Scrutiny of New Technique Ushers in Evidence-Based Changes in Practice

Bone anchored hearing devices have provided a niche solution in the rehabilitation of some of our patients with hearing loss. While an intolerance or inability to wear conventional devices is a general indication they have a well-established place in the rehabilitation of those with a large conductive loss but a well-preserved bone curve. Use in mixed loss or in single sided sensorineural loss is a little more contentious.For the first 20 years of its existence the surgical technique and equipment changed little. Key surgical steps included a lengthy and quite bloody reduction in scalp thickness to permit the placement of a relatively short abutment.1 Many were previously performed under general anesthesia at our institution for precisely these reasons.
In 2011, Hultcrantz et al. described the Minimally Invasive Ponto Surgery (MIPS) procedure using a 5-mm dermal punch to remove the limited tract of soft tissue needed to accommodate the Ponto (Oticon, Copenhagen, Denmark) abutment.2 The drilling procedure was then completed in seconds, through a cannula placed to protect the skin and soft tissues while holding cooling fluid.
MIPS heralds a departure from the traditional “open approach” to percutaneous fixture placement. The procedure has resulted in a simplification of the surgical steps and a dramatic reduction in surgical time (Figure 1). Our group at Dalhousie University saw the significant reduction in surgical time and procedural invasiveness as a logistical opportunity to move such cases out of the main operating room. Having been involved in animal lab prototype testing of the technique during its development in Scandinavia, the team were keen to be early adopter of the technique. The first fixture was placed on 11 March 2016 and after completing an initial cohort of a dozen surgeries a self-imposed moratorium was observed while the recipients were carefully monitored. We sought to perform a quality assurance project using our own small prospective cohort to justify this change in practice.
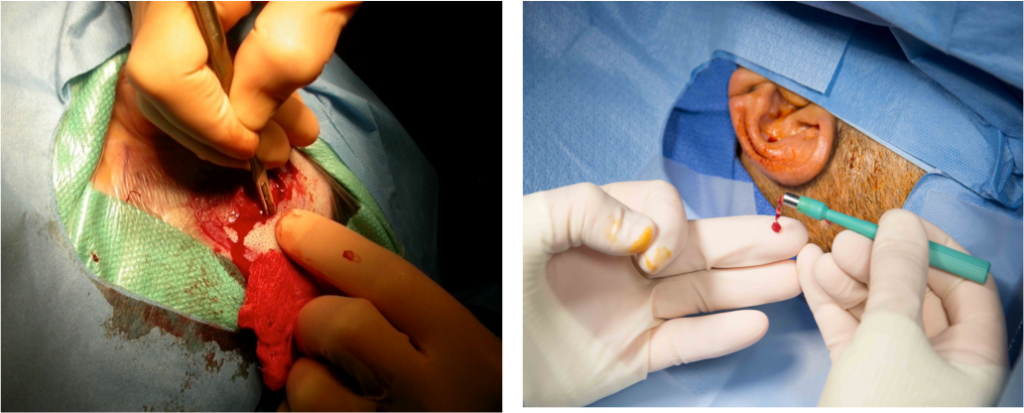
Figure 1. Bleeding and dissection are strikingly reduced with the MIPS approach (right) compared to the more intrusive open approach (left).
We investigated the long-term safety and stability of the abutments in the Halifax case-series. Early evidence from soft tissue preserving techniques for BAHD suggest favorable and safe outcomes.1 With this in mind, we coordinated MIPS research clinic was used to follow patients, assess the implant site and gather qualitative information through patient interviews and surveys. The patient’s soft tissue status around the implant was evaluated independently by three different assessors using the Inflammation, Pain, Skin Height (IPS) Scale proposed by Kruyt.3 Patients qualitative perspectives were assessed using the Surgical Satisfaction Questionnaire (SSQ-8) modified for MIPS and through a semi-structured interview that assessed their experience.
Our study has demonstrated that it is possible to maintain secure fixture/abutment placement with the MIPS procedure. With a minimum follow-up of 1 year, skin complications were low, consistent with other investigators. Implants were stable, and it is reassuring to us that no fixtures were lost in this highly-scrutinized cohort.4 The mean (SD) soft tissue status score averages using the IPS Scale were low for inflammation 0.1 (0.1), pain 0.1 (0.1), skin height 0.2 (0.1) and total IPS score 0.4 (0.3) indicating minimal soft tissue changes.
Patient experiences with MIPS were overwhelmingly positive. All patients reported speedy recoveries, often getting back to routine activities the next day. The surgical experience was felt to be minimized, with patient’s reporting they received high quality care. Issues reported included getting used to having a foreign object on their head and initial maintenance of the implant site (Figure 2).

Figure 2. A sample of follow-up abutment site pictures taken at the parallel research clinic most recent visit.
The mean time for the MIPS procedure was 5 minutes and 55 seconds (0.10 hours) and 1 hour and 7 minutes (1.13 hours) for the open approaches.5 We confirmed a total cost saving of $456.83 for MIPS compared the open approaches through the direct cost analysis5. The comparative cost saving calculated is independent of surgical venue meaning that the cost saving will be evident at institutions where moving MIPS outside the main OR is not possible. Indirect cost savings to the healthcare system include the benefit of regaining over two hours of prime operating time including procedure and turnaround that frees up facilities and staff to allow for other more urgent operations to be completed. In addition to this, the logistical consideration of performing MIPS procedures as day cases is that a hospital bed is not required. Procedures will not be cancelled due to a lack of overnight hospital bed availability. Hospital resources can be channeled more efficiently for surgical procedures that necessitate an overnight bed (Table 1).
Table 1. The Costs and Number of Healthcare Providers (HCP) Required for MIPS versus Open Techniques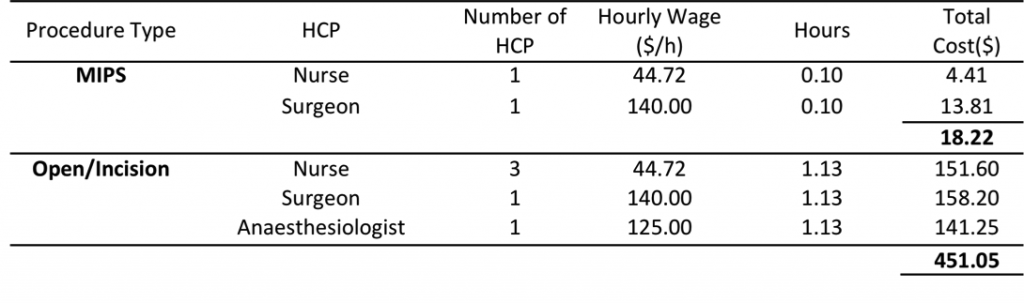
It is intuitive and entirely feasible that equipment costs can be reduced even further in the future. Once out of the operating room setting, we reviewed the items required for this short procedure. The arrangement shown below (Figure 3) is a significant departure from the previous requirement to open a full surgical tray. These proposals have clear implications both for costs associated with initial outlay to purchase items and equipment and for the subsequent costs of sterilizing and maintaining such equipment.
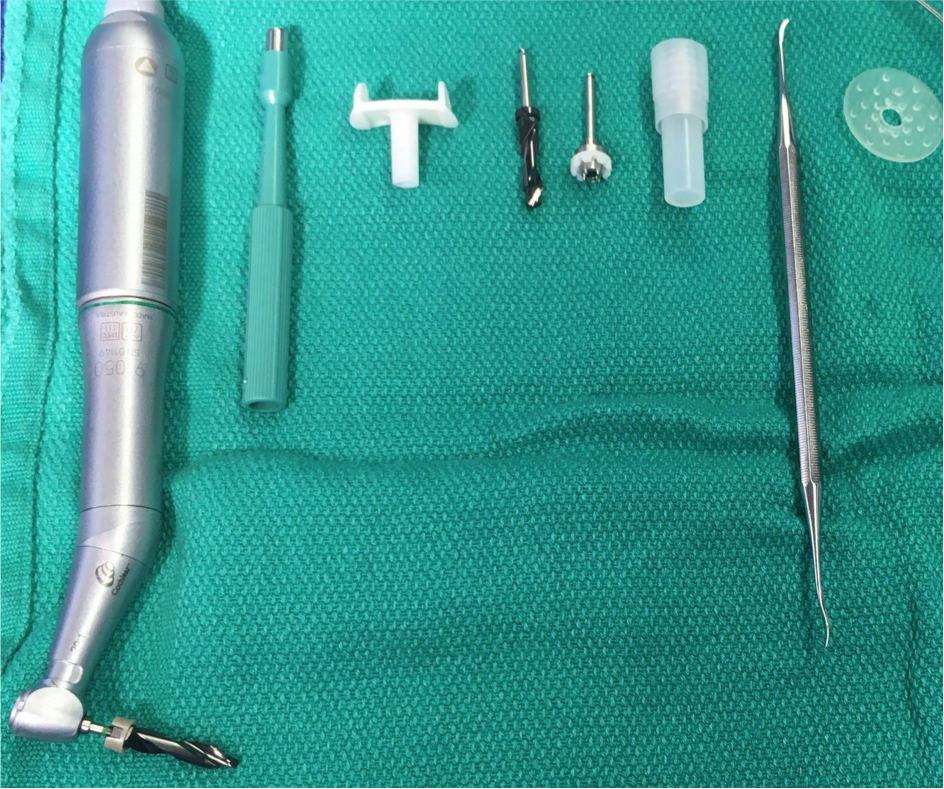
Figure 3. Proposed reduction in surgical tray. From left: Drill with bit, skin punch, cannula, countersink drill bit, handpiece connector, combined abutment and fixture, raspatorium/ dissector, healing cap.
To date, there have been few MIPS case series published. Bonilla et al. showed promising MIPS outcomes in their cohort, confirming a shorter procedure time and fewer skin complications one week after surgery when compared to the linear incision technique6. While details of other experiences are limited, there are mixed results reported.7 The highly anticipated long-term, multi-centre MIPS outcomes data recently published showed no difference in inflammation compared to linear incisions.8–10 There was improvement in skin sensation, sagging, cosmetic result and reduction of surgical time but a non-significant increase in implant extrusion rate that warrants further investigation.8–10
This is the first published study documenting the direct cost benefits of the MIPS procedure compared to open approaches. As one of the first North American adopters of the MIPS procedure, we thought it diligent to perform a quality assurance project using our own original prospective cohort. Our findings conclude both device stability and patient satisfaction with no loss of fixtures. In consequence, we now perform MIPS placements uniquely. All surgeries are performed under local anesthesia in clean facilities in our brachytherapy suite. Our work has been widely disseminated through publication in the Canadian Journal of Otolaryngology and through presentations at OSSEO.
References
- Johansson M, Holmberg M, Hultcrantz PM. Bone anchored hearing implant surgery with tissue preservation – A systematic literature review. Oticon Med Rev. 2015;
- Hultcrantz M. Outcome of the bone-anchored hearing aid procedure without skin thinning: a prospective clinical trial. Otol Neurotol. 2011;32(7):1134–9.
- Kruyt IJ, Nelissen RC, Johansson ML, Mylanus EAM, Hol MKS. The IPS-scale: A new soft tissue assessment scale for percutaneous and transcutaneous implants for bone conduction devices. Clin Otolaryngol. 2017;42(6):1410–3.
- Sardiwalla Y, Jufas N, Morris DP. Long term follow-up demonstrating stability and patient satisfaction of minimally invasive punch technique for percutaneous bone anchored hearing devices. 2018;5:1–7.
- Sardiwalla Y, Jufas N, Morris DP. Direct cost comparison of minimally invasive punch technique versus traditional approaches for percutaneous bone anchored hearing devices. J Otolaryngol - Head Neck Surg. 2017;46(1):4–9.
- Bonilla A, Magri C, Juan E. Findings from the experience with the punch technique for auditory osseointegrated implants: A retrospective single center comparative study. Acta Otorrinolaringol Esp [Internet]. 2017;68(6):309–16. Available from:http://www.embase.com/search/resultssubaction=viewrecord&from=export&id=
L616411577%0Ahttp://dx.doi.org/10.1016/j.otorri.2017.01.005%0Ahttp://sfx.library.uu.nl/utrechtsid=
EMBASE&issn=19883013&id=doi:10.1016%2Fj.otorri.2017.01.005&atitle=Findings+from+the - Bennett A, Banigo A, Lovegrove D, Wood M. Comparison of non soft tissue reduction techniques for BAHA insertion: Open approach vs. MIPS. In: OSSEO. Nijmegen; 2017.
- Johansson M, Holmberg M. Design and clinical evaluation of MIPS – A new perspective on tissue preservation. Oticon Med. 2014;1–12.
- Calon TGA, van Hoof M, van den Berge H, de Bruijn AJG, van Tongeren J, Hof JR, et al. Minimally Invasive Ponto Surgery compared to the linear incision technique without soft tissue reduction for bone conduction hearing implants: study protocol for a randomized controlled trial. Trials - Open Access. 2016;17(1):540.
- Calon ÃTGA, Johansson ML, Bruijn AJG De, Berge H Van Den, Wagenaar M, Eichhorn E, et al. Minimally Invasive Ponto Surgery Versus the Linear Incision Technique With Soft Tissue Preservation for Bone Conduction Hearing Implants : A Multicenter Randomized Controlled Trial. Otol Neurotol. 2018;39:882–93.

