Canadian Hearing Health and Research Strategy – A Call for Action!
Present and future challenges for the mission and practice of Audiology were highlighted at the 2019 Speech-Language & Audiology Canada event that took place in Montreal in May. In the hallway of the conference venue, participants were invited to post on large panels their thoughts concerning Canada’s response to the World Health Organization (WHO)’s call to develop and implement a national hearing strategy. I was impressed by the number of postings that emphasized a role for research in such terms as: “dedicated research funding,” “bridge clinic and research to inform a strategy,” “we need the right data -- Canadian data!” “consistent funding by agencies,” and “improve funding.”
The Upcoming Challenge of Hearing Loss, Tinnitus, and Hyperacusis
Hearing loss is the fourth leading cause of disability, and it is projected that its global prevalence will increase from 6.12% in 2018 to 9.6% by 2030.1 Indeed, with the current demographic trends, namely, a growing and aging population, it is to be expected that the number of people with hearing loss will continue to increase. There is also a concern about the rising exposure to loud sound spurred by technological advances in recreational settings and the ensuing risk of developing irreversible hearing loss among teenagers and young adults.2 In this context, there is certainty that all countries, including Canada, will soon be facing a serious challenge regarding hearing loss.
The concern about the escalation of hearing loss can be extended to tinnitus, since hearing loss is the most important risk factor for tinnitus. In a recently published Statistics Canada report of tinnitus data from the Canadian Health Measures Survey (CHMS)3 [of note: the right data -- Canadian data!], it was estimated that 37% of Canadians (aged 19 to 79) had experienced in the past year tinnitus described as “the presence of hissing, buzzing, ringing, rushing or roaring sounds in [the] ears when there is no other sound around”, without specifically referring to chronic tinnitus. Moreover, tinnitus was deemed bothersome in 7% of the population. The striking news was that individuals aged 19 to 29 were significantly more likely to have experienced past-year tinnitus (46%) than those aged 30 to 49 (33%) or 50 to 70 (35%). This is in stark contrast with past studies in which prevalence was higher among older individuals. Such high prevalence in the younger age group was associated with the use of audio devices and exposure to loud music in this age group. Comorbidities of tinnitus were self-reported mental health vulnerability, mood disorder, a weak sense of community belonging, high daily stress and sleep of poor quality, all of which undoubtedly increase the economic burden of tinnitus above and beyond hearing loss.
There are several ways to address the growing prevalence of hearing loss, for instance via preventative actions for infections, noise exposure, ototoxic medications, and by developing policies to increase awareness about hearing care and improve access to hearing health technology and services. However, fundamental to any health issue is the core building of knowledge through research. It has been suggested that the delay for knowledge transfer from bench to bedside is 17 years.4 One can speculate that the closer the research to a given population, the narrower the gap between bench and bedside, and the fastest the benefit from the research outcomes. In view of the huge challenge that awaits Canada, our attention turns to the ongoing hearing research in our country.
Funding for Hearing Research in Canada
The main public funding organization supporting health research is the Canadian Institutes of Health Research (CIHR). As stated in the CIHR Act, CIHR's mandate is to "excel, according to internationally accepted standards of scientific excellence, in the creation of new knowledge and its translation into improved health for Canadians, more effective health services and products and a strengthened Canadian health care system" (http://www.cihr-irsc.gc.ca/e/7263.html).
CIHR is divided into 13 virtual Institutes, each of which is dedicated to a specific area of focus:
Aging, Cancer Research, Circulatory and Respiratory Health, Gender and Health, Genetics, Health Services and Policy Research, Human Development, Child and Youth Health, Indigenous People’s Health, Infection and Immunity, Musculoskeletal Health and Arthritis, Neurosciences, Mental Health and Addiction, Nutrition, Metabolism and Diabetes, and Population and Public Health. Each year CIHR contributes 1 billion dollars to support health research.
What portion of this billion dollar funding is devoted to one of the most important challenges of the future according to the WHO, namely hearing loss and tinnitus?
To answer this question, I searched the CIHR Funding decision database, selecting the five following topics that can be deemed important in terms of burden of disease: (i) hearing, (ii) vision (pertaining to the sensory system), (iii) diabetes, (iv) autism (chronic conditions), and (v) depression (a prevalent mental disorder). For each topic, searches were conducted using the following keywords: (i) deafness, hearing loss, tinnitus, hearing, auditory, (ii) vision, vision loss, visual, (iii) diabetes, diabetic, (iv) autism, autistic, and (v) depression, depressive. Except for keywords, topics were searched using identical criteria: (1) funding for the specific period of 2019-2020 (includes grants terminating at the end of June 2019 as well as ongoing ones beginning in January and April 2019); (2) Grants only (funding direct research costs, excluding personnel awards for salary support); (3) Operating grants (under Program Family, e.g., not Equipment grant, Randomized Control Trials, Salary Programs, etc; (4) All programs (including any type of program, i.e. the ones in criteria 2 and 3 as well as team grants, networks, priority funding, Institute, etc., for the widest possible search); (5) Institute (any of the 13 CIHR sectorial Institutes).
All abstracts were reviewed to ensure that the grant proposal identified by keywords belonged to the searched research topic. Figure 1 shows the overall number of active grants per topic and Figure 2 shows the total amount of funding per topic. The total number of grants for the five selected topics was 605, which amounted to $114,139,574 in funding. Hearing resulted in 11 hits (1.8% of the total number of grants, and 0.99% of the total funding), followed by Vision (4.6% of grants, 4% of total funding), Autism (13.7% of grants, 15.6% of total funding), Depression (29.1% of grants, 24.7% of total funding), and Diabetes (50.7% of grants, 54.5% of total funding). Of note, only a single grant (which happened to be in its final year of funding) focused on tinnitus (animal model). It is also interesting to note that Diabetes research, which is nested within an Institute of its own, received the lion’s share among the selected topics. Finally, Figure 3 shows the average funding per grant. Again, Hearing research received the smallest share ($103,223), followed by Depression ($160,506), Vision ($167,935), Diabetes ($202,790), and Autism ($214,415).
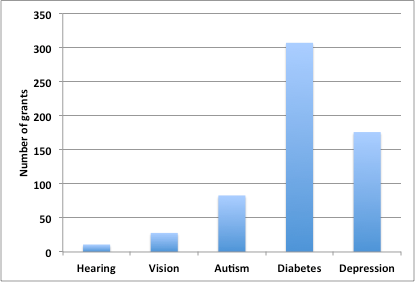
Figure 1. Number of active (2019-2020) CIHR grants for selected health topics, all programs.
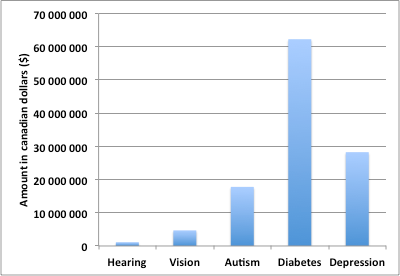
Figure 2. Total funding for active CIHR grants.
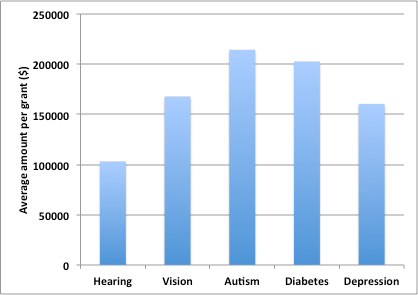
Figure 3. Average funding per active grant.
Funding for Hearing Research in the United States of America (USA)
As I was writing this paper, a study on funding of hearing loss research in the USA, with similar goals but using a slightly different approach, was published.5 The largest public funding system for health research is the National Institutes of Health, on which CIHR was modeled, consisting of 21 virtual Institutes, some of which are similar to one or the other of the 13 CIHR Institutes. However, in the context of this paper, a crucial difference is that the NIH includes a National Institute on Deafness and Other Communication Disorders (NIDCD), for which there is no equivalent among the CIHR institutes. In the USA, most, if not all, hearing research is nested within that the NIDCD.
In Blustein, the NIH RePORTER database was searched for projects funded in fiscal year 2017.6 Despite the $202 million dollars devoted in 2017 to hearing loss research (compared to the $1.1 million for hearing research in Canada, such as 202 times less funding for a 9 times smaller population), this field was felt by the authors to be relatively underfunded relative to the disease burden measured in DALYs that it represents. The Disability-adjusted life-years (DALY) index is used to quantify years lost of healthy life, or in other words “the gap between current health status and an ideal health situation where the entire population lives to an advanced age, free of disease and disability” (WHO, accessed June 2019). Since DALY allows comparisons between the burden imposed by different diseases, it was noted that, while hearing loss came as 10th in DALYs among the 30 most common conditions in the USA, it only ranked 20th in terms of funding.
So, Where To Go from Here?
Obviously, researchers working in the field of hearing are much more numerous than could be retraced here in the CIHR database. Fortunately, enough, researchers have – to a variable degree – access to some funding from other sources through local or provincial public agencies, private foundations, and companies. But should Canada step up, develop and implement a national hearing health strategy, as called for by the WHO, a consistent and serious hearing research component should certainly be part of it. With the looming challenge posed by hearing disorders, it is time to open a conversation concerning the opportunity of adding an Institute on Hearing and Communication Disorders to the existing CIHR structure, so that all researchers working in the hearing field can speak with a united voice.
References
- World Health Organization. Addressing the rising prevalence of hearing loss. 2018; Geneva.
- World Health Organization-International Technical Union (WTO-ITU), Safe listening devices and systems: a WHO-ITU standard; 2019.
- Ramage-Morin PL., et al., Tinnitus in Canada. Health Rep 2019; 30(3):3–11.
- Morris ZS, Wooding S, and Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med 2011;104(12):510–20.
- Blustein J., National Institutes of Health Funding for Hearing Loss Research. JAMA Otolaryngol Head Neck Surg 2019.
- World Health Organization.; Available from: https://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/. Accessed June 2019.

