Thirty Years of The Neurophysiological Model of Tinnitus and Tinnitus Retraining Therapy (TRT)
Thirty-five years ago, research, existing models and treatment approaches for tinnitus were focused on the periphery of the auditory system, mainly at the cochlea. Analysis of tinnitus patients' reactions and reported complaints (e.g., sleep problems, increased stress level, anxiety, depression, inability to enjoy a variety of activities in life, inability to concentrate and focus attention) strongly indicated involvement of other systems in the brain, particularly the limbic and autonomic nervous systems in the clinically-significant tinnitus. This observation created the basis for the neurophysiological model of tinnitus with the main assumption that in clinically-significant tinnitus (i.e., tinnitus which is bothersome enough for a person to seek help) other systems in the brain outside the auditory system are involved.1,2
The model stressed the difference between "experiencing" tinnitus versus "suffering" because of it. At the time, it was assumed that patients must be aware of tinnitus to suffer because of it. Even though about 80% of the people perceiving tinnitus did not have problems with it, research continued to focus on mechanisms of tinnitus perception and not on mechanisms which were responsible for tinnitus being the problem. Last but not least, high comorbidity of decreased sound tolerance (DST - a subject exhibiting negative reactions to a sound which would not be a problem for an average listener) has not been sufficiently recognized and thus its impact at proper modification of a therapeutic approach has not been appreciated.
To facilitate visualization of basic concepts involved with the neurophysiological model, a simple block diagram has been proposed (Figure 1A). There are two loops in the network of the interconnections of the main systems involved in the processing of tinnitus signal - a high loop involving cognitive processing (Figure 1B) and a low loop involving subconscious processing (Figure 1C). Analysis of results from over 300 sequential patients revealed that the low, subconscious loop is dominant in chronic tinnitus, while the high loop is particularly significant during the initial period of developing bothersome tinnitus.
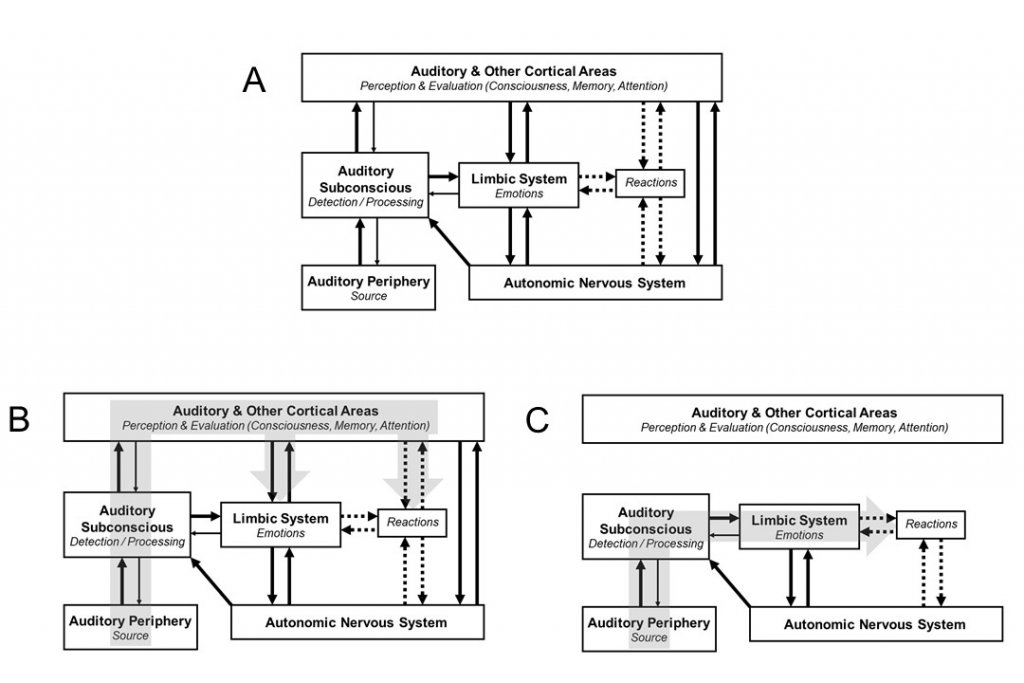
Figure 1. The block diagram of the Neurophysiological Model of Tinnitus. (A)Whole network. (B) Upper loop. (C) Lower loop.
Connections within the neuronal networks that are implicated in yielding the adverse effects of tinnitus are governed by the principles of conditioned reflexes. Suffering individuals develop an automatic negative response to tinnitus signal (i.e., neuronal activity perceived as tinnitus) in spite of the fact that this activity is, in reality, ordinary stimulus, which does not induce reactions in most people who consequently just experience it. On the basis of the neurophysiological model of tinnitus the treatment was developed (Tinnitus Retraining Therapy - TRT), which aims at the retraining of the connections of the auditory system with other systems in the brain, effectively to break these connections and achieve habituation (removal) of negative reactions to tinnitus.2,4 Brain plasticity is crucial in order for retraining and habituation to occur. Habituation of perception occurs automatically once a sufficient level of habituation of reactions is achieved. (Figure 2). At the end of the TRT treatment patients still perceive tinnitus at a smaller fraction of the time and no longer are affected by tinnitus. Consequently, patients can return to their normal lives. TRT consists of two components which have to be implemented simultaneously: retraining counseling and sound therapy.
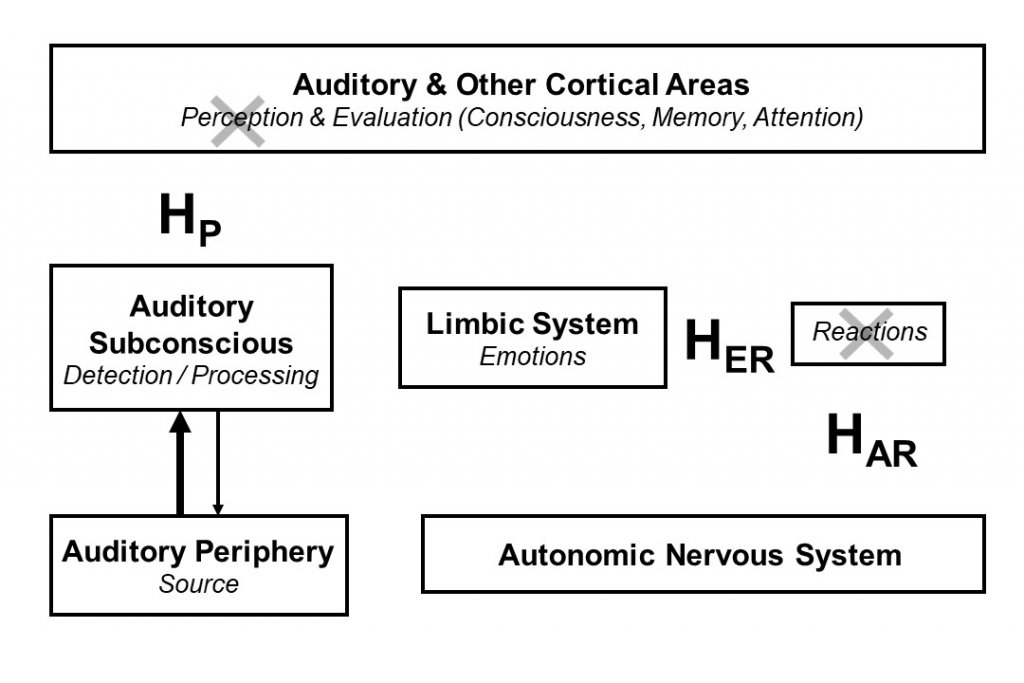
Figure 2. Goals of TRT: habituation of tinnitus. HER - habituation of emotional reactions. HAR - habituation of autonomic reactions. HP - habituation of tinnitus perception.
Tinnitus frequently coexists with other problems of the auditory system, e.g., decreased sound tolerance, hearing loss, tensor tympani syndrome. It is imperative to consider these problems to ensure a successful outcome of tinnitus treatment. Note that TRT is not aimed at changing tinnitus signal but at changing functional connections which are responsible for the activating by this signal non-auditory parts of the brain. Consequently, the etiology of tinnitus is irrelevant, and TRT can be used to treat tinnitus of any origin and somatosounds.
Basic stages of TRT implementation have remained the same over the past 30 years and include4:
- Detailed initial interview and history of the problems. Selected validated questionnaires are used as a part of the process to assess the initial state, determine the progress of the treatment, and evaluate the final outcome.
- Audiological evaluation with extended up to 12 kHz audiogram; measurements of Distortion Product Otoacoustic Emission - particularly useful in case of tinnitus with normal hearing; Loudness Discomfort Levels are used as a part of an evaluation of DST.
- Diagnoses, establishing a treatment plan appropriate to the specific characterization of a patient.
- Retraining counseling (teaching session, influencing directly high loop) aiming at reclassification of tinnitus to a category of neutral stimuli and demystifying tinnitus by providing information appropriate to a given patient which would be helpful to neutralize the patient’s negative associations and misconceptions. The neurophysiological model of tinnitus is discussed in simple language to provide a new frame of reference for tinnitus. A detailed discussion of realistic goals to achieve habituation is a part of counseling (i.e., tinnitus / decreased sound tolerance stop having an impact on patient's life, tinnitus signal might remain unchanged but will not induce negative reactions (habituation-based treatment), TRT is not "a quick fix" and retraining takes time).
- Sound Therapy (influencing all systems, but the principal effect is its impact at the low loop) with the main goal decreasing the contrast between tinnitus and background neuronal activity effectively weakening it (Figure 3), and reducing abnormal gain in the auditory system (particularly important in hyperacusis). It is crucial to understand that sound is important and not a particular device. However, ear-level instruments are very helpful in the implementation of sound therapy, helps patient compliance and crucial for patients with hearing loss where additional use of hearing aids is suggested (reduced strain to hear and provide auditory stimulation).
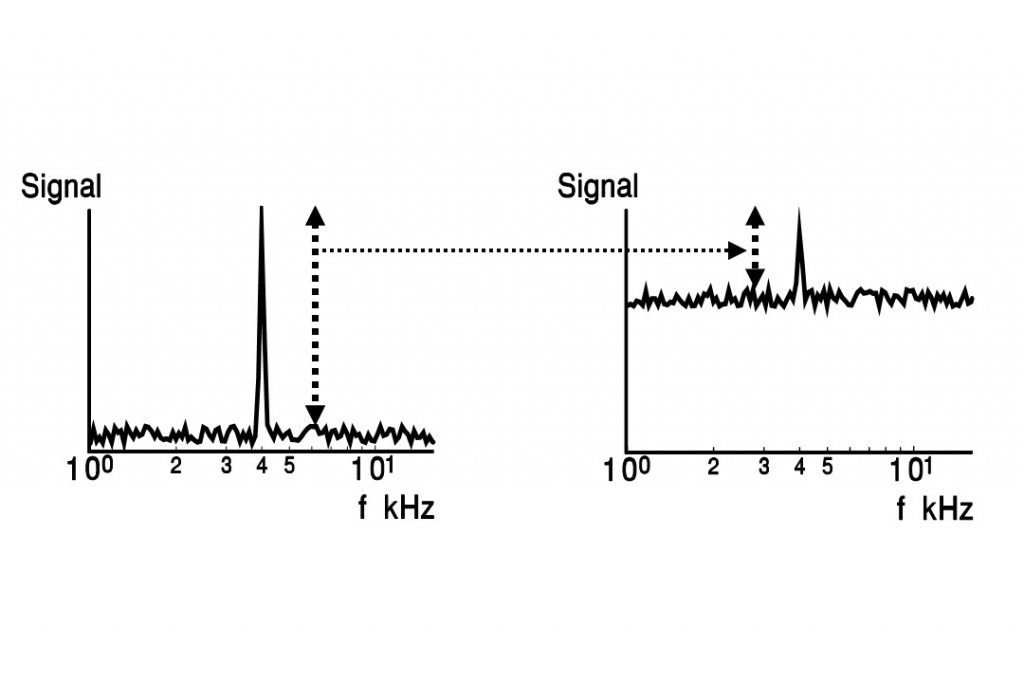
Figure 3. The strength of a tinnitus (or sound-evoked) signal depends on its difference from background neuronal activity, which is influenced by sound environment.
- Follow-up visits are particularly important at the beginning of treatment. They focus on continued counseling and answering patients’ questions and concerns. Once the process of habituation is initiated and the connections between auditory and other systems are weakened, less frequent follow-up visits are necessary. The end of the treatment is determined by the patient, but we insist on a continuation of the treatment for at least nine months to prevent relapse.
While the principles on which TRT is based remain the same, a number of modifications have been introduced in the TRT implementation over the last 30 years. Major changes include:
- The recognition of the importance of conditioned reflexes and the dominant role of the subconscious pathways (the low loop) in tinnitus-related problems, leading to extensive modifications of counseling and aspects of sound therapy.
- The refinement of sound therapy incorporating specific instructions related to setting the sound level. It has been always postulated in TRT that sound used as a part of sound therapy should not evoke annoyance, discomfort or problems because of any reason, as it would cause negative excitation of the limbic system and work against habituation to occur. However, only after introducing Real Ear Measurements (REM) of the sound level generated by sound generators as used by patient revealed significant issue - the "mixing point" turned out to be unrealistic for the majority of patients as they first experienced annoyance caused by the sound while trying to reach "mixing point." Consequently, since 2002,4,5 the sound setting of devices used in TRT was updated from the recommendation of reaching the "mixing point" to treat it as a potential goal. It is nice to reach, but not recommended as necessary. On the other hand, REM measurements indicated a significant number of patients uses a very weak sound level below 6 dB SL, which is in the range of stochastic resonance and may actually enhance their tinnitus!5,6
- The recognition of the existence of misophonia (i.e., negative reactions to a specific, for a given patient, patterns of sound), as a separate part of DST and the necessity for its concurrent treatment with specific protocols.
- Higher stress on hearing rehabilitation and an expanded high-frequency range of amplification.
New advances in hearing aids and a broad variety of combination instruments made a significant change in facilitating the tinnitus treatment. Overall, the change in TRT outcome relates to the shorter time needed to see clear improvement (reduced from 1 year to 1 month) and the shorter time of treatment (from 18–24 months to 9–18 months).
Over 150 papers on Medline are selected with “Tinnitus Retraining Therapy” as a key term. Many of papers describe the clinical outcome of TRT with reports on average about 80% of patients showing significant improvement. There are some clinical studies on TRT reporting various conclusions from highly positive to not supportive.7–10
Without detailed discussion on specific study paradigms, below there is a list of potential reasons why some of them lead to conflicting conclusions not matching the outcome of the majority of clinical reports.
- The choice of tool for the primary outcome measure might not reflect patients ’ problems, e.g., using the change of quality of life as the primary outcome measure.
- Studies do not exclude subjects with hyperacusis or misophonia, and they are not treating DST - a condition which is essential for treating patients with tinnitus and DST.
- Sound therapy in TRT is not assured by the use of ear-level instruments, which although might be useful but not absolutely necessary.
- TRT always utilizes specific counseling and sound therapy working inseparably together. This condition is necessary, as the main goal of TRT is to retrain subconsciously conditioned reflexes linking the auditory system with other systems in the brain. To create a conditioned reflex it is necessary for sensory stimulus (e.g., tinnitus) and reinforcement (e.g., negative activation of the autonomic nervous system) to occur at the same time. Presenting independently sound and reinforcement will not result in creating a conditioned reflex. Exactly the same principle applies when an attempt is made to extinguish/retrain reflex - sound and changed reinforcement has to happen simultaneously. Therefore, TRT requires the simultaneous application of both counseling and sound therapy.
- The setting parameters of instruments and instructions on how to use them during treatment might be incorrect and reflect a long-abandoned method, e.g., it is not recommended to reach the "mixing point" for the past 20 years, yet some studies continue using this old recommendation; the need to be above the range of stochastic resonance (6 dB SL) and necessity for patient to have possibility of changing sound level from sound generators or sound generators part of combination instruments for at least 20 dB are frequently ignored.
- A study does not assess long-term stable outcomes.
- Statistically significant improvement should not be equated with clinically significant improvement
There is no one universally accepted method to help tinnitus patients; nevertheless, with specific adjustments to cultural differences and health systems, TRT seems to help patients in many countries around the world. If nothing else, the neurophysiological model of tinnitus and its implementation in TRT offers a philosophy and overall guidance for tinnitus habituation-based treatments.
References
- Jastreboff PJ. Phantom auditory perception (Tinnitus): mechanisms of generation and perception. Neurosci Res 1990;8:221–54.
- Jastreboff PJ, and Jastreboff MM. Tinnitus and decreased sound tolerance. In: Ballenger's Otorhinolaryngology Head and Neck Surgery. 18th edition. eds P.A. Wackym, and J.B. Snow, Jr., PMPH-USA, Ch31; 2018.
- Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. Cambridge University Press; 2004.
- Jastreboff PJ, Jastreboff MM, and Payne L. Sound levels used in Tinnitus Retraining Therapy. 7th International Tinnitus Seminar, Fremantle, Western Australia; 2002.
- Jastreboff PJ, Jastreboff MM. Tinnitus retraining therapy for patients with tinnitus and decreased sound tolerance. Otolaryngol Clin North Am 2003;36:321–36.
- Jastreboff PJ, Jastreboff MM. Tinnitus Retraining Therapy. In: Tinnitus: Theory and Management, ed. J.B. Snow, Jr. BC Decker, Hamilton, London; 2004.
- Henry JA, Schechter MA, Zaugg TL et al. Outcomes of clinical trial: tinnitus masking versus tinnitus retraining therapy. J Am Acad Audiol 2006;17(2):104–32.
- Bauer CA, Berry JL, Brozoski TJ. The effect of tinnitus retraining therapy on chronic tinnitus: A controlled trial. Laryngoscope Investig Otolaryngol 2017 May 28;2(4):166–77. doi: 10.1002/lio2.76. eCollection 2017 Aug. PMID: 28894836
- Forti S, Costanzo S, Crocetti A, Pignataro L, Del BL, Ambrosetti U. Are results of tinnitus retraining therapy maintained over time? 18-month follow-up after completion of therapy. Audiol Neurootol 2009;14(5):286–89.
- Tinnitus Retraining Therapy Trial Research Group, Scherer RW, Formby C. Effect of Tinnitus Retraining Therapy vs Standard of Care on Tinnitus-Related Quality of Life: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg 2019 May 23. doi: 10.1001/jamaoto.2019.0821. [Epub ahead of print].

