Toward Standardization of Tinnitus Services by Audiologists
Introduction
Approximately one in every 10–15 adults experiences chronic tinnitus.1,2 For most, the perception is fairly innocuous. For others, it is the trigger for sleep disruption, concentration difficulties, and emotional reactions.3 It is quite common for tinnitus sufferers to complain of the frustration and hopelessness that results from healthcare providers offering the standard bromide, “nothing can be done—learn to live with it.” We focus here on audiologists and their role in providing effective clinical services for their patients.
Every audiologist is aware that tinnitus is highly prevalent in their patient population. Hearing loss and tinnitus go hand in hand, and audiologists are accomplished in providing services to address hearing loss, but not necessarily tinnitus. In addition, many patients with tinnitus also report decreased sound tolerance (DST). Our premise is that audiologists, relative to all other healthcare providers, are in the best position to help patients with the three related conditions of hearing loss, tinnitus, and DST.
Although so many people are in need of clinical services for their tinnitus, very few healthcare providers have the knowledge and expertise to fill this role. Audiologists are ideally positioned to provide tinnitus clinical services because they are:
- Hearing aid experts, and they have expertise with sound-generating devices that can be used to alleviate effects of tinnitus.
- Trained and knowledgeable in anatomy, physiology, and pathology of the auditory system.
- Skilled in assessing hearing function, with these skills being adaptable to evaluate psychoacoustic attributes of tinnitus using existing equipment and facilities.
- Skilled in counseling patients regarding the auditory system and auditory rehabilitation.
- Affiliated with otolaryngologists, who are necessary to perform medical evaluations for underlying causes of tinnitus.
Consistent with these inherent qualifications for audiologists to serve as tinnitus-care providers, Audiology national organizations include tinnitus care in their scope of practice. It is therefore puzzling why most audiology graduate programs do not provide comprehensive training in tinnitus management. The net result is that audiologists are not prepared by their graduate education to become tinnitus practitioners. The purpose of this article is to argue for the necessity of audiologists to at least become competent in assessment of the tinnitus patient and to provide basic intervention for bothersome tinnitus through the use of hearing aids, sound-generating devices, and the provision of accurate tinnitus-care information to their patients.
Methods of both tinnitus assessment and intervention are numerous, and consensual standards do not exist to inform inter-clinic consistency in conducting these procedures. As a result, audiologists who provide tinnitus services vary greatly in how the services are delivered. In 2014, evidence-based tinnitus practice guidelines were published by the American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF).4 Two years later, it was concluded these guidelines were “followed infrequently” in the United States.2 Recently, specific procedures for basic tinnitus management by audiologists were recommended based on the AAO-HNSF guidelines and over two decades of tinnitus clinical research.5 The present article reviews those recommendations as an effort to promote greater uniformity amongst audiologists in their provision of tinnitus services.
Basic Audiologic Services for Tinnitus
The protocol described below is a brief overview of what has already been described in detail.5 Please refer to the figure for this section. The figure is an adaptation of the figure that appears in the original article,5 with some slight revisions. The following hyperlink provides access to the Tinnitus and Hearing Survey, Tinnitus Screener, and Tinnitus Functional Index: https://hearing.health.mil/For-Providers/Progressive-Tinnitus-Management/PTM-Provider-Resources/Tinnitus-Questionnaires
Initial Evaluation
In the figure, the box labeled “Initial Evaluation” contains three evaluation tasks that are considered essential, and two that are optional. The first two tasks are what any audiologist would normally do as part of a routine assessment: case history and audiologic evaluation. The case history should of course ask questions about any symptoms that would indicate the need for a medical evaluation by an otolaryngologist.6 The AAO-HNSF guidelines recommend that every patient complaining of tinnitus be evaluated by an otolaryngologist.4 If this is not feasible (which is often the case), then the audiologist must at least recognize symptoms that would suggest “secondary” tinnitus, such as tinnitus caused by some condition in the head or neck that produces an actual sound. Such conditions can be serious, and even life-threatening, so this is a critical concern.
The audiologic evaluation is routine, except for the caveat that many patients with tinnitus find acoustic reflex testing to be aversive. Such testing should therefore be done only if indicated by other test results. Tinnitus psychoacoustic testing is not normally recommended due to the inability to utilize the test results to inform clinical decision-making.7
The third “essential” task is to administer the Tinnitus and Hearing Survey (THS).8 The THS requires only about 5 minutes of additional time and is critical to clearly distinguish tinnitus-specific from hearing-specific problems. Patients often blame their hearing problems on their tinnitus9 and the THS was designed specifically to sort out this confusion. The THS also includes two items that screen for DST. The astute examiner can use the responses to these two items to reasonably surmise if a DST problem is related more to hyperacusis (loudness hypersensitivity) or misophonia (emotional/psychological reactions to certain sounds).10
It might be noted that a standard tinnitus questionnaire is not recommended as part of the initial evaluation. This is because patients who blame their tinnitus for their hearing problems will respond accordingly to questions about the impact of their tinnitus, inflating the severity score and giving the indication the tinnitus is a worse problem than it is. A standard questionnaire, however, is optional at this point. Clinicians might want more detailed information than is available from the THS about why the tinnitus is a problem for the patient. Tinnitus questionnaires, of which there are many, provide a comprehensive look at how and why the tinnitus is bothersome.11 The information derived can be useful for counseling purposes.
The Tinnitus Screener is also optional, and is used only if there is uncertainty about what the patient means by “I have tinnitus.” Assuming the patient’s symptoms are consistent with “primary” tinnitus, which is defined as “idiopathic and may or may not be associated with sensorineural hearing loss,”4 then it is important to know how long the patient has experienced tinnitus and the frequency of its occurrence. The Tinnitus Screener is a six-item algorithmic instrument that can be completed in less than 1 minute. Completing it will indicate if the patient’s tinnitus duration is persistent (i.e., chronic; ≥6 months) or recent-onset (i.e., acute; <6 months). It will also determine if the tinnitus frequency of occurrence is “constant,” “intermittent” (lasting at least 5 minutes and occurring at least daily or weekly), “occasional” (lasting at least 5 minutes and occurring less than weekly), or “temporary” (caused by some event and expected to resolve on its own). Constant or intermittent tinnitus would necessitate tinnitus clinical services, while occasional or temporary tinnitus would suggest educating the patient about hearing conservation and following up to monitor for any increase in symptoms.
Based on the initial evaluation, a decision is made as to whether the patient’s tinnitus is bothersome or non-bothersome. This decision relies on the THS, and is ultimately made by the patient. There is no threshold score on the THS that would distinguish between bothersome versus non-bothersome tinnitus, but rather the score for the Tinnitus Section A is compared to the score for the Hearing Section B. The scores are discussed with the patient, and the patient decides if further tinnitus services are needed. If not, then the patient’s tinnitus care is complete.
Addressing Bothersome Tinnitus
If it is determined the patient’s tinnitus is bothersome, then it is helpful to provide brief information about tinnitus and/or recommend a tinnitus general information class—if such a class is available. Essential information about tinnitus can be dispensed in various formats—brochures, handouts, apps, videos, books, etc., which will help to empower the patient to make informed decisions. It is especially important that they are aware of the evidence base for any intervention they may consider receiving. They should be informed of the AAO-HNSF guidelines, and a 2-page fact sheet is available for download that summarizes the AAO-HNSF recommendations: https://www.entnet.org/sites/default/files/sites/default/files/Oct2014_TinnitusGuidelineFactSheetFINAL_1.pdf.
Following the provision of basic tinnitus information, hearing aids are the next consideration. Audiologists may not be aware that hearing aids have considerable research support as “treatment” for tinnitus.12–15 This research has involved participants having both bothersome tinnitus and aidable hearing loss. Many audiologists, however, also fit hearing aids to people who would not be considered traditional hearing aid candidates—the primary reason being to treat the tinnitus.5 Hearing aids are available from all manufacturers with a built-in sound generator. Although these “combination instruments” have not been shown to be superior to amplification alone for treating tinnitus, they are preferred because they have the capability of delivering a customized acoustic signal if desired by the patient. Also, hearing aids with streaming capability are ideal for patients so they can listen to any sound from their smartphone as “sound therapy.”
If ear-level devices will not be used, then the next decision is whether tinnitus intervention is desired by the patient. If not, then the patient’s tinnitus care is complete. This decision relies on having a conversation with the patient to discuss results of the THS. The objective is to know if the patient desires intervention for the types of tinnitus problems listed in Section A of the THS.
Patients with bothersome tinnitus who do receive hearing aids or combination instruments should be evaluated again with the THS at least 1 month following their fitting date. As just described, the decision is whether intervention is desired for the types of problems described in Section A of the THS. If not, then the patient’s tinnitus care is complete. If intervention is desired, then a tinnitus general information class may be ideal, but is optional at this point. What is essential is to administer a tinnitus questionnaire prior to the intervention so as to obtain a pre-intervention baseline. Many questionnaires are available for this purpose.11 We recommend the TFI because it has been validated for being sensitive to changes in functional effects of tinnitus resulting from intervention.16 The audiologist might provide the intervention, or the patient will be referred for these specialized services. Either way, the TFI would be administered following intervention and the pre- and post-intervention TFI scores would be compared to determine outcomes of the intervention. On average, a 13-point or greater decrease in the TFI score would indicate a clinically significant reduction in tinnitus functional effects. Ultimately, however, it is the patient’s subjective report that determines whether the intervention has resulted in an improved quality of life. If the outcomes are satisfactory, then the patient’s tinnitus care is complete. If not, then further intervention is required and should be continued until the patient is satisfied that no further services are needed.
Audiologists who are motivated to provide tinnitus intervention have many options available to them. It is beyond the scope of this article to describe all the different possible interventions, but it should be noted that Cognitive-Behavioral Therapy (CBT) has the strongest research evidence according to the AAO-HNSF tinnitus practice guidelines.4 It is therefore important to collaborate with a mental health provider who can deliver CBT. Otherwise, audiologists have many options for delivering sound therapy via different modalities.17 It is recommended that hearing aids or combination instruments be tried first, followed by self-help education so that patients can learn what to do to help themselves whenever their tinnitus is problematic. Free or very inexpensive apps are available that can also be helpful.18 Expensive sound-therapy options should be considered as the last resort, and only if supported by controlled research and affordable by the patient.
Summary
Tinnitus clinical services have not been standardized, leaving patients at risk of receiving unvalidated, ineffective, and needlessly expensive tinnitus care. This article is intended to promote standardization of these services by describing an efficient and research-based clinical protocol for audiologists. The protocol includes a case history, appropriate referral, audiologic assessment, use of the Tinnitus and Hearing Survey, brief tinnitus information or tinnitus information class, hearing aids or combination instruments as warranted, follow-up assessment, and criteria for determining if further tinnitus-specific services are needed. Use of this protocol can help to promote standardization of tinnitus practice by audiologists. It should be apparent that people with bothersome tinnitus represent a relatively untapped market for many audiologists.
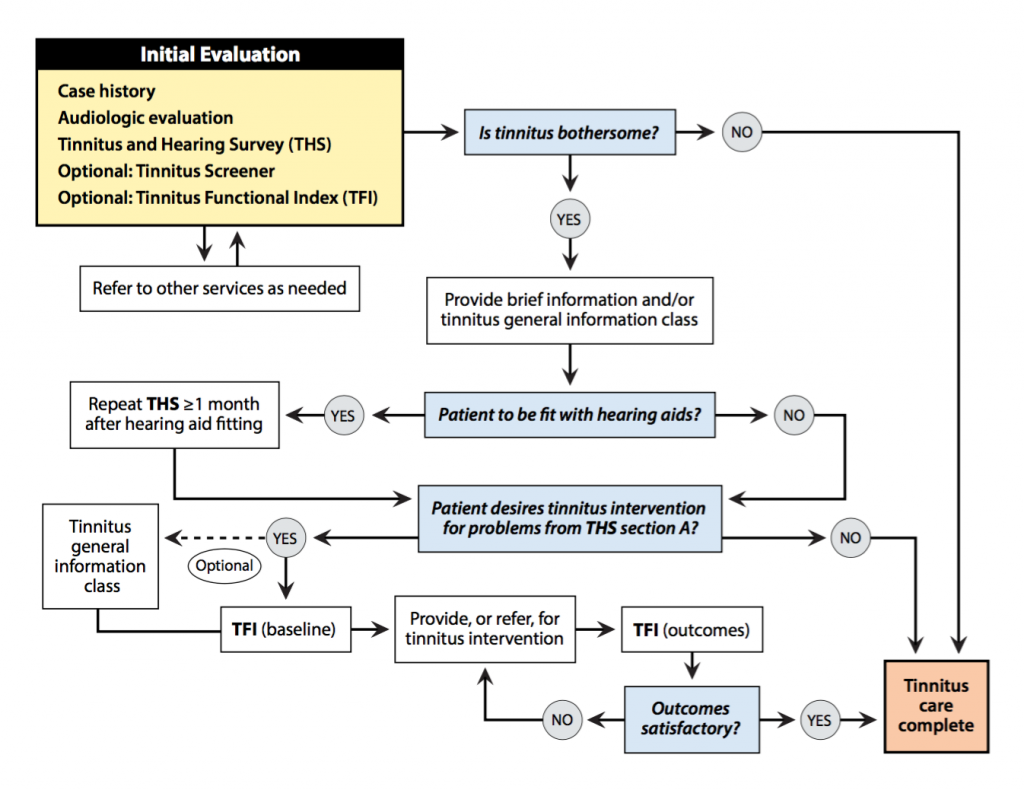
Figure 1. This decision-tree flowchart (created by Lynn Kitagawa, MFA, Medical Media, VA Portland Health Care System) shows the different steps that are recommended by the present authors for the provision of basic tinnitus services by audiologists. It is adapted, with permission, from a similar figure previously published.5
References
- Hoffman HJ, Reed GW. Epidemiology of tinnitus. In: Snow JB, ed. Tinnitus: Theory and Management. Lewiston, NY: BC Decker Inc.; 2004: 16-41.
- Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, Severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg Oct 1 2016;142(10):959–65.
- Henry JA, Dennis K, Schechter MA. General review of tinnitus: Prevalence, mechanisms, effects, and management. Journal of Speech, Language, and Hear Res 2005;48(5):1204–34.
- Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg Oct 2014;151(2 Suppl):S1–S40.
- Henry JA, Manning C. Clinical protocol to promote standardization of basic tinnitus services by audiologists. Am J Audiol Apr 22 2019;28(1S):152–61.
- Henry JA, Zaugg TL, Myers PJ, Kendall CJ, Michaelides EM. A triage guide for tinnitus. J Fam Pract Jul 2010;59(7):389–93.
- Henry JA. Measurement of tinnitus. Otol Neurotol Sep 2016;37(8):e276–85.
- Henry JA, Griest S, Zaugg TL, et al. Tinnitus and hearing survey: a screening tool to differentiate bothersome tinnitus from hearing difficulties. Am J Audiol Mar 2015;24(1):66–77.
- Ratnayake SA, Jayarajan V, Bartlett J. Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus? Noise Health Jul-Sep 2009;11(44):156–60.
- Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. New York: Cambridge University Press; 2004.
- Newman CW, Sandridge SA, Jacobson GP. Assessing outcomes of tinnitus intervention. J Am Acad Audiol Jan 2014;25(1):76–105.
- Shekhawat GS, Searchfield GD, Stinear CM. Role of hearing AIDS in tinnitus intervention: a scoping review. J Am Acad Audiol Sep 2013;24(8):747–62.
- Henry JA, Frederick M, Sell S, Griest S, Abrams H. Validation of a novel combination hearing aid and tinnitus therapy device. Ear Hear Jan 2015;36(1):42–52.
- Henry JA, McMillan G, Dann S, et al. Tinnitus management: randomized controlled trial comparing extended-wear hearing aids, conventional hearing aids, and combination instruments. J Am Acad Audiol Jun 2017;28(6):546–61.
- dos Santos GM, Bento RF, de Medeiros IR, Oiticcica J, da Silva EC, Penteado S. The influence of sound generator associated with conventional amplification for tinnitus control: randomized blind clinical trial. Trends Hear. 2014;18.
- Meikle MB, Henry JA, Griest SE, et al. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear Mar-Apr 2012;33(2):153–76.
- Hoare DJ, Searchfield GD, El Refaie A, Henry JA. Sound therapy for tinnitus management: practicable options. J Am Acad Audiol Jan 2014;25(1):62–75.
- Skarzynski PH, Kutyba J, Cywka K, Sztabnicka A. Effects of Using the ReSound Relief Application in Therapy of Tinnitus. American Academy of Audiology Annual Convention. Nashville, TN; 2019.

