Tinnitus and Sound Tolerance Program at the University of Montreal’s Clinic of Speech-Language Pathology and Audiology
The University of Montreal's speech-language pathology and audiology clinic was established in 2009. In 2015, a tinnitus and sound tolerance problem program was created to offer services to patients with tinnitus and/or sound tolerance problems in the Montreal area. The audiologists working at the clinic, including the current authors, created a clinical protocol to improve the care of those patients. This protocol was also intended with the philosophy of providing an evidence-based approach of tinnitus and sound-tolerance care to students from the École d'orthophonie et d'audiologie (School of speech-language pathology and audiology). Indeed, a lot of students had their placement at the clinic where they could apply the knowledge acquired in their 45 hours of tinnitus and sound tolerance problem classes.
This protocol was influenced by different evidence-based protocols and guidelines from around the world for treating patients with tinnitus and sound tolerance problem and adapted to our specific environment. The program consists of 9 steps:
- Pre-appointment gathering of information
- Triage
- Questionnaires in the waiting room
- Case history
- Evaluation
- Classification
- Determination of the intervention plan and objectives
- Intervention
- Reference to other health professionals
The next sections will briefly describe every step of this clinical protocol.
1. Pre-Appointment Gathering of Information
At the clinic, as soon as a request for tinnitus and/or sound tolerance problem is receive we send the Tinnitus Functional Index questionnaire1 and the GUF questionnaire by e-mail or by regular mail to the patient.2 We ask them to fill it out and send them back to us rapidly.
2. Triage
Upon reception of the questionnaires, an audiologist or an audiology student analyses both questionnaires. As per the results on the Tinnitus Functional Index and the GUF questionnaire, patients are assigned to one out of five possible levels of a handicap for each of the disorders (See Table 1 for tinnitus and Table 2 for sound tolerance problem).
Table 1. Degree of Handicap as Classified by the TFI Score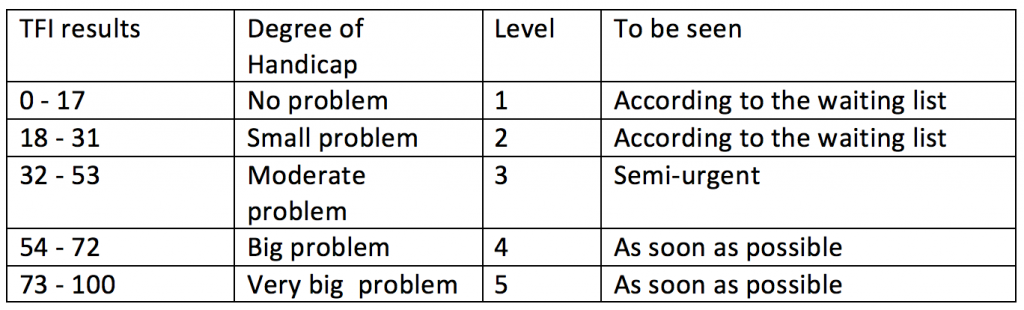
TFI = Tinnitus Functional Index
Table 2. Degree of Handicap as Classified by the GUF Score.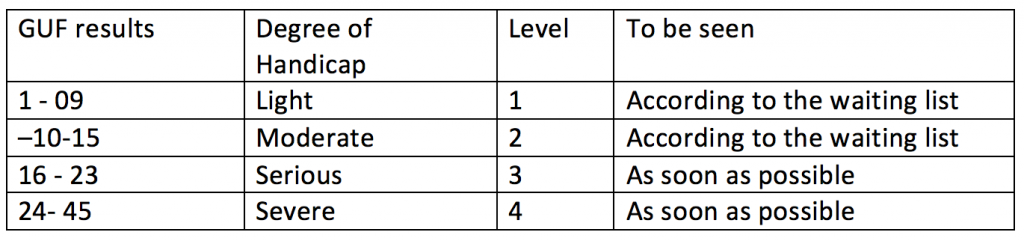
GUF = Geräuschüberempfindlichkeit (hypersensitivity to noise).
This triage allows patients that are severely or very severely handicapped by their tinnitus and/or sound tolerance problem to be seen in priority in order to access individualized care as early as possible.
For example, a case of 5 or 4 total score will be seen as a priority if possible in-within 2 weeks after the reception of the questionnaires while a patient who rate 1 or 2 will be seen according to the waiting list.
The TFI questionnaire analysis also includes the examination of the results for each subscale (Intrusion, Sense of Control, Cognitive, Sleep, Auditory, Relaxation, Quality of life and Emotional) to determine which subscale gives the highest result and indicate the domain most negatively affected by tinnitus. This information is useful for the case history and counselling.
This allows us to know at what level the patient is the most affected: sleep, loss of sense of control, or else.
3. Questionnaires in the Waiting Room
Upon arrival of the patient in the clinic, we asked that any patients who are classified in having a level of handicap of ≥ 3 on the TFI and/or the GUF questionnaire, fill out the following additional questionnaires in the waiting room: the PHQ-9 to screen any signs of depression,3 the GAD-7 to screen signs of anxiety and the Canadian Mental Health Association to screen the level of stress (https://cmha.ca/fr/evaluateur-de-sante-mentale).4 The information retrieved from these questionnaires guides us on the need to refer patients with high score to mental health provider for psychological support. It is well known that a higher handicap of tinnitus and/or sound tolerance problem is a link to a higher prevalence of other comorbidities such as depression, anxiety and stress.5,6
4. Case History
To guide the students with the case history, we have created a 7-page case history for tinnitus and a 4-page case history for sound tolerance problem that we asked the patient to fill. The information retrieved for the tinnitus part includes the description of the tinnitus, the factors that trigger or exacerbate the tinnitus (emotional events, temporomandibular joint disorders, neck pain, etc.), the perspective of the patient on their reaction to the tinnitus and their health condition and medications uptake. When we complete our case history, we take into account the results of each subscale of the TFI. As an example, we will not question the patient about the quality of his sleep if the result on this subscale of the TFI is very low. For the sound tolerance problem part, the questions focus mainly on which sounds are problematic, on the use of hearing protection and on the presence of other sound-induced sensations like pain. This questionnaire is available to any clinicians who would like to have a copy upon request to the authors.
5. Evaluation
For each patient, a complete hearing evaluation is accomplished including otoacoustic emissions with 8 measures per octave. We also test the extended high frequencies up to 16 000 Hz. Tinnitus psychoacoustic evaluation (loudness, pitch, minimum masking level and residual inhabitation) is considered optional: If the patient consults in audiology as part of a legal case (VAC workers compensation board, legal matter) or if a sound generator or a combination of hearing aid and sound generator is chosen as the intervention, only then, those psychoacoustic evaluations are performed. Otherwise, they are not routinely performed with the exception of when patients asked the test to be performed. Indeed, we asked the patient if they would like to know the intensity and pitch of the tinnitus before the clinical evaluation, after the case history.
If we think that the patient presents somatic tinnitus related to TMJ or neck problems, an isometric evaluation is performed base on a protocol developed at the to determine if the patient should be referred to a physiotherapist or a dentist for treatment.7
6. Classification
Patients are then categorized following the classification of Jastreboff and Jastreboff (see Table 3).8 This classification is different than the one performed for the triage. Indeed, the triage classification allowed us to determine the degree of disability of the tinnitus/ sound tolerance problem and was used to prioritize patients with urgent needs. The second classification is used to determine at what level we must intervene. Does the patient present only a problem of tinnitus or a combination of both tinnitus and sound tolerance problem? Does the patient have hearing loss or not? The recommended treatment will change depending on this classification. As such, basic counselling could be recommended for patient category 1 and more advanced intervention with the use of amplification for patient category 2.
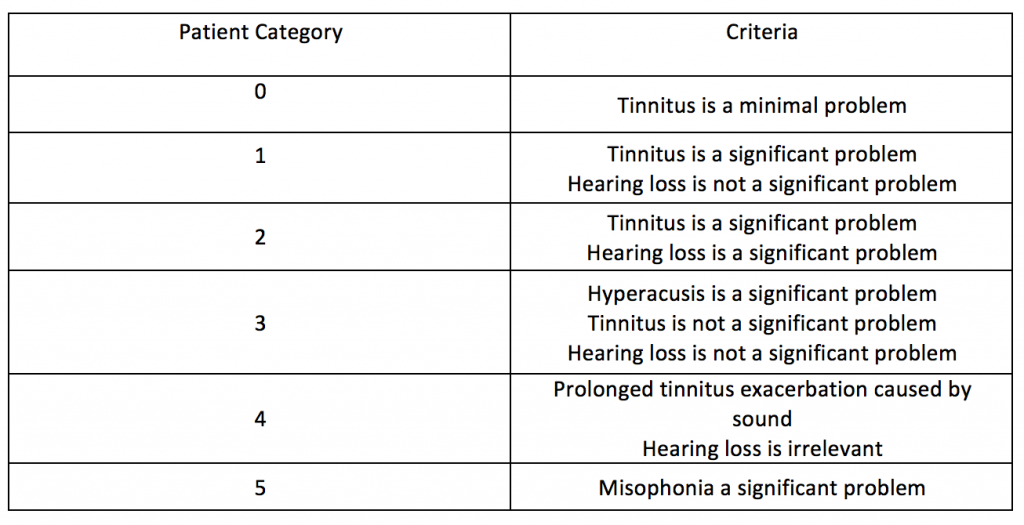
Table 3. Categories of Tinnitus and Hyperacusis Patients as per Jastreboff and Jastreboff8
7. Determination of the Intervention Plan
In collaboration with the patient, the students, and the clinical supervisor, the information gathered before and during the evaluation is analyzed and an intervention plan is elaborated. The objectives of the intervention plan are decided in collaboration with the patient and written on the COSIT form.9 The COSIT is a form similar to the regular COSI but applies to tinnitus. It is a tool used to make a decision relative to the objectives of the rehabilitation plan. As an example, the objectives could be: reduce tinnitus effect on wellbeing and depression, improve sleep and to reduce or remove the annoyance of tinnitus.
Potential Components of the Intervention Plan
Based on the objectives, we determine in collaboration with the patient and a decision aid tool component of the intervention plan. A decision aid tool is used to present different intervention options for the patient with the advantages and disadvantages of each intervention. The patient is thus involved in the choice of his treatment. This is part of the patient-centred approach. In addition, all patients are informed about a support group call Acouphènes Québec.
An example of a decision aid tool is available online at: https://www.tinnitus.org.uk/Handlers/Download.ashx?IDMF=03e0d869-dc7d-4195-a85a-c8e209f5b987
These components can be:
- Prescription for hearings aids on a trial basis
- Prescription of ear-level sound generators on a trial basis
- Prescription of a combination of instruments on a trial basis
- Prescription of a tabletop sound generator.
- Referral to a tinnitus support group.
- Referral to a psychologist for CBT and/or treatment of a depression, anxiety and/or stress problem.
- Referral to other health providers (family physician, ENT, physical therapist, etc.).
- Give written documentation to the patient about tinnitus.
- Information on Sound therapy.
- Desensitization program for hyperacusis.
8. Interventions
Counselling
All patients receive appropriate directive information on tinnitus including information on symptoms, possible causes, the emotional chain-reaction, the association with the limbic system and cues on how to manage and control the tinnitus. Patient is either given a more basic counselling or a more directive counselling based on Jastreboff classification: basic counselling is used for a score of 0 while for patients classified as 3 or more, a more directive counselling is offered.
The directive counselling includes all the following elements:
- What are the possible causes of his/her tinnitus?
- Hearing loss
- Hidden hearing loss
- Metabolic
- Medications
- Somatic (TMJ, neck)
- How tinnitus is generated in the central auditory system.
- The connection between the central auditory system, the limbic system, and the reaction of the patient to their tinnitus.
- The fight and flight reaction.
- The involvement of the sympathetic nervous system.
- The habituation processes.
- Benefits of cognitive behavioral therapy (CBT), relaxation, meditation, mindfulness meditation.
- The benefits of sound enrichment to reduce the perception of their tinnitus during the day.
- The benefits of sound therapy at night, including pillow speakers and noise generators, to reduce sleep disturbance caused by their tinnitus.
- The benefit of using a hearing aid if the patient has a hearing loss in combination with their tinnitus.
This directive counseling is done with the help of a PowerPoint presentation with all the information. We are presently in the process of creating a similar PowerPoint for the directive counseling for patients presenting only reduced sound tolerance symptoms. In addition, all the patients receive a folder containing information on tinnitus, masking strategies, list of noise generators application for iOS and Android and a list of purchase options for sleep pillow speakers.
Targeted Interventions
Hearing aids: When a patient presents a hearing loss, a hearing aid trial is recommended. During this trial, patients are given the choice to try the hearing aids with or without the tinnitus masker. If they choose the hearing aid with the masker, the noise is adjusted based either on the hearing loss or the tinnitus evaluation (pitch and level matching). If a patient does not present a hearing loss, the information on tinnitus masker within hearing aids is presented but not recommended as a first intervention.
Noise generator: Noise generators are recommended for patients having difficulty to fall asleep or to concentrate during the day because of their tinnitus (a list of free applications for iOS and Android phones for soothing sounds and a list of places to purchase pillow speakers are included in the information folder).
9. Reference to Other Healthcare Professional
Referrals: After analyzing the information gathered at the case history and questionnaires and the results of the evaluation, referral to other health professionals is determined. If cognitive-behavioural therapy (CBT) is recommended, a list of psychologists specialized in CBT is given to the patient. If the tinnitus is thought to be of a somatic nature, a list of physiotherapists specialized in somatic tinnitus and a list of dentists specialized in MTC joints is given. In the case of an ear asymmetry, conductive or mixed hearing loss, sudden hearing loss or other worrisome signs, patients are directly referred to an ENT.
We can also refer patients to:
- His/her family physician;
- A pharmacist for evaluation of the medications taken by the patient;
Follow-up: Depending on the components of the intervention plan and the severity of the tinnitus, patients are always followed-up by e-mail or with an appointment one month after the intervention. The objectives of the intervention plan are reviewed with them and, if necessary, modified according to their comments.
Conclusion
This program is a valuable addition to the University of Montreal's speech-language pathology and audiology clinic as it allows students to apply competency-based intervention with patients that have tinnitus and/or sound tolerance problem. Positive feedback has been received from patients suffering from tinnitus and/or sound tolerance problem. We hope that this protocol can motivate more clinicians to take in charge tinnitus and sound tolerance problem patients and help them create their own clinical protocol.
References
- Meikle MB, Henry JA, Griest SE, et al. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear 2012;33(2):153–76. doi:10.1097/AUD.0b013e31822f67c0
- Blasing L, Goebel G, Flotzinger U, et al. Hypersensitivity to sound in tinnitus patients: an analysis of a construct based on questionnaire and audiological data. Int J Audiol 2010; 49(7):518–26. doi:10.3109/14992021003724996
- Kroenke K, Spitzer RL, and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–13. doi:10.1046/j.1525-1497.2001.016009606.x
- Lowe B, Decker O, Muller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 2008;46(3):266–74. doi:10.1097/MLR.0b013e318160d093
- Bhatt JM, Bhattacharyya N, and Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope 2017;127(2):466–69. doi:10.1002/lary.26107
- Pattyn T, Van Den Eede F, Vanneste S, et al. Tinnitus and anxiety disorders: A review. Hear Res 2016;333:255–65. doi:10.1016/j.heares.2015.08.014
- IRDPQ. Guide clinique Prise en charge des usagers présentant des acouphènes avec une composante somatosensorielle. 2018. Retrieved from https://www.ciusss-capitalenationale.gouv.qc.ca/sites/default/files/guide_clinique-acouphene.pdf
- Jastreboff PJ and Jastreboff MM. Tinnitus Retraining Therapy (TRT) as a method for treatment of tinnitus and hyperacusis patients. J Am Acad Audiol 2000;11(3):162–77.
- Searchfield GD. A client oriented scale of improvement in tinnitus for therapy goal planning and assessing outcomes. J Am Acad Audiol 2019;30(4):327–37. doi:10.3766/jaaa.17119

