Striking the Right Balance – Pediatric Vestibular Assessment: Considerations and Modifications
In this edition of “Striking the Right Balance,” Audiologists Curtis Wetmore and Kaitlin Harvey from the Centre for Advanced Hearing and Balance Testing and the Munk Hearing Centre at Toronto General Hospital, Toronto, ON, share their insight on considerations and modifications for pediatric vestibular assessments.
Michael Vekasi, MClSc, R.Aud, Aud(C), FAAA and Erica Zaia, MSc, RAUD are coordinating the “Striking the Right Balance,” feature which will cover the latest information on ‘all things vestibular.’ If you would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by simply emailing CAAvestibular@gmail.com to let us know you want to be a part. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
It is well documented that sensorineural hearing loss (SNHL) is the most common congenital sensory impairment, occurring in roughly 3 out of every 1000 children.1 Previous research demonstrates that more than half of children with profound SNHL have a related vestibular deficit, which makes vestibular impairment the most common associated feature of SNHL.2 For this reason, it is important for pediatric audiologists to consider a vestibular loss in addition to hearing loss. To identify and evaluate a vestibular impairment in children, the gold standard assessment is a battery of clinical tests that investigate semicircular canal and otolith function. However, these diagnostic tests can be difficult to complete, especially for young children. In this article, we will outline some considerations and modifications to help vestibular clinicians conduct pediatric assessments effectively without the use of specialized equipment. We will also highlight a straightforward vestibular screening assessment that can be used by any number of clinicians in the absence of diagnostic equipment.
Some housekeeping issues before we start: first, we will be discussing videonystagmography (VNG) and the video head impulse test (vHIT) as assessments of the semicircular canals, as well as cervical and ocular vestibular myogenic potentials (c/oVEMPs) as assessment of the otoliths. Rotational chair is no longer used at our clinic, so we will not be addressing this test; however, a rotational chair does serve as a reliable assessment of VOR function for young children.3 Secondly, at our clinic, we see children as young as 3 years old and we attempt all three vestibular tests (VNG, vHIT, c/oVEMPs) on each patient. Generally, more modifications are required for children below the age of 7. Finally, we will not be explaining the interpretation of vestibular tests in this article. Nevertheless, it is necessary to have a solid understanding of the interpretation of each specific test before conducting a vestibular assessment, especially when attempting to modify it.
VNG
Considerations
-
- VNG goggles - Small head size and difficulty keeping eyes open in the dark
- Tiny ear canals and possible occluding wax
- Otitis media with effusion (OME) and PE tubes
- Intimidating assessment
- Intolerance for warm water temperature (44℃)
Modifications
-
- Electronystagmography (ENG) is an excellent option for younger children. Head size is not an issue when using electrodes as opposed to VNG goggles. With ENG, all tests without fixation are completed with eyes closed as opposed to eyes open in the dark. This is much easier for children and you can get parents to help keep their child’s eyes shut.
- It is very important to complete thorough otoscopy before performing the caloric test. Cerumen management is needed if wax is present. If possible, it is helpful to have a different clinician perform the wax removal to not lose the child's trust. With tiny ear canals, it is important to note the direction and curvature of the ear canal to position the caloric nozzle correctly. If not, water might not enter the ear canal fully which can result in an artificially absent or small response.
- If PE tubes or a tympanic membrane (TM) perforation is present, it is very important to use air as opposed to water to stimulate the ear. Again, very thorough otoscopy (and tympanometry if needed) should be done to confirm TM status. A difference of TM status between ears could result in a false caloric weakness or bilaterally could mimic bilateral hypofunction. For this reason, special care and consideration need to be taken when analyzing the results of the caloric test in the presence of PE tubes/middle ear dysfunction.
- It is important to outline the caloric procedure with any patient, but this is especially true for younger children. This often means demonstrating how the water comes out of the irrigator and letting the child feel the temperature of the water (Doing this will result in many fewer tears and much better results in our experience). Children do best with the caloric test when you make it fun! For instance, refer to the test as the caloric coaster and explain that they might feel as though they are on a carnival ride. This helps to reduce the fear and anxiety that a child may experience before the test and ensures that you get a more accurate result or any result for that matter.
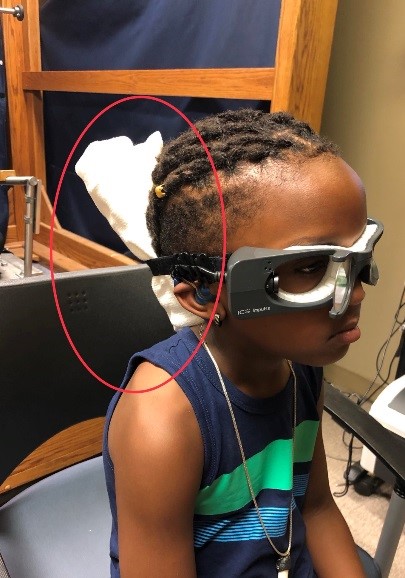
- A typical and well-known modification to the caloric test is the completion of a monothermal warm screen (44℃) if a patient is intolerant of the induced dizziness.3 Some young children, however, will be intolerant of the warm water. In this case, a cool screen (30℃) can be performed to get useful bilateral caloric information (Figure 1).

Figure 1. VNG goggles during the pediatric caloric test.
vHIT
Considerations
-
- vHIT goggles and small head size
- Sustained attention and intolerance of head movements
Modifications
-
- Properly fit vHIT goggles are one of the most important factors in obtaining an accurate vHIT study. Goggle slip produces an artificially high gain value and ultimately limits the diagnostic value of the test. Some vHIT systems have the option to use goggle cushions designed for smaller faces, even with this modification, the goggles might not be tight enough. To work around this issue, we use rolled towels and place them between the child’s head and the goggle strap to achieve a tighter fit (see Figure 2). Other centers report success with using foam as an intermediary device to improve the tightness of the goggles.
- The vHIT is a relatively quick test, taking roughly 10 minutes to perform. For younger children, 10 minutes might as well be an eternity for maintaining attention on a small affixed dot on the wall. An interesting visual stimulus will be a clinician’s best friend for obtaining a complete vHIT test. Fun stickers, a captivating video on a smartphone, or a toy held by a caregiver will help maintain a child’s gaze during head impulses. Bonus: the more interesting the visual stimuli the less the child will blink during the test! As a last resort, have a curious child watch their eye on the computer while performing head impulses. To help with the tolerance of the goggles and head movements, younger children can sit on a caregiver’s lap during the test while the clinician reaches around them to perform impulses.
c/oVEMPs
Considerations
-
- Limited attention span and inconsistent muscle contractions
- Conductive and mixed hearing loss
- Tiny ear canals and unsafe stimulus levels
Modifications
-
- VEMPs are a relatively quick and easy-to-perform test; however, obtaining reliable and repeatable waveforms relies on the child’s sustained attention and consistent muscle contraction. Children 7-8 years and older are usually able to perform the test with little modification. Kids under the age of 7 may require more modifications to obtain a full c/oVEMP test. To maintain the child’s attention and ensure sufficient and consistent muscle contraction, we often use an engaging visual stimulus (ideally a video on a smartphone) to prompt the child to perform the required eye gaze angle for oVEMPs and head position for cVEMPs.
- Normal middle ear function is required to obtain air conduction VEMP responses. Middle ear dysfunction is a common consideration in the pediatric population. Therefore, bone conduction VEMPs can be used to overcome any middle ear dysfunction and help obtain information about otolith function.
- The stimulus levels required to elicit air conduction VEMPs can be loud enough to be harmful to children. Smaller ear canal volume means that the sound levels reaching the cochlea are at least 3dB higher than in an adult ear. Additionally, reduced attention span and inconsistent muscle contraction means that it can take more trials to get a repeatable response. It is recommended that the air conduction stimulus be reduced from 125 dBSPL to 120 dBSPL for children with ear canal volume less than 0.8 mL.4 Evidence also suggests that a 750 Hz tone burst can achieve a similar VEMP response with less high-intensity sound exposure.4 Therefore, using 750 Hz in place of the typically used 500 Hz tone may be considered (Figures 3 and 4).

Pediatric Vestibular Screen
It is rare for audiologists to have access to the equipment necessary to carry out a full vestibular assessment, not to mention it can be a fairly challenging and time-intensive process. For this reason, Cushing and Papsin1 proposed a screening assessment that can be applied by any clinician. The screening assessment includes at least one of the following:
- Review of motor milestones
- Assessment of balance
- Assessment of horizontal canal function (if possible)
First, ask a caregiver about their child’s motor milestones (For example, ask how old the child was when they first sat unsupported or walked). Next, perform a quick assessment of the child’s balance by getting them to stand on one foot with their eyes open. This balance task is a component of the Bruininks Osetetsky Test of Motor Proficiency-2 (BOT2) and, along with one foot standing with eyes closed, has been demonstrated to be an effective screening tool for balance dysfunction in children.2 Table 1 outlines expected motor milestones and duration of expected one-foot standing by age.3–5
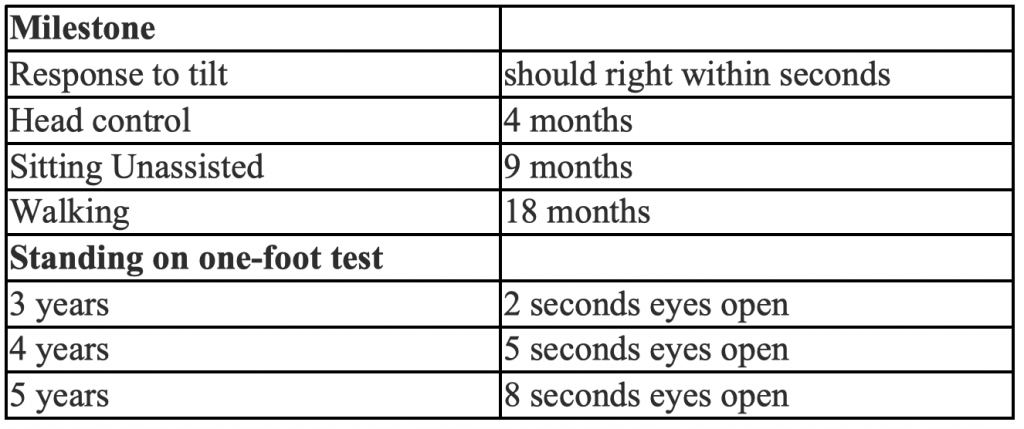
Adapted from McCaslin, 2016.5
Finally, if possible, look for horizontal canal function. For infants under the age of 6 months, this can be done easily by spinning them (and their caregiver) in a chair for a few rotations. Infants cannot suppress their VOR, so a healthy response will result in a child exhibiting post-rotary nystagmus. Which is to say that after the child stops spinning, nystagmus should be present with the fast phase directed away from the direction of the spinning.1 For older children, a bedside head impulse test can be performed to assess VOR function. We realize that a bedside VOR assessment may be beyond the comfort level and scope of many audiologists. In this case, the first two aspects of this screen may be the most feasible.
Information from any single step is useful in identifying a possible vestibular impairment.1 An abnormal finding during at least one of these steps in a child with SNHL should indicate a referral (or a recommendation for a referral) to an ENT for a vestibular evaluation.
Final Thoughts on Pediatric Vestibular Testing
Have prizes – one of the most useful pediatric tools that we have developed at our clinic is a treasure chest. Having stickers for a completed task or a prize at the end of the entire vestibular assessment can make a huge difference in patient cooperation.
Oh, and get to know Paw Patrol and the movie Frozen!
Acknowledgements
Thank you to Laurel Palmer (MSc, Reg. CASLPO) for providing input and helping edit this article.
References
- Cushing SL, Papsin BC. Cochlear implants and children with vestibular impairments. Semin Hear 2018;39(03):305–20
- Oyewumi K, Wolter NE, Heon E, et al. Using balance function to screen for vestibular impairment in children with sensorineural hearing loss and cochlear implants. Otol Neurol 2016;37:926–32.
- O’Reilly RC, Morlet T, Cushing SL. Manual of Pediatric Balance Disorders. San Diego: Plural Publishing; 2013.
- 4. Janky KL, Rodriguez AI. Quantitative vestibular function testing in the pediatric population. Semin Hear 2018;39(03):257–74
- McCaslin DL. Pediatric vestibular disorders and the role of the audiologist. AudiologyOnline 2016; article 17145. Retrieved from www.audiologyonline.com

