An Audiology Ripple Effect
From the Labs to the Clinics
Renowned auditory researcher Dr. Robert Harrison brings us up to date on information and research from the Labs. Appropriately titled “From the Labs to the Clinics”, Bob is involved in laboratory and applied/clinical research, including evoked potential and otoacoustic emission studies and behavioural studies of speech and language development in children with cochlear implants. For a little insight into Bob’s interests outside the lab and the clinic, we invite you to climb aboard Bob’s Garden Railway.

In the history of audiology, many new ideas and methods have come and gone. Some things that were once new, like ear trumpets and tuning forks to assess hearing, are now gone (at least for most hearing healthcare professionals). Likewise, some brilliant methods to evaluate hearing, such as the Bekesy audiometry and the tone-decay test, appear to have been abandoned. I don't know why because they were so informative.
Some novel testing methods, such as the measurement of otoacoustic emissions (OAEs), have significant value for probing the important cochlear mechanisms. For example, OAEs indicate the status of the outer haircell cochlear amplifier and can help distinguish hearing loss caused by outer vs. inner haircell dysfunction. However, apart from the widespread and essential use of OAEs for newborn hearing screening, I do not see much uptake of emission testing in regular clinical assessments. On that note, in a subsequent CA column, I will write more in favour of OAE testing for hearing loss diagnosis.
Today I want to remind you, or inform you for the first time, about a hearing test that was suggested more than 6 decades ago but was never adopted as a clinical tool in audiology despite its value as a diagnostic tool and its simplicity of method. I am referring to the measurement of the audiogram fine structure.
In 1958, E. Elliott published as a short communication in the prestigious journal Nature titled: A Ripple Effect in the Audiogram.1 (Prof. Elliott was involved in psychoacoustics research at the Admiralty Research Laboratory, London, but I cannot find any other publications by this author.) The ripple effect in the audiogram is perfectly displayed in the one published figure shown below.
These audiograms show are hearing thresholds measured between 400 Hz and 4 kHz in two normal hearing subjects, but in contrast to clinical audiograms measured with tones at octave intervals, these were measured with test tones presented at 10 Hz intervals.
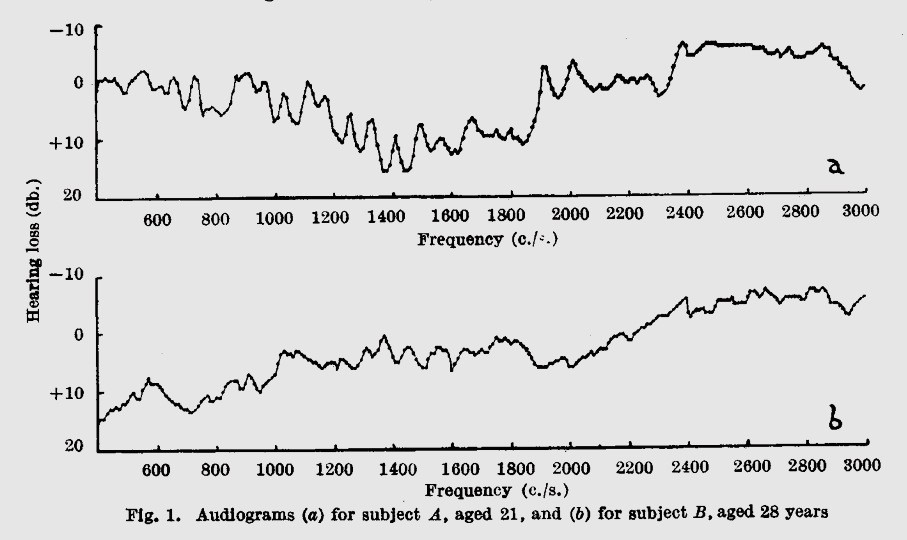
The fine frequency steps of the test procedure revealed, in normal hearing subjects, narrow peaks, and valleys in threshold, often exceeding10 dB. Compare this “real audiogram” to the clinical audiogram where a few test points are joined by straight lines!
Now that we understand more about cochlear physiology and how outer haircells boost the mechanical motion of the organ of Corti along the length of the cochlea, the origins of the audiogram ripple become clear. The small peaks in the fine structure most likely reflect variations in the cochlear amplifier gain along the cochlear length.
What, you might ask, would be the clinical value of knowing about cochlear amplifier status in patients? Well, the value could be very significant. This fine structure reflects outer haircell activity and provides similar information to that gained from recording OAEs. In types of sensorineural hearing loss where outer haircells are damaged, the audiogram ripple (and OAE amplitudes) are reduced. As with OAEs, audiogram fine structure can inform us about the etiology of hearing loss, allow many forms of differential diagnosis and tell us what cochlear mechanisms are dysfunctional.
My columns in Canadian Audiologist are all about knowledge translation: “From the Labs to the Clinic.” So why was this gem of an idea never adopted in clinical audiology?
References
- Elliott E. A Ripple Effect in the Audiogram. Nature 1958;181:1076. https://doi.org/10.1038/1811076a0