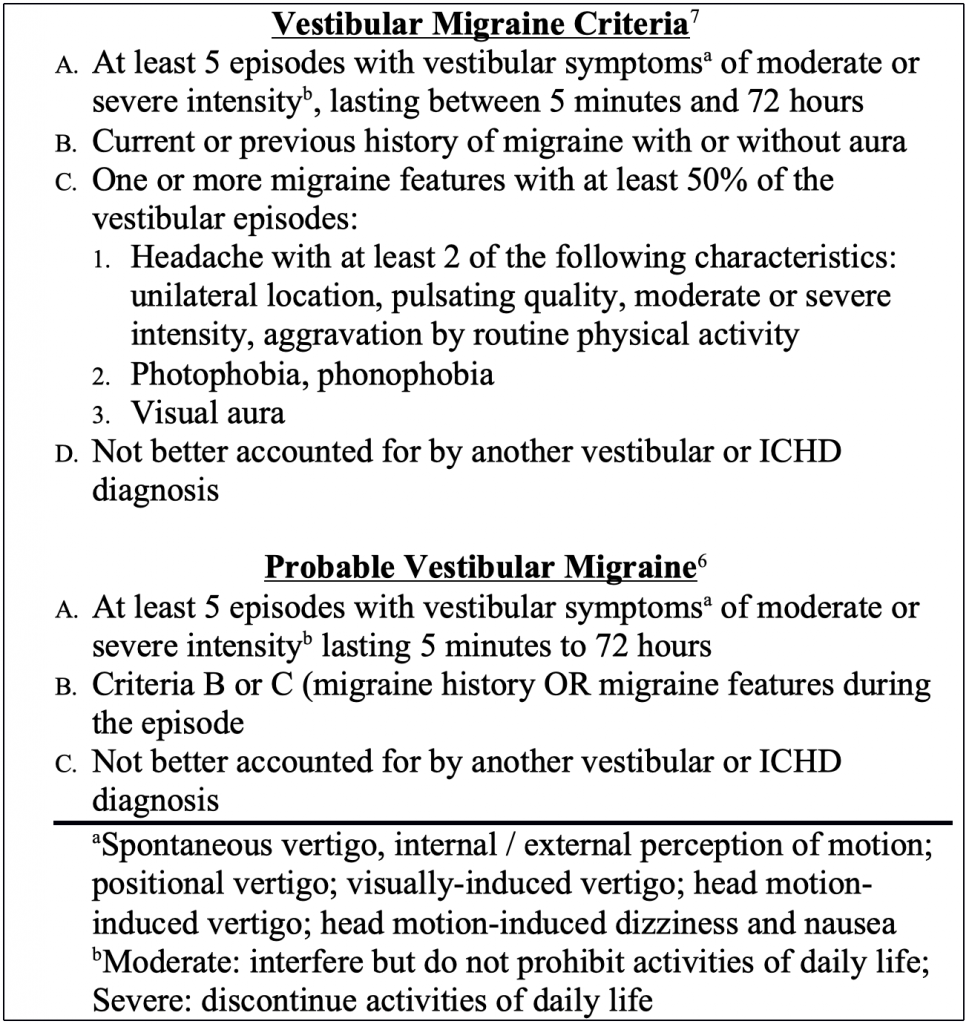
Episodic Vertigo – Differentiating the Possible Etiologies
There are significant challenges in diagnosing vestibular migraine. Keep in mind that there is no objective test specific for vestibular migraine – it is a diagnosis based on consensus criteria. These criteria are in beta form, meaning that they are still under evaluation and may be adjusted in the future as we learn more about this disorder. Additionally, not all patients with recurrent dizziness and headache history will meet the criteria for vestibular migraine, and therefore may need different management options. Other disorders that include recurrent dizziness, such as BPPV and Ménière’s disease may also be considered for these patients. To further complicate the diagnosis process, there is overlap among vestibular migraine and these other disorders presenting with recurrent dizziness. It is important to remember the diagnostic criteria for each of these disorders to determine the diagnosis; however, there is evidence that these pathologies may also co-exist in some patients.9,10
Vestibular Laboratory Findings
Can we isolate the vestibulopathy and identify vestibular migraine? This is challenging as there is no clinical diagnostic test for vestibular migraine. Look at this in terms of what we do in the vestibular laboratory – the vestibular diagnostician evaluates the vestibular system for what is working and perhaps what is not, but a management team is needed to determine the etiology. Audiologists do provide significant input to this team by providing objective measures and functional data for these complex patients. Now that a consistent criterion is used for vestibular migraine diagnosis, we can better look to our diagnostics to determine a “laboratory profile” (Figure 2). The majority of vestibular laboratories start with videonystagmography (VNG). In our laboratory, the VNG has not provided much in the way of a clinical profile, aside from ruling out a peripheral vestibulopathy. Occasionally, patients will demonstrate significantly saccadic smooth pursuit (10%). Caloric asymmetry is rare in our patient cohort, with 7% demonstrating significant asymmetry. Importantly, there was no evidence that these asymmetries were uncompensated. These data are somewhat less significant than previous reports, which found a larger percentage of caloric asymmetry in patients with headache.11 This is not too surprising as the diagnostic criterion have varied over time, leading to perhaps a wide range of patients included in these samples. Interestingly, recent literature suggests that otolith reflex pathway abnormalities may be a common characteristic in vestibular migraine. Our data found a significant proportion of bilaterally absent ocular VEMP responses (28%) as well as reduced amplitude and significant asymmetry as compared to controls.12 Importantly, these otolith reflex pathways have shown functional abnormalities as well, as measured by subjective visual vertical and horizontal tasks.13,14
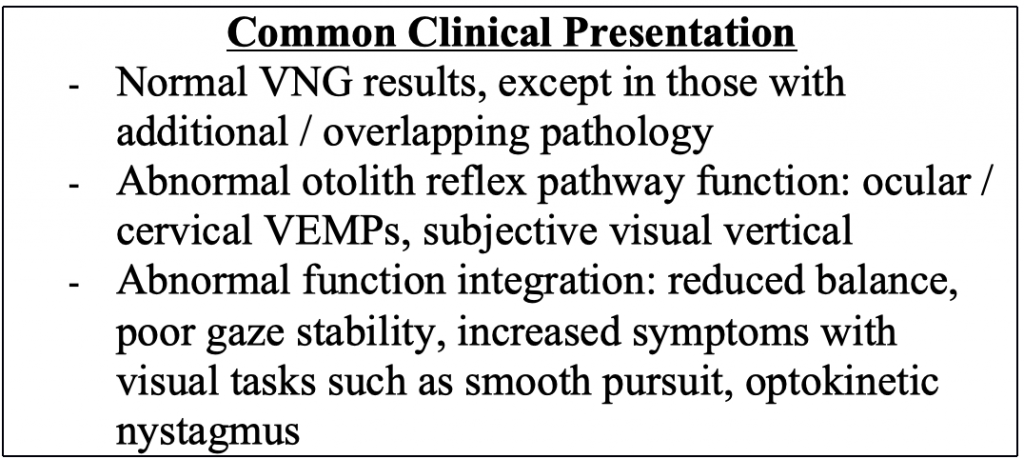
Because migraine impacts multisensory information processing,15 functional measures should be emphasized when a patient has suspected vestibular migraine. Posturography testing has found increased postural instability in patients with migraine while experiencing headache especially in eyes-closed conditions.16 Further, as many patients with vestibular migraine experience motion sensitivity, evaluating the influence of abnormal visual reference on postural stability is important.17 Our clinical data finds abnormalities in 44% of patients diagnosed with vestibular migraine when using the Sensory Organization Test. The abnormality pattern, however, is variable and demonstrate patterns associated with vestibular (12%), somatosensory (10%), and visual preference (6%). Another 6% demonstrate global imbalance while 10% were described as “aphysiologic” or “physiologically inconsistent.” This concept of aphysiologic balance function is interesting and may not actually be “aphysiologic” as we would describe in a malingering patient. It may relate more to the prevalence of anxiety in this population.18,19 Gaze stability is another functional metric that may be helpful in evaluating patient with vestibular migraine. Many patients with vestibular migraine describe increased dizziness with quick head turns. Tests such as the Dynamic Visual Acuity Test or Gaze Stability Test can quantify the changes in visual acuity with head movement and provide a target for rehabilitation services. The literature in this area is limited, but our clinical data has found abnormalities in 68% of patients with vestibular migraine using this test paradigm. Because semicircular canal function is generally appropriate in this group, these findings suggest atypical multisensory integration as contributing to dizziness symptoms.
Management Strategies
Vestibular migraine management requires a team approach for optimal outcomes. This team generally includes vestibular diagnosticians and otologists, physical therapists, psychiatrists, psychologists, and neurologists. The management strategy will vary based on the patient, but importantly there are numerous options that may be used for successful treatment. Table 1 provides a summary of the management options available as reported in the literature. Given that I am not a physician, I can only comment on what is reported in the literature regarding medical management. Collaboration with a headache specialist is best to manage these options. Recent literature has found valproic acid, venlafaxine, and flunarizine helpful as prophylactic treatment options to reduce the number, frequency, and severity of vestibular attacks.20
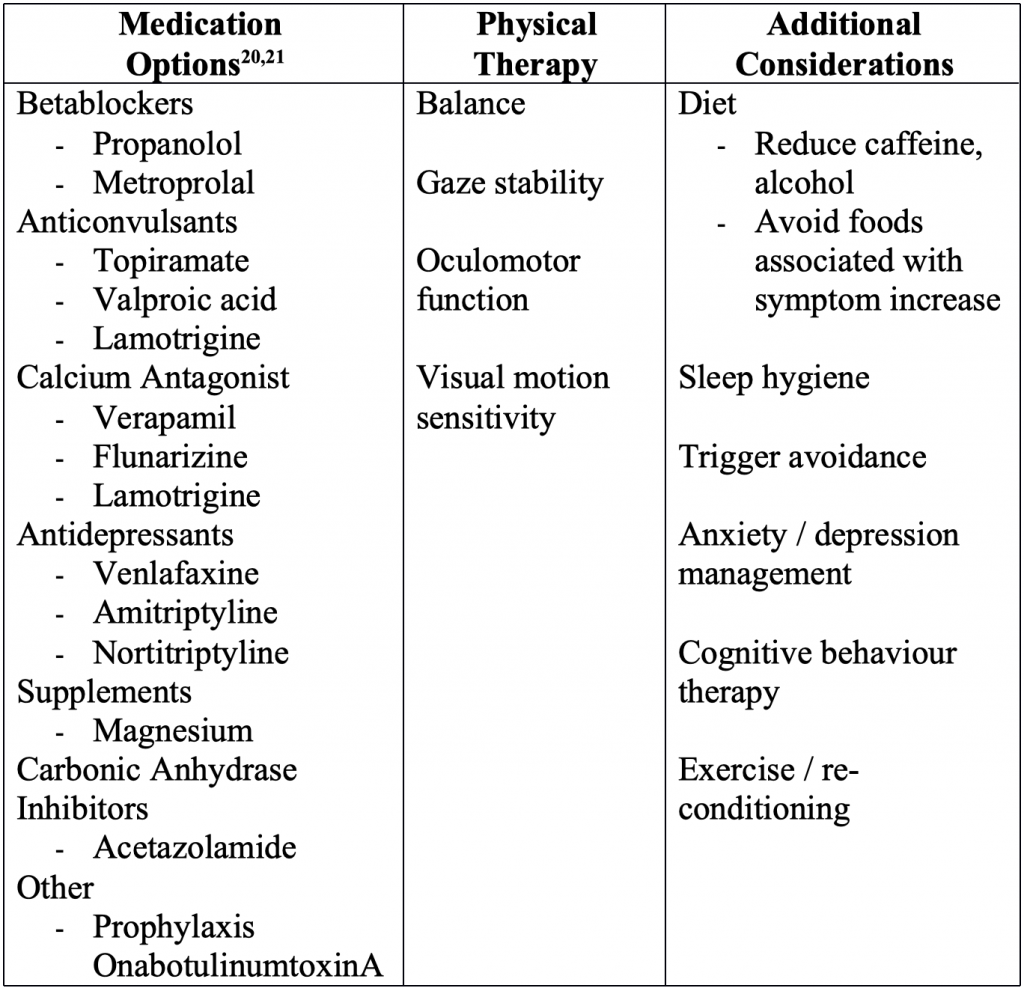
While medications may be indicated in many of these patients, the importance of vestibular rehabilitation should not be overlooked. Alghadir and Anwer22 provide a current review of available literature on the use of vestibular rehabilitation for those with diagnosed vestibular migraine. Because many of these patients do not effectively incorporate vestibular information, they are at risk for falls. Patients with vestibular migraine are challenging candidates for rehabilitation as they present with various comorbid conditions that also need to be addressed, including anxiety (overall anxiety as well as anxiety about dizziness), significant motion sensitivity, and hypervigilance.23,24 Even though this may be challenging for the patient to complete, our team finds that vestibular rehabilitation is a vital component of the management protocol, addressing the functional limitations present in these patients. Emerging literature that suggests that vestibular rehabilitation may also aid in reducing headache symptoms, anxiety, and self-report dizziness symptoms,25 further highlighting the importance of this component.
Conclusion
Vestibular migraine is a common, but unfortunately, overlooked etiology for patients with recurrent dizziness symptoms. Because these patients are often evaluated in the vestibular laboratory, we have the opportunity to assist in guiding them to the appropriate management team by ruling out characteristics associated with other etiologies, as well as providing information regarding the functional capabilities of the patient. All of this information helps to determine planning for rehabilitation options. Now that vestibular migraine has a standardized criterion, we can work together to better identify the patient characteristics and clinical laboratory findings associated with this patient group, further improving our ability to provide effective management.
References
- World Health Organization. The Global Burden of Disease: 2004 Update. Geneva; 2008.
- Ramage-Morin P, Gilmour H. Prevalence of migraine in the Canadian household population. Heal Rep 2014;25(6):10–16.
- Özge A, Aydinlar E, Tasdelen B. Grey zones in the diagnosis of adult migraine without aura based on the International Classification of Headache Disorders-III beta: exploring the covariates of possible migraine without aura. Pain Res Manag 2015;20(1):e1-e7.
- Furman J, Marcus D, Balaban C. Vestibular migraine: clinical aspects and pathophysiology. Lancet Neurol 2013;12:706–15.
- Lempert T, Neuhauser H. Migrainous vertigo. Neurol Clin 2005;23:715–30.
- Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res 2012;22:167–72.
- International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33(9):629–808.
- Formeister E, Rizk H, Kohn M, Sharon J. The epidemiology of vestibular migraine: a population-based survey study. Otol Neurotol 2018;39:1037–44.
- Murofushi T, Tsubota M, Kitao K, Yoshimura E. Simultaneous presentation of definite vestibular migraine and Meniere’s disease: overlapping syndrome of two diseases. Front Neurol 2018;9:749.
- Foster C, Breeze R. The Meniere attack: an ischemia/reperfusion disorder of inner ear sensory tissues. Med Hypotheses 2013;81(6):1108–15.
- Shin J, Kim C, Park H. Vestibular abnormality in patients with Meniere’s disease and migrainous vertigo. Acta Otolaryngol 2013;133(2):154–58.
- Zaleski A, Bogle J, Starling A, et al. Vestibular evoked myogenic potentials in patients with vestibular migraine. Otol Neurotol 2015;36(2):295–302.
- Ashish G, Augustine A, Tyagi A, Lepcha A, Belraj A. Subjective visual vertical and horizontal in vestibular migraine. J Int Adv Otol 2017;13(2):254–48.
- Winnick A, Sadeghpour S, Otero-Millan J, Chang T-P, Kheradmand A. Errors in upright perception in patients with vestibular migraine. Front Neurol 2018;9:892.
- Schwedt T. Multisensory integration in migraine. Curr Opin Neurol 2013;26(3):248–53.
- Anagnostou E, Gerakulis S, Voskou P, Kararizou E. Postural instability during attacks of migraine without aura. Eur J Neurol 2019;26:319–25.
- Lim Y-H, Kim J-S, Lee H-W, Kim S-H. Postural instability induced by visual motion stimuli in patients with vestibular migraine. Front Neurol 2018;9:1–8.
- Brasseaux R, Greve K, Gianoli G, Soileau J, Bianchini K. The relationship between the modified somatic perception questionnaire and dynamic platform posturography. Otol Neurotol 2008;29(3):359–62.
- Peres M, Mercante J, Tobo P, Kamei H, Bigal M. Anxiety and depression symptoms and migraine: a symptom-based approach study. J Headache Pain 2017;18(1):37.
- Liu F, Ma T, Che X, Wang Q, Yu S. The efficacy of venlafaxine, flunarizine, and valporic acid in the prophylaxis of vestibular migraine. Front Neurol 2017;8:1–5.
- Bisdorff A. Management of vestibular migraine. Ther Adv Neurol Disord 2011;4(3):183–91.
- Alghadir A, Anwer S. Effects of vestibular rehabilitation in the management of a vestibular migraine: a review. Front Neurol 2018;9:1–9.
- Vitkovic J, Winoto A, Rance G, Dowell R, Paine M. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol 2013;260(12):3038–48.
- Kutay Ö, Akdal G, Keskinoğlu P, Balcı B. Vestibular migraine patients are more anxious than migraine patients without vestibular symptoms. J Neurol 2017;264(Suppl 1):S37–S41.
- Sugaya N, Arai M, Goto F. Is the headache in patients with vestibular migraine attenuated by vestibular rehabilitation? Front Neurol 2017;8:124.

