How Do Medical Masks Degrade Speech Reception?

Reprinted with permission from | May 2020 Hearing Review
Speech blocked by surgical masks becomes a more important issue in the Era of COVID-19
By Alexander Goldin, PhD, Barbara Weinstein, PhD, and Nimrod Shiman
The data show that each type of medical mask in this study essentially functioned as a low-pass acoustic filter for speech, attenuating the high frequencies (2000-7000 Hz) spoken by the wearer by 3 to 4 dB for a simple medical mask and close to 12 dB for the N95 masks. This means the speech quality degradation, in combination with room noise/reverberation and the absence of visual cues, renders speech close to unintelligible for many patients with hearing loss.
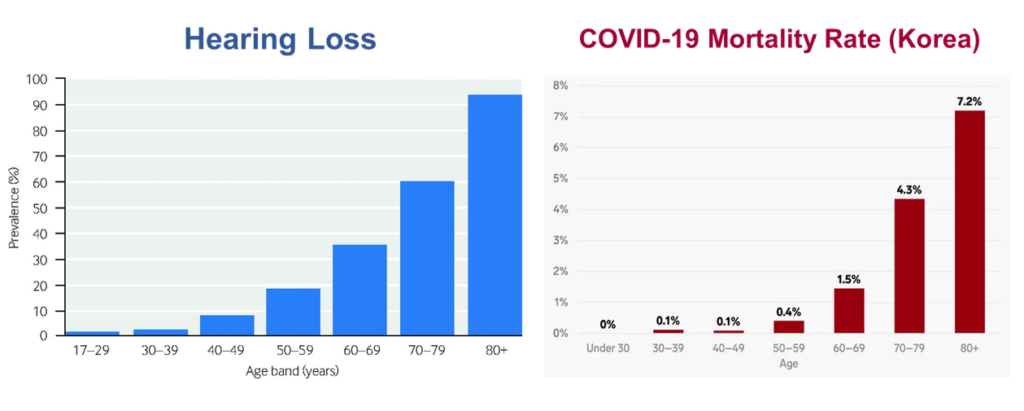
The pervasive toll of hearing loss on clinician-patient communication has become magnified with advent of the coronavirus (COVID-19 virus). In fact, as is shown in Figure 1, the trajectory of hearing loss and the infection fatality by age distribution tell a very important story—one most of us may not have as of yet considered. In short, hospitals, emergency departments, and intensive care units (ICUs) are now flooded with older adults with the COVID-19 virus. Many of the people who have fallen victim to the virus have hearing loss, are unaccompanied by family members, are frail, have multiple chronic conditions and are likely without hearing assistance. Estimates of the infection fatality ratio in the oldest age group (≥80 years) ranges from 8% to 36%, and sex-based data suggest that older men generally fare worse than elderly women in their ability to combat the virus.
We are all aware that a cornerstone of patient safety and quality healthcare is effective communication which allows patients to participate fully in their care. For communication to be effective, it must take place in a manner appropriate to one’s age, understanding, and communication abilities. Furthermore, medical information, when provided, must be complete, accurate, timely, unambiguous, and understood by the patient.1 It is well established that when patients can hear and understand the healthcare provider, they are much more likely to be compliant and follow physician recommendations and have their medical needs optimally met.
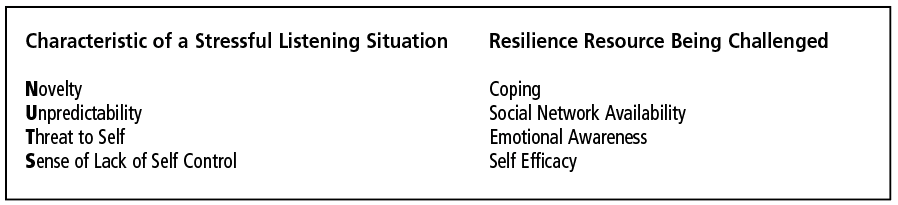
Since social, psychological, and environmental factors also influence speech understanding especially in hospital settings, older adults are at a great disadvantage in what is now the new normal.2 As is evident from Table 1, the hospital is a very stressful listening situation.3 It is novel (N), unpredictable (U), threatening (T), and the skill set (S) to cope tends to be compromised. Add to this the fact that clinical care is now often being delivered in settings which are extremely noisy and distracting—replete with alarms beeping and ongoing competing conversations between patients and providers.
Further, the struggle to understand speech for persons with hearing loss is now exacerbated by the masks which are a necessity to help minimize the spread of the virus. These masks pose two obvious problems for patients with hearing loss: 1) the patient cannot gain any cues from lipreading, and 2) the voice of the healthcare provider is attenuated and distorted. This brief study looks at the latter problem.
How Does a Medical Mask Impact the Speech Signal?
We decided to quantify the potential challenge to a listener’s comprehension at the acoustic level posed by the variety of masks being worn by healthcare providers. The Alango Technologies team based in Israel measured voice samples in an anechoic chamber as a function of the type of mask being worn (Figure 2). A GRAS head and torso simulator was used to play white noise though the artificial mouth, and the output acoustic signal was measured by a microphone at 2 meters distance.
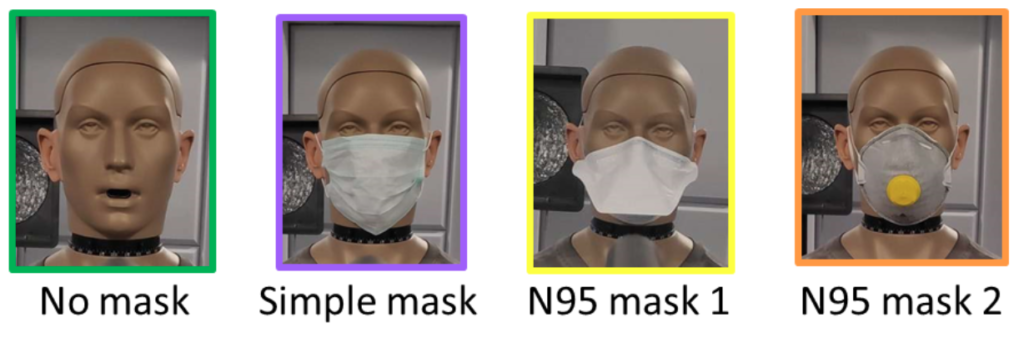
Figure 3 summarizes the measurements. Only the differences between the green (no mask curve) and the others are important. Our findings were not unexpected but were unsettling. The data show that each mask essentially serves as a low-pass filter, attenuating the high frequencies (2000-7000 Hz) spoken by the wearer, with the decibel (dB) level of attenuation ranging from 3 to 4 dB for a simple medical mask and close to 12 dB for the N95 masks.

In short, the speech quality degradation, in combination with room noise/reverberation and the absence of visual cues, renders speech close to unintelligible for many.
Recommendations for Caregivers
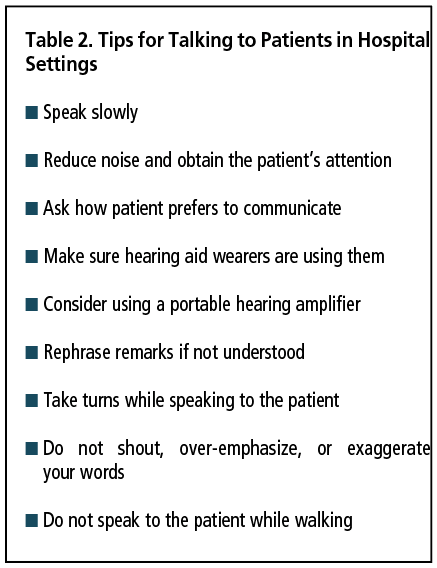
We include in Table 2 a list of universal communication precautions we have created, and encourage each of you to share with your patients and colleagues in healthcare settings. For those patients who do not have a hearing aid or assistive listening device, we also strongly recommend use of commercially available and affordable voice enhancement technologies (eg, Alango BeHear ACCESS or BeHear NOW, Williams Sound Pocket Talker, etc) or hearing apps on smartphones (eg, Jacoti ListenApp) to help optimize speech understanding.
In the words of Helen Keller, it is our firm belief that “Alone we can do so little; together we can do so much.”
References
- Blustein J, Wallhagen MI, Weinstein BE, Chodosh J. Time to take hearing loss seriously. Joint Commission Jour on Qual and Patient Safety. 2020;46:53-58.
- Peelle JE. Listening effort: How the cognitive consequences of acoustic challenge are reflected in brain and behavior. Ear Hear. 2018;39(2):204-214.
- Pichora-Fuller MK. How social psychological factors may modulate auditory and cognitive functioning during listening. Ear Hear. 2016;37:92S-100S.

