How I Became Unethical
It all began…
…in the mid-1960s. I was at the University of Wisconsin studying for a PhD in audiology. Back then, if an audiologist dispensed (sold) a hearing aid, it was considered unethical behavior by the American Speech and Hearing Association (ASHA) and resulted in membership expulsion and loss of professional certification. The reasons given were that the audiologist as a professional should not profit financially from selling a hearing aid (or any other commercial product) and that selling products would compromise and influence our clinical decisions. That is, our responsibility to the patient did not extend beyond providing professional, objective advice.
This noble idea was inculcated with an utmost, nearly religious fervor. As a result, we students and practitioners alike internalized an unshakeable sense of moral rectitude and conscientiousness, for we believed we were members of a profession that eschewed even the slightest trace of questionable or unprincipled conduct. And this attitude, to the profession's credit, remains undiluted to this day.
However, as described below, this proscription had been put in place for a compelling reason other than assuring ethical behavior.
The genesis of our discontents…
The profession of audiology began only a couple of years after WWII; it simply did not exist before that time. It was the stepchild of other disciplines, including psychology, deaf education, speech pathology, psychoacoustics, and medical rehabilitation. The founders were engaged in a struggle to have audiology recognized as a serious, scholarly, independent field of study leading to universities' advanced degrees. It was crystal clear that audiology would not be admitted to the university graduate school if the sale of hearing aids were involved; avoiding instruction in retail principles and practices was a necessary and inevitable strategy.
This then was the ultimate but underappreciated origin of the decision for audiologists to refrain from hearing aid dispensing. It was put in place primarily to assure the acceptance of audiology as a respectable academic field of study. But it morphed into and was represented to us as a necessary and principled decision to protect the profession's reputation. Unfortunately, as we know, subsequently, this once reasonable determination had an inadvertent crippling and contentious effect on our profession for many years.
Audiology — a profession that had strayed…
Audiology is an outgrowth of programs instituted to care for WWII service members who had lost their hearing during wartime. Hearing aid selection and fitting had been one of the primary thrusts of the military rehabilitation program. But almost from its beginning, audiology moved away from its initial raison d'etre, and seeking scientific respectability in the eyes of the academy, had shuffled rehabilitation to the bottom of the audiology totem pole. In its place, developing and performing reliable and valid site of lesion diagnostic testing became the preferred mission of our profession. As a result, hearing aid selection and fitting became an ever more neglected part of the curriculum except regarding the evaluation and fitting of children.
In the early years, most university audiology programs had relatively few or no faculty members with expertise in technical, calibration, or acoustic matters, much less in hearing aid selection and fitting. Speechreading and auditory training techniques were felt to be of more value in hearing rehabilitation than amplification. For a professor, teaching hearing aid classes became the least desirable assignment; the practicum was often left in the hands of graduate assistants, and few students selected amplification as their major field of interest.
Some relevant history…
In the military hearing rehabilitation clinics of WWII, the procedure for fitting the two and three-piece vacuum tube body hearing aids of the time involved switching between different components, such as receivers, sometimes microphones or batteries, and the aids, to determine an acceptable fitting. (Figure 1).1 By comparing performance between different setups, using speech testing results followed by trial periods, sometimes for weeks, a specific body aid at a specific setting was selected for the veteran.2–4
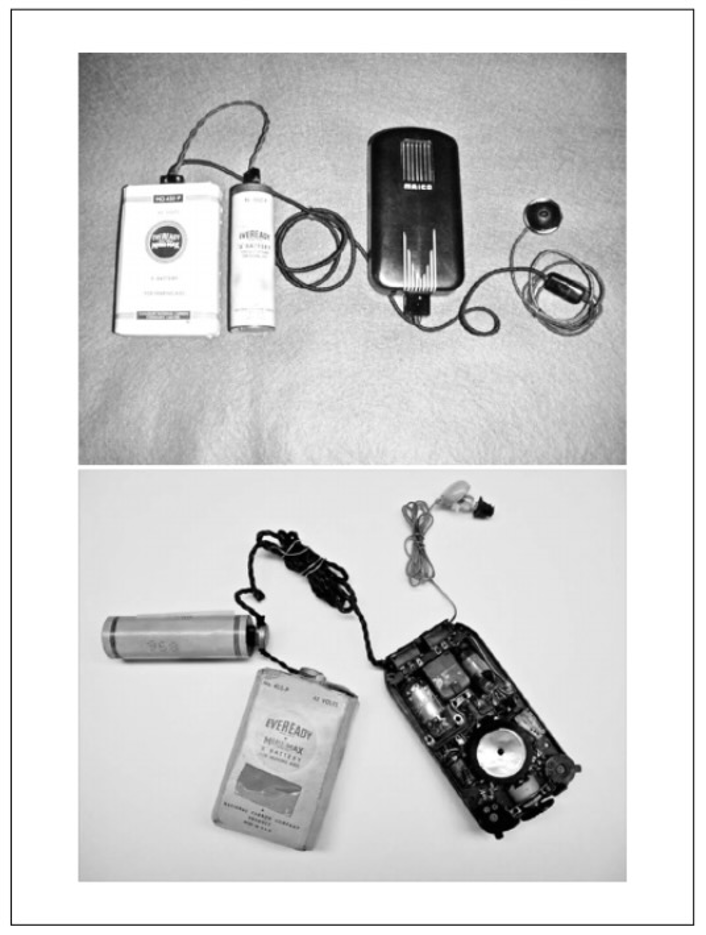
After the war, by the late 1950s, hearing aids had transitioned away from body-level aids to one-piece transistor-based ear-level instruments (see Figure 2). Despite this vast difference in product architecture and the extensive proliferation of both models and manufacturers that became available after the war, a shortened version of the WWII "comparative" fitting procedure continued to be taught and used in university clinics . . . despite studies and evidence that showed it to be unreliable.5–9 The authors of the prestigious Harvard Report (1947) specifically criticized the comparative method, labeling it as a waste of time that led to a "false sense of precision.”10
The retail marketplace…
During the 1940s to the 1960s, one could literally step off the bread truck yesterday and become a hearing aid dealer (dispenser) today. Minimal training was provided other than how to sell, and essentially no license was needed. However, a particular talent was required to convince people to buy the bulky, ugly, expensive, low fidelity instruments of the day. Plus, those who entered and left the business after a short stay sold the instruments and then dodged the after-fitting issues that invariably followed. The egregious behavior of these folks, especially those who sold aids from door-to-door and did not follow up, gave the hearing aid sales business a disreputable and unsavory reputation
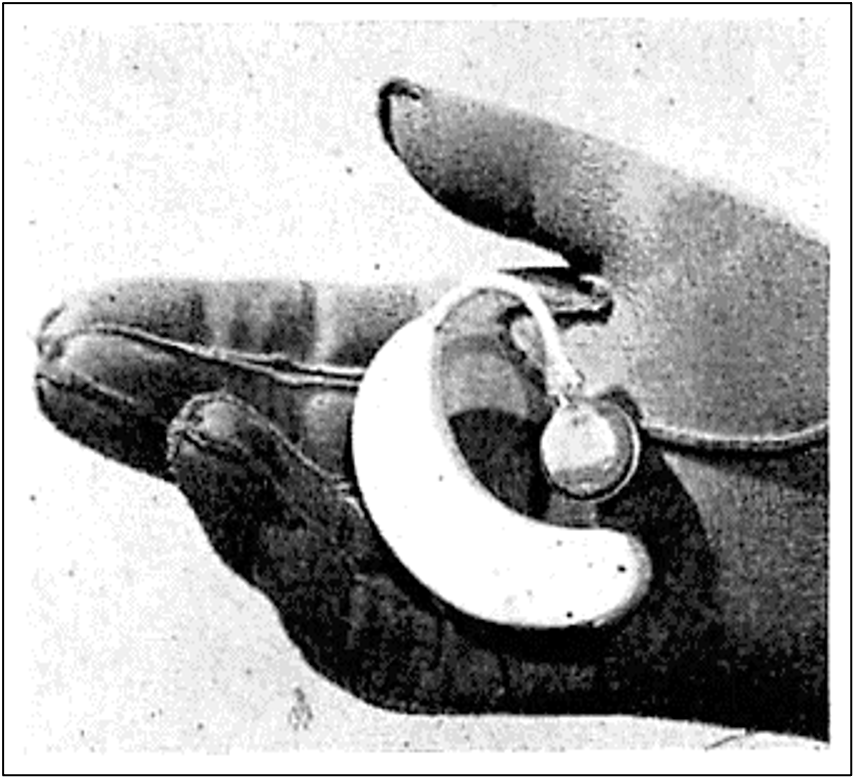
Dealers usually carried only one or two lines of hearing aids, and to fit them, they used master hearing aids furnished by the manufacturer, used rule of thumb formulas to figure out gain, or followed directions contained in the manufacturer's charts (See Figure 3).

A small minority of dealers did develop reasonably decent fitting techniques, knew how to counsel people appropriately and adjust their aids as best they could when things were not quite right, and learned to minimize their mistakes. In the end, the fitting expertise of the dealer essentially depended on learning from trial and error how to achieve acceptable goodness of fit, and some were quite competent. But even properly motivated dealers often found that despite their best intentions, a percentage of customers experienced issues and accused them of being deceptive or dishonest.
The patient runaround…
Both ENT and general practice physicians knew very little about hearing aids and understandably did not want to get involved with them. A patient with hearing loss might go to a doctor (maybe, rarely), who might refer them to an audiologist (rare, for only a few of us were around in the 1950-60s). Usually, the doctor skipped the audiologist and referred the patient directly to a dealer who did the actual fitting. And neither the doctor nor the audiologist, the primary specialists in treatment and management of patients with hearing impairment, ever saw the patient again because the patient returned to the dealer for any necessary follow-up.
Audiologists of the day knew very little about hearing aids, although they thought they did. They knew infinitely more about hearing and hearing disorders than the hearing aid dealer (or even many otolaryngologists at that time) but little about practical hearing aid fitting. On the other hand, even with their lack of academic training, a small number of dealers knew more about useful hearing aid fitting and patient care strategies than audiologists did.
Despite all that, audiologists, practicing in university and community clinics prescribed and recommended specific hearing aids for the patient to purchase (using the discredited modified comparative procedure). Clinics usually referred to a select few dealers, then held the dealer responsible for the success of the fitting. When the patient did not benefit, the dealer had to take the brunt of the patient’s dissatisfaction and the audiologist's criticism and perhaps lose future referrals. It was no wonder that the dealers grew to immensely dislike audiologists for setting themselves up as experts and authorities when they were neither.
Most all patients bypassed professionals and chose to go directly to a dealer. The situation was not a responsible state of affairs, and it was tragic in the case of children, for dealers typically had no idea how to deal with a profoundly deaf young child.
The product in all its glory…
The hearing aids of that time (the 1960s) were Model Ts compared to today, even the ear-level models. All aids were fitted with closed molds, often with deep canals, nearly always monaural. Audiologists at that time considered the fitting of two aids unethical, and dealers who did were deemed to be greedy and deceitful.
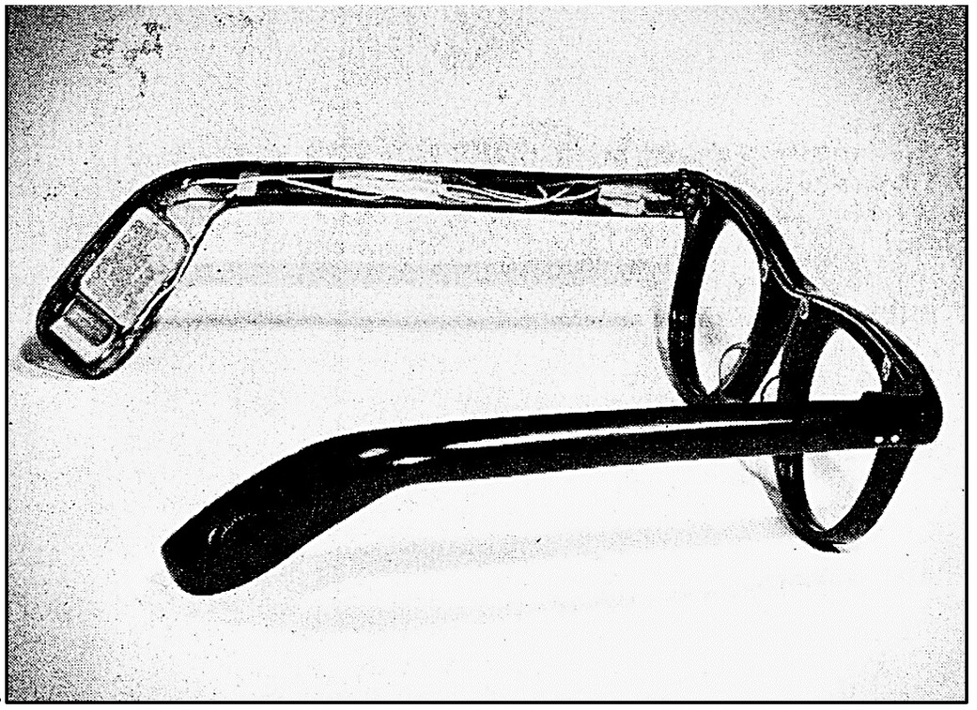
Earmold vents were used but necessarily kept relatively small, or feedback ensued. Two or three fixed response alternatives, sometimes mediated by insertion or removal of tiny screws, or in the case of body aids by changing receivers, might be available in a few selected models. Ear level instruments were quite large; eyeglass aids were very popular (in some years making up the majority of aids sold) but required the dispenser to learn how to adjust and fit eyeglasses. Battery life was short, amplifiers were peak clipping, and internal and external feedback was endemic. The ultimate irony was that most patients presented with mild to moderately severe, high-frequency sensorineural losses, yet the hearing aids of the day were usually designed for flatter, more advanced hearing losses.
To summarize, in those years (1950s-60s), hearing aids were crude, problematic, and unreliable, selection and fitting procedures were a joke, and responsible and informed patient care and follow-up was a crap game.
To dispense or not to dispense…
…that was the question. So, given the discouraging state of the hearing aid world at the time, why did I choose to begin dispensing?
While working on my PhD, a few other grad students at the University of Wisconsin and I had been debating for months with a part-time returning older student, Don Schaefer. He was taking audiology courses intending to open a hearing aid office in Madison that would only accept referrals from otolaryngologists – an exciting and new idea. However, he insisted that dispensing by audiologists was perfectly ethical and not a conflict of interest, and of course, we student audiologists argued vehemently with him.
Eventually, we came to an unexpected conclusion (to us) that he was quite correct: the only reasonable path for the profession, given the unfortunate state of hearing aid fittings in the clinic, was for audiologists to dispense directly. We audiologists would learn by on-the-job training what we did not know about hearing aids. Most importantly, with our academic training, the profession would develop (in time) rigorous, reliable procedures and methods for selecting and fitting aids that assured informed and efficacious treatment.
As to the concern about compromising one's ethics, if audiology could not educate and train its practitioners to make the right decisions for the patient, then the profession would be a failure from the start. Therefore, we concluded the obvious answer was for the profession to continue developing and training audiologists to be rigorously uncompromising in placing the patient’s needs above their own, as had been done successfully in other health professions.
This point of view was vigorously rejected and resisted by the ASHA and all the university faculties. Audiologists selling hearing aids was an idea that threatened their standing in the ASHA and the academy. The ASHA and the universities were firmly wedded to the notion that audiologists should remain a respectable distance from the sordid practices of the retail world.
1967: I engage in sordid practices…
With the help of Don Schaefer, who indeed had opened an office in Madison, I began to attend national and local hearing aid dealer meetings, never revealing my true identity as an audiologist, for my life would have been in mortal danger. For in general, dealers were the enemy, and they fervently disliked audiologists. Those were exciting times for me, however. I watched and listened and chatted with dealers of all stripes, learned about the companies and their philosophies, and attended their instructional courses, such as they were. As a result, I learned many new, interesting and unexpected things about amplification and met a small cadre of fine and respectable dealers; I felt I was the sole privileged participant in a heretofore secret world.
I began to work part-time with Don at his office, doing audiometric workups, repairing and cleaning hearing aids, and ultimately, one fine day in November 1967, I stepped off the cliff and sold and fitted my first hearing aid. No lightning, no thunder, no voice from heaven; life went on with nary a ripple.
Enamored with the mission and the financial opportunities that lie ahead, despite having completed all the courses and preliminary requirements for my PhD, I left the university while writing my dissertation. I moved to Minneapolis in early 1968 and opened a dispensing office selling Radioear and Audiotone hearing aids. A few other brave, pioneering souls, also accredited members of the ASHA with Master's degrees, later joined with me in the crusade, opening offices over the next two years in Detroit (John Schuneman), Philadelphia (Mel Sorkowitz), Milwaukee (Otis Whitcomb, who was with me briefly in Minneapolis), and Denver (Don Northey).
Reality raises its ugly head…
It was undoubtedly one of the most trying times I've ever experienced, and I began to have doubts about my decision. Without realizing it fully, I was attempting to implement a totally new dispensing concept with no previous experience, questionable selling skills, no business experience, and unreliable and ill-conceived products. Even some hearing aid companies refused to do business with me, for they did not want audiologists to compete with their dealers. I was new in town, so I visited all the ENT physicians in the Twin Cities to sell them on the new and startling idea of a free-standing audiology/dispensing facility and ask for their referrals. At that time, I knew of only one other ASHA accredited clinician who was engaged in private practice in all of North America, Olaf Haug, and he did not dispense hearing aids.
I learned to my chagrin and dismay that the professor who was the head of audiology at the University of Minnesota where I did my undergraduate studies was actively bad-mouthing my endeavors to the ENT doctors in the area, calling me an unethical and underqualified audiologist. Even more disheartening, some of my former fellow students were doing the same thing, telling ENT doctors not to refer patients to me. Understandably, the doctors had no idea where the truth was and were very hesitant to deal with an “unethical” audiologist.
It was difficult for me to accept the idea that I was an unethical professional when I knew within the deepest part of myself I was properly trained, motivated, and operating in patients' best interests. But I’m not surprised, in looking back, that I felt like an outcast, and no amount of self-talk helped rid me of that feeling nor its reality.
Living the life…
But I loved what I was doing. My fascination with the complex issues of providing useful amplification grew. Fortunately, about the time I started dispensing, open ear canal amplification was discovered.11-13 Although it involved using a CROS hearing aid, with the microphone on one side and the receiver and a tube on the other, the ability to provide high frequency amplification without feedback, even though in only one ear, was a revelation and allowed me to confidently fit patients with mild to moderate, high frequency losses, which were in abundance.14 I also found the Audiotone Auricon, a master hearing aid, to be invaluable in assisting me to make good decisions about selection and fitting, and cannot remember any of my patients returning their aid(s) out of dissatisfaction (see Figure 4).

I spent hours at my bench taking apart hearing aids, cleaning and reassembling them, soldering and installing CROS aids in eyeglasses, learning how to grind, modify and buff earmolds (see Figure 5). I read all I could about the different fitting philosophies of the time. Most of all, I began to learn how to encourage patients to accept amplification and fine-tune and resolve fitting problems as they arose.
I continued to attend state and national dealer's meetings, identifying and understanding their issues. Finally, a hearing aid licensing law was introduced at the state legislature after a few years, and I testified against its passage. It was ill-conceived, punitive, and it required all patients to be seen by an audiologist when in fact, there might have been only about 60-70 audiologists in the entire state, many of whom were teaching and not in clinical practice. This made me even more unpopular with some of my confreres, but a few others, on the other hand, were beginning to refer to me.
But referrals came slowly in the beginning. Rejection from most of the local audiologists was palpable, and then one day, I got a phone call from Ken Johnson, Executive Director of the ASHA, who was adamantly opposed to audiologists dispensing. He was friendly and said he understood my intentions were honorable, but he said on the day I had sold my first hearing aid, I had violated the ASHA Code of Ethics, and therefore I had revoked my membership by myself. An interesting way to put it, and I did not argue. Subsequently, a notice to that effect was circulated to some members of the ASHA. I tried not to care, but actually, I did, for no one wants to be viewed as an outlaw.
I join the carnival…
At the end of about two years, my office was operating in the black, after being in the red in the early days. I had developed a loyal following with some otolaryngologists, a few audiologists, and other referring sources, and my patients began referring their friends and relatives to me. But I soon realized that the actual job of dispensing hearing aids was becoming too repetitive and routine for me and was less a challenge than in the beginning.
The fact that each aid sold provided needed income was extremely important, but I was intrigued with the idea of professional dispensing becoming recognized and accepted. So I began to devote my spare time to becoming a small one-person marketing machine, writing letters and articles for periodicals and making speeches at state conventions and other professional meetings.
In the meantime, because I had testified against the dealer licensing bill, I had achieved the improbable reputation of being viewed by the industry as a reasonable and fair-minded audiologist. As a result, I began to be actively recruited by hearing aid manufacturers who realized that soon dealer licensing in each state was a foregone conclusion, and they needed someone to help prepare and educate their dealers. In addition, to help them, dealers and company executives alike, to understand the professional imperative. Most importantly, it was pointed out to me that I would have at my disposal a much bigger national platform from which to articulate and influence audiologists about the logic and appropriateness of dispensing. Of course, this appealed to me, so after pondering an offer and following a difficult winding down of the office, I accepted the position of Vice President of a large hearing aid company in December 1970.
The aftermath…
I subsequently spent 40 years happily and gainfully employed in the hearing aid manufacturing industry doing research, writing and speaking, influencing product quality and development, and engaging in professional affairs. When the ASHA abandoned the proscription against dispensing in the late 1970s, the Director of Audiology, Gene Del Polito, asked me to rejoin. However, when he said I would have to pay the dues in arrears from many years in the past, I politely declined, shedding no tears. After that, I actively supported any way I could the critically necessary founding of the American Academy of Audiology and the even more consequential shift to a doctoring profession.
At a convention some years later, my old professor at the University of Minnesota fell all over himself apologizing to me. Of course, I appreciated his apology, but it was unnecessary, for I knew what had motivated him. He was a true believer, a prisoner among many, handcuffed by the prohibitory injunction, and he firmly believed he was doing the right thing—protecting the profession.
But by then, opposition to our unlikely proposition of audiologists dispensing had withered quite away. Also, by then, I had received plenty of personal and professional recognition and accolades due to my part in the struggle. But more importantly, seeing the profession incorporate dispensing as an integral part of our professional mission has made the Sturm und Drang of those early years completely worthwhile.
The author wishes to thank and is grateful for his reviewers' careful editing and advice, Jerry Northern and Dave Preves.
References
- Curran, JR and Galster JA. The Master Hearing Aid. Trends in Amplification 2013; 27. DOI: 10.1177/1084713813486851
- Carhart R. Selection of hearing aids. Archives of Otolaryngology 1946; 44(1), 1–18.
- Carhart R. Tests for the selection of hearing aids. Laryngoscope 1946; 56, 780–794.
- Carhart R. Volume control adjustment in hearing aid selection. Laryngoscope 1946; 56: 510–526.
- Chial MR and Hayes CS. Hearing aid evaluation methods: Some underlying assumptions. Journal of Speech and Hearing Disorders 1974; 39: 27–79.
- McConnell F, Silber EF, and McDonald D. (1960). Test-retest consistency of clinical hearing aid tests. Journal of Speech and Hearing Disorders 1960; 25: 273–280.
- Schwartz DM. Hearing aid selection methods: An enigma. In GA Studebaker & FH Bess (Eds.), The Vanderbilt hearing- aid report. Upper Darby, PA: Monographs in Contemporary Audiology; 1982.
- Shore I, Bilger RC, and Hirsh IJ. Hearing aid evaluation: Reliability of repeated measurements. Journal of Speech and Hearing Disorders 1960; 25: 152–170.
- Walden BE, Schwartz DM, Williams DL, et al. Test of the assumptions underlying comparative hearing aid evaluations. Journal of Speech and Hearing Disorders 1983; 48: 264–273.
- Davis H, Stevens SS, Nichols RH, Jr., et al. Hearing Aids. An experimental study of design objectives. Harvard University Press, Cambridge, Massachusetts; 1947.
- Dodds, E., & Harford, E. (1968). Modified earpieces and CROS for high frequency hearing loss. Journal of Speech and Hearing Disorders, 11, 204-218.
- Harford, E., & Barry, J. (1965). A rehabilitative approach to the problem of unilateral hearing impairment: the contralateral routing of signals (CROS). Journal of Speech and Hearing Disorders, 30, 121-138.
- Harford, E., and Dodds, E. (1974). Versions of CROS hearing aids. Archives of Otolaryngology, 100, 50-57.
- Curran JR. How open canal amplification was discovered. Canadian Audiologist 2014; 1(6)


