Unperceived Hearing Loss among Canadians Aged 40 to 79
By Pamela L. Ramage-Morin, Rex Banks, Dany Pineault and Maha Atrach
DOI: https://www.doi.org/10.25318/82-003-x201900800002-eng
Abstract
Background: People with audiometrically measured hearing loss do not always self-report a hearing impairment.
Data and methods: Data were collected from 2012 through 2015 as part of the Canadian Health Measures Survey. The study sample was composed of respondents aged 40 to 79 with valid audiometric results for both ears (n = 3,964). Unperceived hearing loss was defined by four criteria: audiometrically measured hearing loss, no self-reported hearing impairment, no hearing aid(s) and no history of a hearing problem diagnosis.
Results: Of the 8.2 million older adults with measured high-frequency hearing loss, an estimated 77% (6.3 million) had hearing loss that was unperceived. Individuals who had never worked in a noisy environment were more likely to have unperceived hearing loss. People who had experienced tinnitus were less likely than others to have unperceived hearing loss.
Interpretation: Unperceived hearing loss occurs more often among those with mild or unilateral hearing loss and those who may not expect to experience hearing loss. Regular screening has been proposed to help raise awareness about hearing loss and to promote earlier detection and intervention that may ultimately improve the quality of life of those experiencing diminished hearing acuity.
Hearing loss consistently ranks among the top five causes of years lived with a disability 1-3 In Canada, an estimated 19% of adults (4.6 million) have at least mild hearing loss in the speech-frequency range (0.5, 1, 2 and 4 kHz).4 An even larger percentage of the adult population—35% (8.4 million)—have some degree of hearing loss in the high-frequency range (3, 4, 6 and 8 kHz)4 , which is where age-related hearing loss typically begins.5 In addition to the aging process, hearing loss may also result from hereditary factors, some chronic conditions, noise exposure, ototoxic substances and medications, or other factors .6-9 The diminished ability to process acoustic information can impede communication. For example, it can be difficult to hear or understand speech, converse in noisy environments and identify where sound is coming from.5,10
There are social and health consequences related to diminished hearing, including embarrassment, fatigue, anxiety, depression and distress;9-13 social isolation and participation restrictions;5,11,14 mobility issues, falls and other injuries;15-17 lower quality of life;12,16,18 cognitive decline and dementia;9,17,19-22 and mortality .23,24 The fatigue that is often reported by individuals with hearing loss may reflect the more intense levels of concentration required to process verbal information. This increased cognitive load is one possible explanation for associations between hearing loss and dementia, as the additional cognitive resources required for communication are used at the expense of those normally engaged for memory and other cognitive processes.21,25,26 The risk of cognitive decline and dementia exists even for those with mild levels of hearing loss.27 Problems with hearing acuity have been associated with other comorbid conditions, including diabetes and cardiovascular disease.9,13,17 The challenges and consequences associated with hearing loss can also extend beyond the individual to their family members and other communication partners as they adjust their interactions.18,28-31
Given the consequences of hearing loss, early recognition and intervention are important.11,13,18 However, the often insidious nature of hearing loss may present a barrier, as individuals and their communication partners may adapt to gradual changes in hearing acuity so that the loss progresses unnoticed.32 In contrast to the prevalence of hearing loss among Canadian adults, just 4% (867,000) of Canadian adults self-reported some level of hearing impairment.4 Even once hearing loss is suspected, there is still an average delay of seven years or more before an individual seeks help.33,34 Ayasse et al.10 described this delay as a critical public health issue. Untreated or delayed hearing loss treatment may be a missed opportunity, as interventions—such as the provision of hearing aids—have been shown to have a positive impact on quality of life.11,12 Furthermore, people who become aware of their early hearing loss may take extra precautions to protect their hearing and prevent or delay further loss.
Two cycles of the Canadian Health Measures Survey (CHMS) included audiometric evaluation, which is the gold standard for measuring hearing acuity,35-37 as well as survey questions38,39 on hearing ability assessed using the Health Utilities Index Mark 3 (HUI3).40,41 Self-reported data are less expensive and more convenient to collect than data from audiometric evaluations; therefore, they have potential for use in clinical practice and epidemiological studies.42-44 A number of studies have examined the associations between audiometrically measured hearing loss and self-reported hearing status primarily to assess the concordance between the two.35,42,44-47 The present study builds on this work: the CHMS provides a unique opportunity to examine the characteristics of the population with unperceived hearing loss—a term that refers to those who do not self-report a hearing impairment despite having some audiometrically measured hearing loss.48 Increasing awareness about unperceived hearing loss can reinforce the potential benefits of regular screening, early hearing loss detection and intervention.11-13,30,34,37
Data from cycles 3 (2012 to 2013) and 4 (2014 to 2015) of the CHMS were combined49 and used to examine the adult population aged 40 to 79 years with unperceived hearing loss. Analyses were limited to this age group for data quality reasons—the sample size was insufficient to provide reliable estimates of self-reported hearing impairment in those younger than 40. The analysis describes the prevalence of audiometrically measured hearing loss and self-reported hearing impairment. The prevalence of unperceived hearing loss was examined by selected sociodemographic, health and other characteristics.
Methods
Data source
The CHMS is an ongoing cross-sectional survey that samples households from five regions across Canada (Atlantic, Quebec, Ontario, Prairies and British Columbia). Participants provide demographic, socioeconomic, health and lifestyle information through an in-person, computer-assisted household interview, followed by direct physical measurements collected at a mobile examination centre (MEC). The CHMS excludes full-time members of the Canadian Armed Forces; residents of the three territories, First Nations reserves and other Aboriginal settlements, and certain remote regions; and residents of institutions such as nursing homes. Altogether, these exclusions represent approximately 4% of the target population. Proxy interviews were accepted in cases of physical or intellectual impairment.
Data from cycles 3 and 4 (2012 to 2013 and 2014 to 2015) were combined for this analysis. During each cycle, data were collected from January (year 1) through December (year 2) at 16 randomly selected sites and two MECs distributed across the five regions. The combined cycle 3 and 4 response rate for the household and MEC components was 52.7%. Details on the sampling design, data collection and response rate calculations are available in the CHMS data user guides38,39 and the Instructions for Combining Multiple Cycles of Canadian Health Measures Survey (CHMS) Data49 . Further information on the sampling frame and data collection is available at http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getInstanceList&Id=251160.
Study sample
This study was based on a sample of 3,964 respondents (1,989 men and 1,975 women) aged 40 to 79 years who had valid audiometric results for both ears. When weights were applied to the sample from cycles 3 (n = 1,990) and 4 (n = 1,974), the respondents represented a population of 15.2 million Canadians.38,39,49
Definitions
Measured hearing loss was established using audiometric evaluation and defined as a unilateral or bilateral pure-tone average greater than 25 dB in the worse ear over high frequencies (3, 4, 6 and 8 kHz). Severity of loss for prevalence estimates was defined as either mild (greater than 25 dB to 40 dB) or moderate to profound (greater than 40 dB). Hearing loss thresholds were based on the American Speech-Language-Hearing Association guidelines .50,51 The high-frequency pure-tone average was used as a continuous variable to control for the severity of hearing loss in the logistic regression models. Details on the CHMS audiometric evaluation are available elsewhere.4
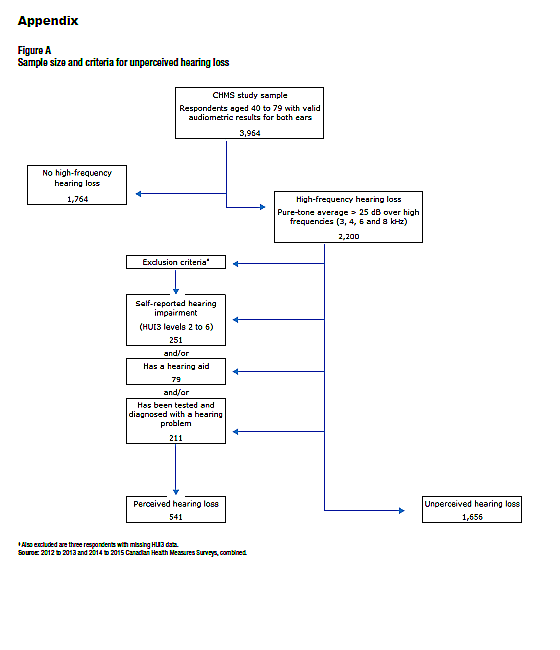
Respondents with audiometrically measured hearing loss who met the following three criteria were classified as having unperceived hearing loss (Appendix Figure A):
- They did not self-report hearing impairment. This was established using the HUI3 hearing attribute domain.40,52 HUI3 is a generic preference-based measure of functional health. Respondents were asked whether they are usually able to hear what is said in a group conversation with at least three other people, without a hearing aid. Those who responded “no” were asked follow-up questions, including whether they are usually able to hear what is said in a group conversation with at least three other people, with a hearing aid; whether they are able to hear at all; whether they are usually able to hear what is said in a conversation with one other person in a quiet room, without a hearing aid; and whether they are usually able to hear what is said in a conversation with one other person in a quiet room, with a hearing aid. Responses were scored according to an established algorithm and then categorized. A dichotomous variable identified individuals who did not report a hearing impairment (level 1) versus those who reported some hearing impairment or could not hear at all (levels 2 to 6).
- They did not own a hearing aid. Respondents were asked whether they had a hearing aid and, if they did, whether they had one for their left ear, right ear or both ears. Having a hearing aid, whether it was used or not, was considered a proxy for hearing loss awareness; therefore, these respondents were excluded from the unperceived hearing loss group.
- They had no past diagnosis of a hearing problem. Respondents who reported ever having their hearing tested were asked whether a health professional ever diagnosed them with a hearing problem. Those who responded “yes” were assumed to have some hearing loss awareness and were excluded from the unperceived hearing loss group.
In summary, people were classified as having unperceived hearing loss if they had an audiometrically measured high-frequency loss, no self-reported hearing impairment, no hearing aid(s) and no past diagnosis of a hearing problem.
The age groups—40 to 59 years and 60 to 79 years—were based on the CHMS sampling design.38,39 The older age group was further divided (60 to 69 years and 70 to 79 years) when sample numbers were sufficient. Age was entered as a continuous variable in the logistic regression models.
Respondents who were married or living with a common-law partner were grouped together and compared with those who were separated, widowed, divorced or single (never married).
Residents of households with two or more inhabitants were compared with those who lived alone.
Self-reported general health was categorized into two groups: good, very good or excellent, versus fair or poor.
People reported whether they had experienced tinnitus, which was described as “the presence of hissing, buzzing, ringing, rushing or roaring sounds in your ears when there is no other sound around you.”
Respondents were asked whether they had a regular medical doctor and were then grouped based on their “yes” or “no” response.
Respondents were also asked whether they had worked in a noisy environment (past or present), defined as one that was so loud that respondents and their co-workers had to speak in raised voices to be understood by or communicate with someone standing an arm’s length away. People who responded “yes” were then asked whether they were required to wear hearing protection at work. A dichotomous variable was used for the prevalence estimates; a second variable for the required use of hearing protection was created that included a “not applicable” category so that it could be included in the logistic regression models. Data for this group are not shown.
Analytical techniques
Weighted frequencies and cross-tabulations were calculated to examine the prevalence of hearing loss, self-reported hearing impairment, and unperceived hearing loss by sex, age group, and selected sociodemographic, health and work characteristics. Logistic regression was used to examine the odds of having unperceived hearing loss with variables that were significant in the bivariate analysis. The adjusted models controlled for sex, age and severity of hearing loss (high-frequency pure-tone average). Model 1 included health-related variables, while the two work-related variables were the focus of Model 2. To account for the complex survey design, variance estimation, coefficients of variation and significance testing (95% confidence intervals [CIs]) were done using the bootstrap technique with 22 degrees of freedom.53 Survey weights account for non-response so that the estimates represented the average Canadian household population aged 40 to 79 years over the survey timeframe (2012 to 2015). Analyses were conducted using SAS 9.3 and SAS-Callable SUDAAN 11.0 software.
Results
Audiometrically measured hearing loss
An estimated 54% of Canadians aged 40 or older (8.2 million) had at least mild hearing loss in the high-frequency range based on audiometric testing (Figure 1). Men were more likely than women to have hearing loss—63% versus 46%—as were older adults compared with those aged 40 to 59 years. For example, 93% of those aged 70 to 79 years had hearing loss, whereas this figure was 38% in the youngest group.

Self-reported hearing impairment
Overall, 6% of people aged 40 to 79 years were classified as having a hearing impairment, according to self-reported answers to the CHMS questions. Hearing impairment estimates were consistently lower than audiometrically measured hearing loss estimates, although similar trends by sex and age group were observed.
Unperceived hearing loss
Among the 8.2 million adults with audiometrically measured hearing loss, the majority (77%, or 6.3 million) had unperceived hearing loss (Table 1). It was more common among individuals whose measured loss was unilateral (86%) rather than bilateral (74%), and more common in those whose measured hearing loss was mild (93%) rather than moderate to profound (65%).

Factors associated with unperceived hearing loss
Table 2 presents the prevalence of unperceived hearing loss by selected characteristics. Based on these characteristics, no differences were observed in the prevalence of unperceived hearing loss for people with mild measured hearing loss.
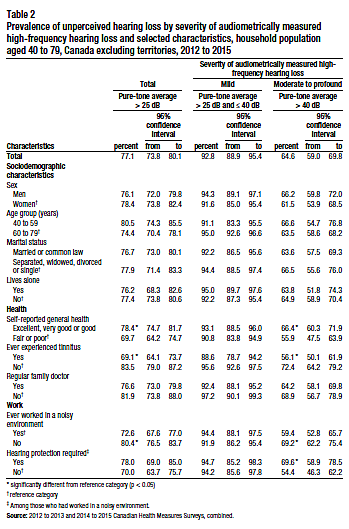
Among individuals with moderate to profound audiometrically measured hearing loss, those who reported good to excellent health were more likely to have unperceived hearing loss (66%) than those who rated their health as fair or poor (56%). People who had experienced tinnitus were less likely than those who had never had the condition to have unperceived hearing loss (56% versus 72%). Individuals who had never worked in a noisy environment were more likely to have unperceived hearing loss than those with noisy work experience. Among people who had worked in noisy environments, those who reported that hearing protection was required were more likely to have unperceived hearing loss. Other than these health and work-related characteristics, there were no differences in the prevalence estimates of unperceived hearing loss based on the selected sociodemographic factors of sex, age group, marital status and living arrangement.
Table 3 shows the odds of having unperceived hearing loss by selected characteristics. Increasing age was associated with lower odds (0.97) of having unperceived hearing loss when it was considered in isolation. However, this significant association was lost in the adjusted models. In both the unadjusted and adjusted logistic regression models, hearing loss severity was significant—as individuals’ high-frequency pure-tone average increased, the odds of having unperceived hearing loss decreased. After taking the pure-tone average, age and sex into account, people who had experienced tinnitus had lower odds (0.5) of unperceived hearing loss than the non-tinnitus population (Model 1), and individuals who had never worked in a noisy environment had significantly higher odds (1.6) of unperceived hearing loss than those with work experience in noisy environments. Despite these differences in the odds of having unperceived hearing loss, the prevalence of high-frequency hearing loss did not differ between those with a history of tinnitus (57%; 95% CI: 53 to 60) and those without (52%; 95% CI: 49 to 55), or between individuals who had worked in a noisy environment (57%; 95% CI: 52 to 61) and those who had not (53%; 95% CI: 49 to 56).

Discussion
This nationally representative study builds on earlier research that explored the concordance between hearing acuity measured with audiometric testing and self-reported measures.35,44,46 Data from the CHMS revealed that prevalence estimates of audiometrically measured hearing loss (in the high-frequency range) were consistently higher than subjective self-reported hearing impairment, which made it possible to identify a sector of the population characterized as having unperceived hearing loss—individuals with diminished hearing acuity, but no self-reported hearing impairment.
Mild hearing loss
There are a number of reasons why hearing loss may not be perceived. An obvious one is that, if the loss is minimal, it may remain undetected reflecting the often insidious onset of hearing loss.32,54 The study results support this possibility, as unperceived hearing loss was more common among individuals whose measured hearing loss was classified as mild, and the severity of loss based on the pure-tone average was significantly associated with unperceived hearing loss in the logistic regression models. However, among those with moderate to profound hearing loss, almost two-thirds had unperceived hearing loss, which indicates that factors other than severity of loss may also be important.
Compensation and adaptation
People experiencing the gradual onset of hearing loss may compensate and adapt so that the loss remains unnoticed and they continue to “hear effectively”.32,47 This study demonstrated that those with unilateral hearing loss were more likely to have an unperceived loss, suggesting that they may be compensating by relying on their better ear. People may gradually adapt by lip reading, moving closer to communicate and increasing the volume on their listening devices.55
Awareness triggering
Experiencing an emotional or social problem may be necessary to trigger hearing loss awareness and thereby reduce unperceived hearing loss.30,47 This awareness could be triggered by family, friends or co-workers expressing concern about the person’s hearing.28 They may witness maladaptive behaviours, including the person with the hearing impairment pretending to hear, guessing at what has been said and avoiding situations such as noisy restaurants that present hearing challenges.55 On the other hand, communication partners may contribute to or prolong an individual’s unperceived hearing loss by providing support to reduce any restrictions associated with the condition.56,57 No associations between marital status or living arrangements and unperceived hearing loss were revealed in the CHMS. This may reflect opposing processes taken by the communication partners of hearing impaired individuals—some may notice signs of hearing loss and point them out to the person, while other communication partners may adapt and compensate for the loss themselves, which reduces awareness. This could lead to a net result of no association at a population level.
Tinnitus
Experiencing tinnitus may also reduce unperceived hearing loss, as people seeking help for this condition would likely undergo audiometric evaluation, or the sounds of tinnitus could be enough on their own to draw someone’s attention to their hearing acuity. According to the CHMS, individuals who had experienced tinnitus were less likely to have unperceived hearing loss. This finding is consistent with the results from a large Korean study58 that found that those with tinnitus had lower odds of having unperceived hearing loss.
Denial and stigma
Denial could contribute to unperceived hearing loss, particularly at younger ages when communication demands from family as well as employment and other circumstances are higher.30,59 Hearing loss can be stigmatizing;47,60,61 therefore, people may reject any association with the condition and its accompanying ageist stereotypes .30,54 Denial and fear of stigmatization are understandable, as there can be substantial consequences for people with hearing impairments.54,60,61 Dalton et al.18 stressed the potential economic consequences of hearing loss when they reported the lower likelihood of full-time employment for men with hearing loss compared with those with normal hearing. Erler and Gartecki59 found that, among women, age was an important factor in the development of attitudes and feelings of stigma associated with hearing loss. They suggested that with increasing age, hearing loss and the use of hearing aids become more common and that familiarity promotes greater awareness, acceptance and less stigma.
Unexpected hearing loss
Hearing loss may be unperceived because it is unexpected, for example, among younger people of pre-retirement age.30 Hearing loss is associated with aging and declining health and therefore may be unexpected among those in good health. According to the CHMS, people who rated their health very positively were more likely to have unperceived hearing loss, although the association was attenuated when other factors were taken into account, a result that is consistent with those from the Korea National Health and Nutrition Examination Survey (KNHANES).58 The hearing loss of people who had never worked in a noisy environment may also be unexpected and—as a result—unperceived. According to the CHMS, they had higher odds of having unperceived hearing loss, which is also consistent with the KNHANES study that examined people who had experienced occupational noise exposure.58 This group of people with unexpected hearing loss is important for hearing loss awareness, as data from the CHMS show that the prevalence of high-frequency hearing loss did not differ significantly between those who had worked in a noisy environment and those who had not.
Screening
The higher prevalence of unperceived hearing loss among people who may not expect it suggests that proactive screening may be beneficial.11,32 Transitioning from unperceived hearing loss to awareness is a process that takes time.30,62 Jennings30 situates people with unperceived hearing loss in the pre-contemplation stage of the Transtheoretical Model. An individual needs to be aware of their hearing loss to move to the contemplation stage, where they can consider taking action, such as consulting a hearing professional. Early identification and treatment of hearing loss could help prevent the development of social isolation, depression, lower quality of life and other consequences of untreated hearing loss .11,63
Strengths and limitations
This study is based on a large sample representative of the Canadian population. It includes results from audiometric testing, as well as a subjective measure of hearing impairment from the HUI3. However, there are a number of limitations. The upper age limit of the CHMS is 79 years, which excludes an older sector of the population that is more likely to experience hearing loss. The CHMS is limited to people living in private households, which excludes individuals living in long-term care or other institutional settings. The onset and duration of hearing loss is unknown. Some surveys include subjective questions designed to be a proxy for audiometrically measured loss44,46 —such as “Do you feel you have a hearing loss?”—which provide an adequate estimation of measured hearing loss in the older population.44 The CHMS includes the HUI3 hearing attribute, which was designed to measure functional limitations or abilities in various circumstances (e.g., whether people are able to hear what is said in a group conversation with at least three other people, without a hearing aid) and was not designed as a proxy for audiometrically measured hearing loss.40,41 Some people may notice their diminished hearing acuity at the same time as they report that they did not have difficulty hearing. Consequently, the group classified as having unperceived hearing loss may include individuals who are truly unaware of their diminished hearing acuity, as well as those who are aware of their hearing loss but report no difficulty. This could be seen as a lack of acceptance of the hearing loss rather than an unperceived loss.30 Lastly, the CHMS is weighted to represent the population and adjusted for non-response. However, it is not known whether people with hearing loss or hearing difficulty were more or less likely to respond to the survey.
Conclusion
Although the term “unperceived hearing loss” has previously appeared in the literature,48 it is not widely used in audiology. However, it is a useful term for identifying a common phenomenon among Canadians in mid to later life. The high prevalence of unperceived hearing loss indicates that there is a need for better awareness among both individuals experiencing loss and health care providers.32 Becoming aware of hearing loss is a process,62 and regular screening is one strategy that was proposed to help reduce unperceived hearing loss.11,64,65 Regular screening provides an additional opportunity to detect comorbidities associated with hearing loss.65 Regular screening could lead to earlier detection and intervention that could ultimately improve the quality of life of those experiencing hearing loss.
What is already known on this subject?
- Hearing loss is one of the leading causes of years lived with a disability worldwide and can lead to social and health consequences, including embarrassment, fatigue, anxiety, depression, distress, social isolation, participation restrictions, falls and other injuries, lower quality of life, and mortality.
- There is a gap between subjectively reported hearing impairment and objectively measured hearing loss.
- In 2012 and 2013, an estimated 35% of Canadian adults had hearing loss in the high-frequency range, but only 4% reported that they had difficulty hearing.
What does this study add?
- Among Canadians aged 40 or older with hearing loss in the high-frequency range, 77% had unperceived hearing loss.
- Unperceived hearing loss was more common among adults with mild or unilateral measured loss.
- Individuals who had experienced tinnitus were less likely to have unperceived hearing loss, while the opposite was true for individuals who had never worked in a noisy environment, even after taking age, sex and hearing loss severity into account.
References
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386(9995): 743-800.
- Global Burden of Disease 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1545-602.
- Cunningham LL, Tucci DL. Hearing loss in adults. New England Journal of Medicine 2017; 377(25): 2465-2473. doi: 10.1056/NEJMra1616601.
- Feder K, Michaud D, Ramage-Morin P, McNamee J, Beauregard Y. Prevalence of hearing loss among Canadians aged 20 to 79: Audiometric results from the 2012/2013 Canadian Health Measures Survey. Health Reports 2015; 26(7): 10-17.
- Gates GA, Mills JH. Presbycusis. Lancet 2005; 366(9491): 1111-1120.
- May JJ. Occupational hearing loss. American Journal of Industrial Medicine 2000; 37:112-120.
- Fechter LD, Pouyatos B. Ototoxicity. Environmental Health Perspectives 2005; 113(7):A443-A444.
- Shearer AE, Hildebrand MS, Smith RJH. Hereditary Hearing Loss and Deafness Overview. 1999 Feb 14 [Updated 2017 Jul 27]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1434/.
- Besser J, Stropahl M, Urry E, Launer S. Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hearing Research 2018; 369: 3-14.
- Ayasse ND, Lash A, Wingfield A. Effort not speed characterizes comprehension of spoken sentences by older adults with mild hearing impairment. Frontiers in Aging Neuroscience 2017; 8:329. doi:10.3389/fnagi.2016.00329.
- Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on quality of life of elderly adults. Clinical Interventions in Aging 2012; 7:159-163.
- Nordvik Ø, Laugen Heggdal PO, Brännström J, Vassbotn F, Aarstad AK, Aarstad HJ. Generic quality of life in persons with hearing loss: a systematic literature review. BMC Ear, Nose and Throat Disorders 2018; 18:1. doi:10.1186/s12901-018-0051-6.
- McMahon CM. Gopinath B, Schneider J, Reath J, Hickson L, Leeder SR, Mitchell P, Cowan R. The need for improved detection and management of adult-onset hearing loss in Australia. International Journal of Otolaryngology 2013; http://dx.doi.org/10.1155/2013/308509.
- Ramage-Morin PL. Hearing difficulties and feelings of social isolation among Canadians aged 45 or older. Health Reports 2016; 27(10):3-12.
- Lin FR, Ferrucci L. Hearing loss and falls among older adults in the United States. Archives of Internal Medicine 2012; 172(4): 369-371.
- Lopez D, McCaul KA, Hankey GJ, et al. Falls, injuries from falls, health related quality of life and mortality in older adults with vision and hearing impairment – Is there a gender difference? Maturitas 2011; 69(4): 359-364.
- Karpa MJ, Gopinath B, Beath K, Rochtchina E, Cumming RG, Wang JJ, Mitchell P. Associations between hearing impairment and mortality risk in older persons: The Blue Mountains Hearing Study. Ann Epidemiol 2010; 20: 452-459.
- Dalton DS, Cruickshanks KJ, Klein BEK, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. Gerontologist 2003; 43(5): 661-668.
- Rutherford BR, Brewster K, Golub JS, Kim AH, Roose SP. Sensation and psychiatry: Linking age-related hearing loss to late-life depression and cognitive decline. The American Journal of Psychiatry 2018; 175(3):215-224.
- Lin FR, Metter EJ, O’Brien RJ, et al. Hearing loss and incident dementia. Archives of Neurology 2011; 68(2): 214-220.
- Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline among older adults. JAMA Internal Medicine 2013; 173(4):293-299.
- Lin FR, Albert M. Hearing loss and dementia – who’s listening? Aging & Mental Health 2014; 18(6):671-673.
- Genther DJ, Betz J, Pratt S, et al. Association of hearing impairment and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2015; 70(1): 85–90. doi:10.1093/gerona/glu094.
- Feeny D, Huguet N, McFarland BH, Kaplan MS, Orpana H, Eckstrom E. Hearing, mobility and pain predict mortality: a longitudinal population-based study. Journal of Clinical Epidemiology 2012; 65(7):764-777.
- Gurgel RK, Ward PD, Schwartz S, Norton MC, Foster NL, Tschanz JT. Relationship of hearing loss and dementia: a prospective, population-based study. Otology & Neurotology 2014; 35(5):775-781.
- Martini A, Castiglione A, Bovo R, Vallesi A. Aging, cognitive load, dementia and hearing loss. Audiology and Neurotology 2014; 19(Suppl 1): 2-5. doi: 10.1159/000371593.
- Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet 2017; 390(10113):2673-2734.
- Schulz KA, Modeste N, Lee J, Roberts R, Saunders GH, Witsell DL. Factors influencing pursuit of hearing evaluation: Enhancing the health belief model with perceived burden from hearing loss on communication partners. International Journal of Audiology 2016; 55(sup3):S69-S78.
- Scarinci NA, Hickson LM. Third-party disability in spouses of older people with hearing impairment. Perspectives on Aural Rehabilitation and Its Instrumentation 2012; 18: 3-12.
- Jennings MB. Audiologic rehabilitation needs of older adults with hearing loss: Views on assistive technology uptake and appropriate support services. Journal of Speech-Language Pathology and Audiology 2005; 29(3):112-124.
- Hétu R, Jones L, Getty L. The impact of a acquired hearing impairment on intimate relationships: implications for rehabilitation. Audiology 1993; 32(6): 363–381.
- Contrera KJ, Wallhagen MI, Mamo SK, Oh ES, Lin FR. Hearing loss care for older adults. Journal of the American Board of Family Medicine 2016; 29(3): 394-403. doi:10.3122/jabfm.2016.03.150235.
- Beck DL, Alcock CJ. Right product; wrong message. Hearing Review. 2014; 21(4):16-20.
- Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. (2007). Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technology Assessment 2007; (11)42: 1–294. doi:10.3310/hta11420.
- Kiely KM, Gopinath B, Mitchell P, Browning CJ, Anstey KJ. Evaluating a dichotomized measure of self-reported hearing loss against gold standard audiometry: Prevalence estimates and age bias in a pooled national data set. Journal of Aging and Health 2012; 24(3): 439-458.
- Baiduc RR, Poling GL, Hong O, Dhar S. Clinical measures of auditory function: The cochlea and beyond. Disease-a-month: DM 2013; 59(4): 147-156.
- Livshitz L, Ghanayim R, Kraus C, Farah R, Even-Tov E, Avraham Y, Sharabi-Nov A, Gilbey P. Application-based hearing screening in the elderly population. Annals of Otology & Laryngology 2017; 126(1):36-41.
- Statistics Canada (a). Canadian Health Measures Survey (CHMS) Data User Guide: Cycle 3. September 2015. Available by request at: http://www23.statcan.gc.ca/imdb-bmdi/document/5071_D4_T9_V2-eng.htm or Statistics Canada’s Statistical Information Service (toll-free 1-800-263-1136; 514-283-8300; infostats@statcan.gc.ca).
- Statistics Canada (b). Canadian Health Measures Survey (CHMS) Data User Guide: Cycle 4. October 2017. Available by request at: http://www23.statcan.gc.ca/imdb-bmdi/document/5071_D4_T9_V2-eng.htm or Statistics Canada’s Statistical Information Service (toll-free 1-800-263-1136; 514-283-8300; infostats@statcan.gc.ca).
- Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single-attribute utility functions for the Health Utilities Index Mark 3 System. Medical Care 2002; 40(2): 113-28.
- Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health and Quality of Life Outcomes 2003; 1:54.
- Kamil RJ, Genther DJ, Lin FR. Factors associated with the accuracy of subjective assessments of hearing impairment. Ear and Hearing 2015; 36(1):1 64-167.
- Swanepoel DW, Eikelboom RH, Hunter ML, Friedland PL, Atlas MD. Self-reported hearing loss in baby boomers from the Busselton Healthy Ageing Study: Audiometric correspondence and predictive value. Journal of American Academy of Audiology 2013; 24(6): 514-521.
- Sindhusake D, Mitchell P, Smith W, Golding M, Newall P, Hartley D, Rubin G. Validation of self-reported hearing loss. The Blue Mountains Study. International Journal of Epidemiology 2001; 30(6):1371-1378.
- Louw C, Swanepoel DW, Eikelboom RH. Self-reported hearing loss and pure tone audiometry for screening in primary health care clinics. Journal of Primary Care & Community Health 2018; 9:1-8.
- Kim SY, Kim HJ, Kim MS, Park B, Kim JH, Choi HG. Discrepancy between self-assessed hearing status and measured audiometric evaluation. PLoS One; 2017; 12(8):e0182718. doi:10.1371/journal.pone.0182718.
- Smith SL, Kricos PB. Acknowledgement of hearing loss by older adults. Journal of the Academy of Rehabilitative Audiology 2003; 36:23-35.
- Rifai K, Pischke S, Agne C, Rosenau J, Klempnauer JL, Manns MP. High rate of unperceived hearing loss in patients after liver transplantation. Clinical Transplantation 2012; 26(4): 577-580. doi: 10.1111/j.1399-0012.2011.01592.x
- Statistics Canada (c). Instructions for Combining Multiple Cycles of Canadian Health Measures Survey (CHMS) Data. Ottawa: Statistics Canada, 2017. Available by request at: http://www23.statcan.gc.ca/imbd-bmdi/document/5071_D4_T9_V2-eng.htm or Statistics Canada’s Statistical Information Service (toll-free 1-800-263-1136; 514-283-8300; infostats@statcan.gc.ca).
- Clark JG. Uses and abuses of hearing loss classification. ASHA: A Journal of the American Speech-Language-Hearing Association 1981; 23(7): 493-500.
- American Speech-Language-Hearing Association (ASHA). Degree of Hearing Loss. Available at: http://www.asha.org/public/hearing/Degree-of-Hearing-Loss/. Accessed 11 December 2018.
- Feng Y, Bernier J, McIntosh C, Orpana H. Validation of disability categories derived from Health Utilities Index Mark 3 scores. Health Reports 2009; 20(2): 43-50.
- Rust KF, Rao JNK. Variance estimation for complex surveys using replication techniques. Statistical Methods in Medical Research 1996; 5: 281–310.
- Hétu R, Riverin L, Getty L, Lalande NM, ST-Cyr C. The reluctance to acknowledge hearing difficulties among hearing-impaired workers. British Journal of Audiology 1990; 24(4): 265-276.
- Hallberg LR-M, Hallberg U, Kramer SE. Self-reported hearing difficulties, communication strategies and psychological general well-being (quality of life) in patients with acquired hearing impairment. Disability and Rehabilitation 2007; 1-10.
- Cox RM, Alexander GC, Gray GA. Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear and Hearing 2005; 26(1):12-26.
- Knudsen LV, Öberg M, Nielsen C, Naylor G, Kramer SE. Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification 2010; 14(3):127-154.
- Choi JE, Moon IJ, Baek S-Y, Kim SW, Cho Y-S. Discrepancies between self-reported hearing difficulty and hearing loss diagnosed by audiometry: prevalence and associated factors in a national survey. BMJ Open 2019; 9:e022440. doi: 10.1136/bmjopen-2018-022440.
- Erler SF, Garstecki DC. Hearing loss- and hearing aid-related stigma: Perceptions of women with age-normal hearing. American Journal of Audiology 2002; 11(2): 83-91.
- Southall K, Gagne J-P, Leroux T. Factors that influence the use of assistance technologies by older adults who have a hearing loss. International Journal of Audiology 2006; 45(4): 252-9.
- Southall K, Gagne J-P, Jennings MB. Stigma: A negative and positive influence on help-seeking for adults with acquired hearing loss. International Journal of Audiology 2010; 49: 804-814.
- Engelund G. “Time for hearing” – recognising process for the individual. PhD thesis, Department of Nordic Studies and Linguistics Audiologopedics, University of Copenhagen & Oticon Research Centre, Eriksholm. 2006.
- Schulz KA, Modeste N, Lee J, Roberts R, Saunders GH, Witsell D. Factors influencing pursuit of hearing evaluation: Enhancing the health belief model with perceived burden from hearing loss on communication partners. International Journal of Audiology 2016; 55:sup3, S69-S78. DOI: 10.3109/14992027.2015.1136437.
- Karlsmose B, Lauritzen T, Engberg M, et al. A randomized controlled trial of screening for adult hearing loss during preventive health checks. British Journal of General Practice 2001; 51:351–355.
- Bray V. A holistic approach to managing hearing loss and its comorbidities. The Hearing Journal 2018; 71(11):14-17. doi: 10.1097/01.HJ.0000549524.79131.ab.
Appendix